Abstract
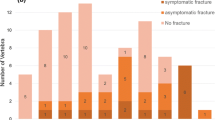
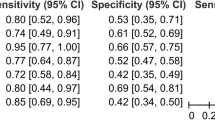
Mechanical instability secondary to vertebral metastases can lead to pathologic vertebral compression fracture (VCF) mechanical pain, neurological compromise, and the need for surgical stabilization. Stereotactic body radiation therapy (SBRT) as a treatment for spinal metastases is effective for pain and local tumor control, it has been associated with an increased risk of VCF. This study quantified computed tomography (CT) based stability measures in metastatic vertebrae with VCF treated with spine SBRT. It was hypothesized that semi-automated quantification of VCF based on CT metrics would be related to clinical outcomes. 128 SBRT treated spinal metastases patients were identified from a prospective database. Of these, 18 vertebral segments were identified with a VCF post-SBRT. A semi-automated system for quantifying VCF was developed based on CT imaging before and after SBRT. The system identified and segmented SBRT treated vertebral bodies, calculated stability metrics at single time points and changes over time. In the vertebrae that developed a new (n = 7) or progressive (n = 11) VCF following SBRT, the median time to VCF/VCF progression was 1.74 months (range 0.53–7.79 months). Fractured thoracolumbar vertebrae that went on to be stabilized (cemented and/or instrumented), had greater fractured vertebral body volume progression over time (12%) compared to those not stabilized (0.4%, p < 0.05). Neither the spinal instability neoplastic score (SINS) or any single timepoint stability metrics in post-hoc analyses correlated with future stabilization. This pilot study presents a quantitative semi-automated method assessing fractured thoracolumbar vertebrae based on CT. Increased fractured vertebral body volume progression post-SBRT was shown to predict those patients who were subsequently stabilized, motivating study of methods that assess temporal radiological changes toward augmenting existing clinical management in the metastatic spine.


Similar content being viewed by others
Abbreviations
- CT:
-
Computed tomography
- SBRT:
-
Stereotactic body radiation therapy
- QOL:
-
Quality-of-life
- VCF:
-
Vertebral compression fracture
- CTV:
-
Clinical target volume
- MRI:
-
Magnetic resonance imaging
- SINS:
-
Spinal instability neoplastic score
- TLICS:
-
Thoracolumbar injury classification and severity score
- DSC:
-
Dice similarity coefficients
- CI:
-
Confidence interval
- NTCP:
-
Normal tissue complication probability
- VuFx-Fx :
-
Fractured vertebral body volume loss calculated at 1 timepoint
- VFx∆t :
-
Fractured vertebral body volume loss progression
- HuFx-Fx :
-
Fractured vertebral body height loss calculated at 1 timepoint
- HFx∆t :
-
Fractured vertebral body height loss progression
- AP:
-
Fractured anterior–posterior
- HAPasym :
-
Fractured vertebral body height asymmetry
- HLRasym :
-
Fractured left–right vertebral body asymmetry
- HAP_asym_∆t :
-
Fractured anterior–posterior vertebral body height asymmetry progression
- HLR_asym_∆t :
-
Fractured left–right vertebral body height asymmetry progression
References
Wong DA, Fornasier VL, MacNab I (1990) Spinal metastases: the obvious, the occult, and the impostors. Spine (Phila Pa 1976) 15:1–4
Harrington K (1988) Mechanisms of metastases. In: Harrington K (ed) Diagnosis and treatment of metastatic bone disease. Mosby, St Louis MO, pp 15–31
Toma S, Venturino A, Sogno G et al (1993) Metastatic bone tumors: nonsurgical treatment. Outcome and survival. Clin Orthop Relat Res 295:246–251
Houston SJ, Rubens RD (1995) The systemic treatment of bone metastases. Clin Orthop Relat Res 312:95–104
Shinoda Y, Sawada R, Yoshikawa F et al (2019) Factors related to the quality of life in patients with bone metastases. Clin Exp Metastasis 36:441–448. https://doi.org/10.1007/s10585-019-09983-0
Hill ME, Richards MA, Gregory WM et al (1993) Spinal cord compression in breast cancer: a review of 70 cases. Br J Cancer 68:969–973
