Abstract
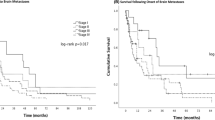
Patients with small cell lung cancer (SCLC) are more likely to have synchronous brain metastasis (SBM) at the time of diagnosis than patients with any other extracranial primary malignancy. We sought to identify which factors predicted an increased risk of SBM in SCLC as well as which factors affected the prognosis of these patients. 38,956 Patients in the Surveillance, Epidemiology, and End Results (SEER) database with microscopically confirmed SCLC from 2010 to 2016 were identified. 6264 (16.1%) Patients with SCLC had SBM at the time of diagnosis. In the multivariable logistic regression, disease specific factors that were predictive of SBM were primary tumor size > 7 cm (adjusted OR = 1.14, 95% CI [1.02, 1.28], p = 0.02), synchronous lung metastases, and synchronous bone metastases. Demographic specific factors predictive of increased SBM risk in this model were younger age, male sex, and race (American Indian/Alaska Native and black patients). Patients insured through Medicaid were less likely to present with SBM. In the multivariate Cox proportional hazards model, lack of insurance was the strongest predictor of mortality (adjusted HR = 1.47, 95% CI [1.26, 1.73], p < 0.001). Other factors associated with an increased risk of mortality include male sex, older age, health insurance coverage through Medicaid, synchronous liver metastasis, synchronous lung metastasis, and primary tumor size > 7 cm. In contrast, Asian patients had a lower risk of mortality. This study identifies risk factors for SBM among patients with SCLC, as well as indicators of prognosis among this patient population.




Similar content being viewed by others
Data availability
SEER Incidence Data is available at https://seer.cancer.gov/data/.
References
Johnson JD, Young B (1996) Demographics of brain metastasis. Neurosurg Clin N Am 7(3):337–344
Nayak L, Lee EQ, Wen PY (2012) Epidemiology of brain metastases. Curr Oncol Rep 14(1):48–54
Hirsch FR et al (1982) Intracranial metastases in small cell carcinoma of the lung: correlation of clinical and autopsy findings. Cancer 50(11):2433–2437
Govindan R et al (2006) Changing epidemiology of small-cell lung cancer in the United States over the last 30 years: analysis of the surveillance, epidemiologic, and end results database. J Clin Oncol 24(28):4539–4544
Altan M, Chiang AC (2015) Management of small cell lung cancer: progress and updates. Cancer J 21(5):425–433
Zheng Y et al (2018) Risk factors for brain metastasis in patients with small cell lung cancer without prophylactic cranial irradiation. Strahlenther Onkol 194(12):1152–1162
Auperin A et al (1999) Prophylactic cranial irradiation for patients with small-cell lung cancer in complete remission. Prophylactic Cranial Irradiation Overview Collaborative Group. N Engl J Med 341(7):476–484
Meert AP et al (2001) Prophylactic cranial irradiation in small cell lung cancer: a systematic review of the literature with meta-analysis. BMC Cancer 1:5
Slotman B et al (2007) Prophylactic cranial irradiation in extensive small-cell lung cancer. N Engl J Med 357(7):664–672
Takahashi T et al (2017) Prophylactic cranial irradiation versus observation in patients with extensive-disease small-cell lung cancer: a multicentre, randomised, open-label, phase 3 trial. Lancet Oncol 18(5):663–671
Schild SE et al (2017) Prophylactic cranial irradiation for extensive small-cell lung cancer. J Oncol Pract 13(11):732–738
Lukas RV et al (2017) State-of-the-art considerations in small cell lung cancer brain metastases. Oncotarget 8(41):71223–71233
Robin TP et al (2018) Radiosurgery alone is associated with favorable outcomes for brain metastases from small-cell lung cancer. Lung Cancer 120:88–90
Bernhardt D et al (2018) Whole brain radiation therapy alone versus radiosurgery for patients with 1–10 brain metastases from small cell lung cancer (ENCEPHALON Trial): study protocol for a randomized controlled trial. Trials 19(1):388
