Abstract
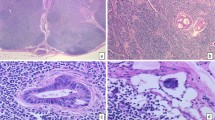
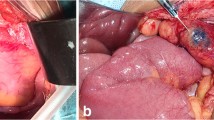
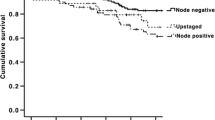
All colon cancer patients with lymph node (LN) positive disease are treated with chemotherapy. Patients with node negative disease are usually cured by surgery alone. Yet about 20% of patients develop recurrence within 5 years despite node negative status. This may often be the result of missed micrometastases by conventional examination. Sentinel lymph node (SLN) mapping was developed to find those nodes detected by blue dye which was ultrastaged to detect micrometastases. Consecutive patients, underwent SLN mapping with the blue dye with success rate of 99.2%. Average number of LN was 18.3, average number of SLN was 3/patient and overall nodal positivity was 45%. Ten patients had skip metastases. Overall survival of 235 patients was 84 months with survival of node negative patients 97 months versus 68 months for node positive patients. For stage I–IV patients, overall survival was as follows: stage I—115 months, stage II—90 months, stage III—84 months and stage IV—24 months respectively. Patients with micrometastases after chemotherapy had average survival of 108 months versus those without chemotherapy was 50 months. Thus, SLN mapping techniques is highly successful, easily reproducible and finds micrmoetastases in over 15% of patients which could have been missed by conventional pathological examination. These patients when treated with adjuvant chemotherapy have similar survival as those of node negative disease. Similarly, patients without any nodal metastases after SLN mapping and ultrastaging, may be considered as true node negative disease and may avoid further adjuvant chemotherapy.
Similar content being viewed by others
References
Golobocan 2012
Weixler B, Warschkow R, Güller U et al (2016) Isolated tumor cells in stage I & II colon cancer patients are associated with significantly worse disease-free and overall survival. BMC Cancer. https://doi.org/10.1186/s12885-016-2130-7
Protic M, Stojadinovic A, Nissan A et al (2015) Prognostic effect of ultra-staging node-negative colon cancer without adjuvant chemotherapy: a Prospective National Cancer Institute-Sponsored Clinical Trial. J Am Coll Surg 221(3):643–651. https://doi.org/10.1016/j.jamcollsurg.2015.05.007 quiz 783–785.
Yun HR, Kim HC, Lee WY et al (2009) The necessity of chemotherapy in T3N0M0 colon cancer without risk factors. Am J Surg 198(3):354–358. https://doi.org/10.1016/j.amjsurg.2008.09.027
Nelson H, Petrelli N, Carlin A et al (2001) National Cancer Institute Expert Panel. Guidelines 2000 for colon and rectal cancer surgery. J Natl Cancer Inst 93(8):583–596
Van der Zaag ES, Bouma WH, Tanis PJ et al (2012) Systematic review of sentinel lymph node mapping procedure in colorectal cancer. Ann Surg Oncol 19(11):3449–3459. https://doi.org/10.1245/s10434-012-2417-0
Mescoli C, Albertoni L, Pucciarelli S et al (2012) Isolated tumor cells in regional lymph nodes as relapse predictors in stage I and II colorectal cancer. J Clin Oncol 30(9):965–971. https://doi.org/10.1200/JCO.2011.35.9539
Jin M, Frankel WL (2018) Lymph node metastasis in colorectal cancer. Surg Oncol Clin N Am 27(2):401–412. https://doi.org/10.1016/j.soc.2017.11.011
Nicastri DG, Doucette JT, Godfrey TE et al (2007) Is occult lymph node disease in colorectal cancer patients clinically significant? A review of the relevant literature. J Mol Diagn 9(5):563–571
Pickren JW (1961) Significance of occult metastases (1961) A study of breast cancer. Cancer 14:1266–1271
Turner RR, Ollila DW, Stern S, Giuliano AE (1999) Optimal histopathologic examination of the sentinel lymph node for breast carcinoma staging. Am J Surg Pathol 23(3):263–267
Greenson JK, Isenhart CE, Rice R et al (1994) Identification of occult micrometastases in pericolic lymph nodes of Duke’s B colorectal cancer patients using monoclonal antibodies against cytokeratin and CC49. Correlation with long-term survival. Cancer 73(3):563–569
Sirop S, Kanaan M, Korant A et al (2011) Detection and prognostic impact of micrometastasis in colorectal cancer. J Surg Oncol 103(6):534–537
Saha S, Wiese D, Badin J et al (2000) Technical details of sentinel lymph node mapping in colorectal cancer and its impact on staging. Ann Surg Oncol 7(2):120–124
Compton CC, Fielding LP, Burgart LJ et al (2000) Prognostic factors in colorectal cancer. Arch Pathol Lab Med 124(7):979–994
Goldstein NS (2002) Lymph node recoveries from 2427 pT3 colorectal resection specimens spanning 45 years. Recommendations for a minimum number of recovered lymph nodes based on predictive probabilities. Am J Surg Path 26:179–189
Wiese DA, Saha S, Badin J et al (2000) Pathologic evaluation of sentinel lymph nodes in colorectal carcinoma. Arch Pathol Lab Med 124(12):1759–1763
Rakislova N et al (2017) Lymph node pooling: a feasible and efficient method of lymph node molecular staging in colorectal carcinoma. Transl Med 15:14
Saha S, Johnston G, Korant A et al (2013) Aberrant drainage of sentinel lymph nodes in colon cancer and its impact on staging and extent of operation. Am J Surg 205(3):302–306
Wiese D, Sirop S, Yestrepsky B et al (2010) Ultrastaging of sentinel lymph nodes (SLNs) vs. non-SLNs in colorectal cancer—do we need both? Am J Surg 199(3):354–358
Wiese D, Saha S, Yestrepsky B et al (2009) A prospective study of false-positive diagnosis of micrometastatic cells in the sentinel lymph nodes in colorectal cancer. Ann Surg Oncol 16(8):2166
Rodriguez-Bigas MA, Maamoun S, Weber TK et al (1996) Clinical significance of colorectal cancer: metastases in lymph nodes < 5 mm in size. Ann Surg Oncol 3(2):124–130
Brown HG, Luckasevic TM, Medich DS et al (2004) Efficacy of manual dissection of lymph nodes in colon cancer resections. Modern Pathol 17(4):402
Short SS, Stojadinovic A, Nissan A et al (2012) Adjuvant treatment of early colon cancer with micrometastases: results of a national survey. J Surg Oncol 106(2):119–122. https://doi.org/10.1002/jso.23057
Viehl CT, Weixler B, Guller U et al (2017) Presence of bone marrow micro-metastases in stage I-III colon cancer patients is associated with worse disease-free and overall survival. Cancer Med 6(5):918–927. https://doi.org/10.1002/cam4.1056
Leong SP, Tseng WW (2014) Micrometastatic cancer cells in lymph nodes, bone marrow, and blood: clinical significance and biologic implications. CA Cancer J Clin 64(3):195–206. https://doi.org/10.3322/caac.21217
Rahbari NN, Aigner M, Thorlund K et al (2010) Meta-analysis shows that detection of circulating tumor cells indicates poor prognosis in patients with colorectal cancer. Gastroenterology 138(5):1714–1726. https://doi.org/10.1053/j.gastro.2010.01.008
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Saha, S., Elgamal, M., Cherry, M. et al. Challenging the conventional treatment of colon cancer by sentinel lymph node mapping and its role of detecting micrometastases for adjuvant chemotherapy. Clin Exp Metastasis 35, 463–469 (2018). https://doi.org/10.1007/s10585-018-9927-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10585-018-9927-5