Burke MV, Atkins A, Akens M et al (2016) Osteolytic and mixed cancer metastasis modulates collagen and mineral parameters within rat vertebral bone matrix. J Orthop Res 34:2126–2136. https://doi.org/10.1002/jor.23248
Burke M, Atkins A, Kiss A et al (2017) The impact of metastasis on the mineral phase of vertebral bone tissue. J Mech Behav Biomed Mater 69:75–84. https://doi.org/10.1016/j.jmbbm.2016.12.017
Kitagawa Y, Kim Y, Tsunoda R, Takai S (2020) Types of pedicle signs indicating symptomatic spinal metastases and their associated clinical and radiological features. J Nippon Med Sch. https://doi.org/10.1272/jnms.JNMS.2021_88-101
Zeng L, Chow E, Bedard G et al (2012) Quality of life after palliative radiation therapy for patients with painful bone metastases: results of an international study validating the EORTC QLQ-BM22. Int J Radiat Oncol Biol Phys 84:e337–e342. https://doi.org/10.1016/j.ijrobp.2012.05.028
Ibrahim A, Crockard A, Antonietti P et al (2008) Does spinal surgery improve the quality of life for those with extradural (spinal) osseous metastases? An international multicenter prospective observational study of 223 patients. J Neurosurg Spine 8:271–278. https://doi.org/10.3171/SPI/2008/8/3/271
Lutz S, Berk L, Chang E (2011) Palliative radiotherapy for bone metastases: an ASTRO evidence based guideline. Int J Radiat Oncol Bio Phys 79:965–976
Wardak Z, Bland R, Ahn C et al (2019) A phase 2 clinical trial of SABR followed by immediate vertebroplasty for spine metastases. Int J Radiat Oncol Biol Phys 104:83–89. https://doi.org/10.1016/j.ijrobp.2019.01.072
Carbonneau A, Sahgal A, Masucci GL (2018) Spinal stereotactic body radiotherapy. adult CNS radiation oncology. Springer, Cham, pp 687–707
Sprave T, Verma V, Förster R et al (2018) Randomized phase II trial evaluating pain response in patients with spinal metastases following stereotactic body radiotherapy versus three-dimensional conformal radiotherapy. Radiother Oncol 128:274–282. https://doi.org/10.1016/j.radonc.2018.04.030
Sprave T, Verma V, Förster R et al (2018) Local response and pathologic fractures following stereotactic body radiotherapy versus three-dimensional conformal radiotherapy for spinal metastases: a randomized controlled trial. BMC Cancer 18:859. https://doi.org/10.1186/s12885-018-4777-8
Tseng C-L, Soliman H, Myrehaug S et al (2018) Imaging-based outcomes for 24 Gy in 2 daily fractions for patients with de novo spinal metastases treated with spine stereotactic body radiation therapy (SBRT). Int J Radiat Oncol 102:499–507. https://doi.org/10.1016/j.ijrobp.2018.06.047
Cox BW, Spratt DE, Lovelock M et al (2012) International spine radiosurgery consortium consensus guidelines for target volume definition in spinal stereotactic radiosurgery. Int J Radiat Oncol 83:e597–e605. https://doi.org/10.1016/j.ijrobp.2012.03.009
Steverink JG, Willems SM, Philippens MEP et al (2018) Early tissue effects of stereotactic body radiation therapy for spinal metastases. Int J Radiat Oncol 100:1254–1258. https://doi.org/10.1016/j.ijrobp.2018.01.005
Al-Omair A, Smith R, Kiehl T-R et al (2013) Radiation-induced vertebral compression fracture following spine stereotactic radiosurgery: clinicopathological correlation. J Neurosurg Spine 18:430–435. https://doi.org/10.3171/2013.2.SPINE12739
Barth HD, Launey ME, Macdowell AA et al (2010) On the effect of X-ray irradiation on the deformation and fracture behavior of human cortical bone. Bone 46:1475–1485. https://doi.org/10.1016/j.bone.2010.02.025
Cunha MV, Al-Omair A, Atenafu EG et al (2012) Vertebral compression fracture (VCF) after spine stereotactic body radiation therapy (SBRT): analysis of predictive factors. Int J Radiat Oncol Biol Phys 84:e343–e349
Boehling NS, Grosshans DR, Allen PK et al (2012) Vertebral compression fracture risk after stereotactic body radiotherapy for spinal metastases. J Neurosurg Spine 16:379–386. https://doi.org/10.3171/2011.11.SPINE116
Rose PS, Laufer I, Boland PJ et al (2009) Risk of fracture after single fraction image-guided intensity-modulated radiation therapy to spinal metastases. J Clin Oncol 27:5075–5079. https://doi.org/10.1200/JCO.2008.19.3508