Kromer C et al (2017) Estimating the annual frequency of synchronous brain metastasis in the United States 2010–2013: a population-based study. J Neurooncol 134(1):55–64
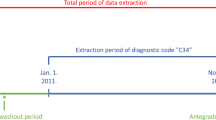
Surveillance, Epidemiology, and End Results (SEER) Program research data (1975–2016). National Cancer Institute, DCCPS, Surveillance Research Program. https://www.seer.cancer.gov (released April 2019, based on the November 2018 submission). Accessed 13 Jan 2020
Lekic M et al (2012) Outcome of small cell lung cancer (SCLC) patients with brain metastases in a routine clinical setting. Radiol Oncol 46(1):54–59
Nakazawa K et al (2012) Specific organ metastases and survival in small cell lung cancer. Oncol Lett 4(4):617–620
Hardy J et al (1990) The value of computed tomographic (CT) scan surveillance in the detection and management of brain metastases in patients with small cell lung cancer. Br J Cancer 62(4):684–686
Waqar SN et al (2018) Brain metastases at presentation in patients with non-small cell lung cancer. Am J Clin Oncol 41(1):36–40
Saber A et al (2017) Mutation patterns in small cell and non-small cell lung cancer patients suggest a different level of heterogeneity between primary and metastatic tumors. Carcinogenesis 38(2):144–151
Rosato A et al (2013) Survivin expression impacts prognostically on NSCLC but not SCLC. Lung Cancer 79(2):180–186
Ren Y et al (2016) Prognostic effect of liver metastasis in lung cancer patients with distant metastasis. Oncotarget 7(33):53245–53253
Pezzi TA et al (2018) Barriers to combined-modality therapy for limited-stage small cell lung cancer. JAMA Oncol 4(8):e174504
Xiao HF et al (2017) Development and validation of two prognostic nomograms for predicting survival in patients with non-small cell and small cell lung cancer. Oncotarget 8(38):64303–64316
Goncalves PH et al (2016) Risk of brain metastases in patients with nonmetastatic lung cancer: analysis of the Metropolitan Detroit Surveillance, Epidemiology, and End Results (SEER) data. Cancer 122(12):1921–1927
Wang S et al (2018) Development and validation of a nomogram prognostic model for SCLC patients. J Thorac Oncol 13(9):1338–1348
Wang L et al (2018) Tumor size and lymph node metastasis are prognostic markers of small cell lung cancer in a Chinese population. Medicine (Baltim) 97(31):e11712
Li B et al (2013) Elevated PLGF contributes to small-cell lung cancer brain metastasis. Oncogene 32(24):2952–2962
Liu T et al (2015) Visfatin mediates SCLC cells migration across brain endothelial cells through upregulation of CCL2. Int J Mol Sci 16(5):11439–11451
Xu ZH et al (2019) Brain microvascular endothelial cell exosome-mediated S100A16 up-regulation confers small-cell lung cancer cell survival in brain. FASEB J 33(2):1742–1757
Steindl A et al (2019) Prognostic assessment in patients with newly diagnosed small cell lung cancer brain metastases: results from a real-life cohort. J Neurooncol 145(1):85–95
Noone AM et al (2016) Comparison of SEER treatment data with Medicare claims. Med Care 54(9):e55–e64
Funding
SEER is supported by the Surveillance Research Program in the National Cancer Institute’s Division of Cancer Control and Population Sciences.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors have no conflicts of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
10585_2020_10040_MOESM1_ESM.png
Supplementary file2 (PNG 78 kb) Supplemental Fig. 1 Insurance status based on race among all patients diagnosed with SCLC
10585_2020_10040_MOESM2_ESM.tiff
Supplementary file2 (TIFF 10549 kb) Supplemental Fig. 2 Survival curves comparing patients with SCLC with SBM based on the presence of insurance status for younger than 65 years of age (n = 2095, number of events = 1812, p < 0.0001, log-rank test)
Rights and permissions
About this article
Cite this article
Reddy, S.P., Dowell, J.E. & Pan, E. Predictors of prognosis of synchronous brain metastases in small-cell lung cancer patients. Clin Exp Metastasis 37, 531–539 (2020). https://doi.org/10.1007/s10585-020-10040-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10585-020-10040-4