Sahgal A, Atenafu EG, Chao S et al (2013) Vertebral compression fracture after spine stereotactic body radiotherapy: a multi-institutional analysis with a focus on radiation dose and the spinal instability neoplastic score. J Clin Oncol 31:3426–3431. https://doi.org/10.1200/JCO.2013.50.1411
Fisher CG, DiPaola CP, Ryken TC et al (2010) A novel classification system for spinal instability in neoplastic disease. Spine (Phila Pa) 35:E1221–E1229. https://doi.org/10.1097/BRS.0b013e3181e16ae2
Joaquim AF, Fernandes YB, Cavalcante RAC et al (2011) Evaluation of the thoracolumbar injury classification system in thoracic and lumbar spinal trauma. Spine (Phila Pa 1976) 36:33–36. https://doi.org/10.1097/BRS.0b013e3181c95047
Fourney DR, Frangou EM, Ryken TC et al (2011) Spinal instability neoplastic score: an analysis of reliability and validity from the spine Oncology Study Group. J Clin Oncol 29:3072–3077. https://doi.org/10.1200/JCO.2010.34.3897
Versteeg AL, Verlaan JJ, Sahgal A et al (2016) The spinal instability neoplastic score: impact on oncologic decision-making. Spine (Phila Pa 1976) 41:S231–S237
Thibault I, Whyne CM, Zhou S et al (2017) Volume of lytic vertebral body metastatic disease quantified using computed tomography-based image segmentation predicts fracture risk after spine stereotactic body radiation therapy. Int J Radiat Oncol Biol Phys 97:75–81. https://doi.org/10.1016/j.ijrobp.2016.09.029
Whyne CM, Hardisty MR (2010) Quantification of metastatic burden in the spine and its structural implications. Bone Brain Metastases Adv Res Treat 4:271–288
Kaloostian PE, Yurter A, Zadnik PL et al (2014) Current paradigms for metastatic spinal disease: an evidence-based review. Ann Surg Oncol 10:248–262. https://doi.org/10.1245/s10434-013-3324-8
Amir E, Whyne C, Freedman OC et al (2009) Radiological changes following second-line zoledronic acid treatment in breast cancer patients with bone metastases. Clin Exp Metastasis 26:479–484. https://doi.org/10.1007/s10585-009-9247-x
Snyder BD, Cordio MA, Nazarian A et al (2009) Noninvasive prediction of fracture risk in patients with metastatic cancer to the spine. Clin Cancer Res 15:7676–7683. https://doi.org/10.1158/1078-0432.CCR-09-0420
Whealan KM, Kwak SD, Tedrow JR et al (2000) Noninvasive imaging predicts failure load of the spine with simulated osteolytic defects. J Bone Jt Surg Am 82:1240–1251
Kaneko TS, Bell JS, Pejcic MR et al (2004) Mechanical properties, density and quantitative CT scan data of trabecular bone with and without metastases. J Biomech 37:523–530
Bagni B, Scutellari PN, Orzincolo C et al (1990) Quantitative analysis of bone density in multiple myeloma. Radiol Med 80:432–440
Chiu N, Probyn L, Raman S et al (2016) Radiological changes on CT after stereotactic body radiation therapy to non-spine bone metastases: a descriptive series. Ann Palliat Med 5:116–124. https://doi.org/10.21037/apm.2016.03.01
Hardisty M, Gordon L, Agarwal P et al (2007) Quantitative characterization of metastatic disease in the spine. Part I. Semiautomated segmentation using atlas-based deformable registration and the level set method. Med Phys 34:3127–3134. https://doi.org/10.1118/1.2746498
Tseng CL, Campbell M, Soliman H et al (2017) Imaging-based outcomes for 24 Gy in 2 daily fractions for patients with de novo spinal metastases treated with spine stereotactic body radiation therapy: an emerging standard. Int J Radiat Oncol 99:S158. https://doi.org/10.1016/j.ijrobp.2017.06.364
Sahgal A, Whyne CM, Ma L et al (2013) Vertebral compression fracture after stereotactic body radiotherapy for spinal metastases. Lancet Oncol 14:e310–e320. https://doi.org/10.1016/S1470-2045(13)70101-3
Germano IM, Carai A, Pawha P et al (2016) Clinical outcome of vertebral compression fracture after single fraction spine radiosurgery for spinal metastases. Clin Exp Metastasis 33:143–149. https://doi.org/10.1007/s10585-015-9764-8
Roberts MG, Cootes TF, Pacheco E, et al (2009) Segmentation of lumbar vertebrae using part-based graphs and active appearance models. In: Lecture notes in computer science (including subseries Lecture Notes in Artificial Intelligence and Lecture Notes in Bioinformatics). pp 1017–1024
Whyne C, Hardisty M, Wu F et al (2007) Quantitative characterization of metastatic disease in the spine. Part II. Histogram-based analyses. Med Phys 34:3279–3285
Chen H, Shen C, Qin J, et al (2015) Automatic localization and identification of vertebrae in spine CT via a joint learning model with deep neural networks. In: Lecture notes in computer science (including subseries Lecture Notes in Artificial Intelligence and Lecture Notes in Bioinformatics). pp 515–522
Czyz M, Eyvazov K, Radwan H, Boszczyk BM (2016) Lumbar spine computed tomography (CT)-based fractal analysis may help in detecting decreased quality of bone prior to urgent spinal procedures (novel technique). Spine J 16:S46. https://doi.org/10.1016/j.spinee.2016.01.029
Redmond J, Friedl KE, Cornett P et al (1988) Clinical usefulness of an algorithm for the early diagnosis of spinal metastatic disease. J Clin Oncol 6:154–157
Yao J, Burns JE, Wiese T, Summers RM (2012) Quantitative vertebral compression fracture evaluation using a height compass. In: SPIE Medical Imaging Conference. p 83151X
Guglielmi G, Palmieri F, Placentino MG et al (2009) Assessment of osteoporotic vertebral fractures using specialized workflow software for 6-point morphometry. Eur J Radiol 70:142–148. https://doi.org/10.1016/j.ejrad.2007.12.001
Bjørnerem Å, Bui QM, Ghasem-Zadeh A et al (2013) Fracture risk and height: an association partly accounted for by cortical porosity of relatively thinner cortices. J Bone Miner Res 28:2017–2026. https://doi.org/10.1002/jbmr.1934
Armstrong MEG, Kirichek O, Cairns BJ et al (2016) Relationship of height to site-specific fracture risk in postmenopausal women. J Bone Miner Res 31:725–731. https://doi.org/10.1002/jbmr.2742
Horger M, Ditt H, Liao S et al (2017) Automated “bone subtraction” image analysis software package for improved and faster CT monitoring of longitudinal spine involvement in patients with multiple myeloma. Acad Radiol 24:623–632. https://doi.org/10.1016/j.acra.2016.12.003
Al Arif SMMR, Knapp K, Slabaugh G (2017) Shape-aware deep convolutional neural network for vertebrae segmentation. In: MICCAI’2017 MSK workshop. pp 12–23
Korez R, Parent S, Kadoury S, et al (2017) 3D Cobb angle measurements from scoliotic mesh models with varying face-vertex density. In: MICCAI’2017 MSK workshop. pp 46–55
Sekuboyina A, Kukaˇ J (2017) Attention-driven deep learning for pathological spine segmentation. In: MICCAI’2017 MSK workshop. pp 104–115
Leung J, Hardisty M, Martel A, et al (2018) Convolutional neural networks for vertebral body segmentation in CT images. In: Orthopaedic research society, pp PS1–052
Verlaan JJ, Diekerhof CH, Buskens E et al (2004) Surgical treatment of traumatic fractures of the thoracic and lumbar spine a systematic review of the literature on techniques. Complications, and Outcome 29:803–814
Verlaan JJ, Diekerhof CH, Buskens E et al (2004) Surgical treatment of traumatic fractures of the thoracic and lumbar spine. Spine (Phila Pa 1976) 29:803–814. https://doi.org/10.1097/01.BRS.0000116990.31984.A9
Marks LB, Yorke ED, Jackson A et al (2010) Use of normal tissue complication probability models in the clinic. Int J Radiat Oncol 76:S10–S19. https://doi.org/10.1016/j.ijrobp.2009.07.1754
Faruqi S, Tseng CL, Whyne C et al (2018) Vertebral compression fracture after spine stereotactic body radiation therapy: a review of the pathophysiology and risk factors. Clin Neurosurg 83:314–322. https://doi.org/10.1093/neuros/nyx493
Acknowledgements
Funding by FED DEV Ontario with matching funds from Lexmark International.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hardisty, M., Wright, T., Campbell, M. et al. CT based quantitative measures of the stability of fractured metastatically involved vertebrae treated with spine stereotactic body radiotherapy. Clin Exp Metastasis 37, 575–584 (2020). https://doi.org/10.1007/s10585-020-10049-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10585-020-10049-9