Abstract
Purpose
AMG 986 is a novel apelin receptor (APJ) agonist that improves cardiac contractility in animal models without adversely impacting hemodynamics. This phase 1b study evaluated the safety/tolerability, pharmacokinetics, and pharmacodynamics of AMG 986 in healthy subjects and patients with heart failure (HF).
Methods
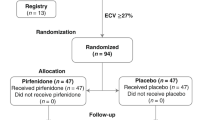
Healthy adults (Parts A/B) and HF patients (Part C) aged 18–85 years were randomized 3:1 to single-dose oral/IV AMG 986 or placebo (Part A); multiple-dose oral/IV AMG 986 or placebo (Part B); or escalating-dose oral AMG 986 or placebo (Part C). Primary endpoint: treatment-emergent adverse events, laboratory values/vital signs/ECGs; others included AMG 986 pharmacokinetics, left ventricular (LV) function.
Results
Overall, 182 subjects were randomized (AMG 986/healthy: n = 116, placebo, n = 38; AMG 986/HF: n = 20, placebo, n = 8). AMG 986 had acceptable safety profile; no clinically significant dose-related impact on safety parameters up to 650 mg/day was observed. AMG 986 exposures increased nonlinearly with increasing doses; minimal accumulation was observed. In HF with reduced ejection fraction patients, there were numerical increases in percent changes from baseline in LV ejection fraction and stroke volume by volumetric assessment with AMG 986 vs placebo (stroke volume increase not recapitulated by Doppler).
Conclusions
In healthy subjects and HF patients, short-term AMG 986 treatment was well tolerated. Consistent with this observation, clinically meaningful pharmacodynamic effects in HF patients were not observed. Changes in ejection fraction and stroke volume in HF patients suggest additional studies may be needed to better define the clinical utility and optimal dosing for this molecule.
Trial Registration Number
ClinicalTrials.gov NCT03276728.
Date of Registration
September 8, 2017








Similar content being viewed by others
Data Availability
Qualified researchers may request data from Amgen clinical studies. Complete details are available at the following: http://www.amgen.com/datasharing.
Code Availability
Not applicable
References
Virani SS, Alonso A, Benjamin EJ, et al. Heart disease and stroke statistics-2020 update: a report from theAmerican Heart Association. Circulation. 2020. https://doi.org/10.1161/cir.0000000000000757.
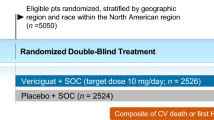
Armstrong PW, Pieske B, Anstrom KJ, et al. Vericiguat in patients with heart failure with reduced ejection fraction. N Engl J Med. 2020. https://doi.org/10.1056/nejmoa1915928.
Cleland JG, Daubert J-C, Erdmann E, et al. The effectof cardiac resynchronization on morbidity and mortality in heart failure. N Engl J Med. 2005. https://doi.org/10.1056/nejmoa050496.
Krum H, Teerlink JR. Medical therapy for chronic heart failure. Lancet. 2011. https://doi.org/10.1016/s0140-6736(11)61038-6.
McMurray JJV, Solomon SD, Inzucchi SE, et al. Dapagliflozin in patients with heart failure and reduced ejection fraction. N Engl J Med. 2019. https://doi.org/10.1056/nejmoa1911303.
Ponikowski P, Voors AA, Ankeret SD, et al. 2016 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure: the task force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology ESC. Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2016. https://doi.org/10.1093/eurheartj/ehw128.
Teerlink JR, Diaz R, Felker GM, et al. Cardiac myosin activationwith omecamtiv mecarbil in systolic heart failure. N Engl J Med. 2021. https://doi.org/10.1056/nejmoa2025797.
Yancy CW, Jessup M, Bozkurt B, et al. ACC/AHA/HFSA focused update of the 2013 ACCF/AHA Guideline for the Management of Heart Failure: a Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Failure Society of America. Circulation. 2017;2017. https://doi.org/10.1161/cir.0000000000000509.
Cohen-Solal A, Logeart D. Is the glass half full or half emptyafter PARAGON-HF? Cardiovasc Res. 2020. https://doi.org/10.1093/cvr/cvz326.
Solomon SD, McMurray JJV, Anand IS, et al. Angiotensin-neprilysin inhibition in heart failure with preserved ejection fraction. N Engl J Med. 2019. https://doi.org/10.1056/nejmoa1908655.
Anker SD, Butler J, Filippatos G, et al. Empagliflozin in heart failure with a preserved ejection fraction. N Engl J Med. 2021. https://doi.org/10.1056/NEJMoa2107038.
Chng SC, Ho L, Tian J, Reversade B. ELABELA: a hormone essential for heart development signals via the apelinreceptor. Dev Cell. 2013. https://doi.org/10.1016/j.devcel.2013.11.002.
O’Dowd BF, Heiber M, Chan A, et al. A human gene that shows identity with the gene encoding the angiotensin receptor is located on chromosome 11. Gene. 1993. https://doi.org/10.1016/0378-1119(93)90495-o.
Tatemoto K, Hosoya M, Habata Y, et al. Isolation and characterization of a novel endogenous peptide ligand for the human APJ receptor. Biochem BiophysRes Commun. 1998. https://doi.org/10.1006/bbrc.1998.9489.
Kleinz MJ, Skepper JN, Davenport AP. Immunocytochemical localisation of the apelin receptor, APJ, to human cardiomyocytes, vascular smooth muscleand endothelial cells. Regul Pept. 2005. https://doi.org/10.1016/j.regpep.2004.10.019.
Eyries M, Siegfried G, Ciumas M, et al. Hypoxia-induced apelin expression regulates endothelial cell proliferation and regenerativeangiogenesis. Circ Res. 2008. https://doi.org/10.1161/circresaha.108.179333.
O’Carroll AM, Lolait SJ. Regulation of rat APJ receptor messenger ribonucleic acid expression in magnocellular neurones of theparaventricular and supraopric nuclei by osmotic stimuli. J Neuroendocrinol. 2003. https://doi.org/10.1046/j.1365-2826.2003.01044.x.
Parikh VN, Liu J, Shang C, et al. Apelin and APJ orchestrate complex tissue-specificcontrol of cardiomyocyte hypertrophy and contractility in the hypertrophy-heart failure transition. Am J Physiol HeartCirc Physiol. 2018. https://doi.org/10.1152/ajpheart.00693.2017.
Ashley E, Powers J, Chen M, et al. Theendogenous peptide apelin potently improves cardiac contractility and reduces cardiac loading in vivo. CardiovasRes. 2005. https://doi.org/10.1016/j.cardiores.2004.08.018.
Berry MF, Pirolli TJ, Jayasankar V, et al. Apelin has in vivo inotropic effects on normal and failing hearts. Circulation . 2004. https://doi.org/10.1161/01.cir.0000138382.57325.5c.
Cheng X, Cheng XS, Pang CCY. Venous dilator effect ofapelin, an endogenous peptide ligand for the orphan APJ receptor, in conscious rats. Eur J Pharmacol. 2003. https://doi.org/10.1016/s0014-2999(03)01821-1.
Dalzell JR, Rocchiccioli JP, Weir RA, et al. The emergingpotential of the apelin-APJ system in heart failure. J Card Fail. 2015. https://doi.org/10.1016/j.cardfail.2015.03.007.
Salcedo A, Garijo J, Monge L, et al. Apelin effects in human splanchnic arteries. Role of nitric oxide and prostanoids. Regul Pept. 2007. https://doi.org/10.1016/j.regpep.2007.06.005.
Tatemoto K, Takayama K, Zou MX, Kumaki I, Zhang W, Kumano K, et al. The novel peptide apelin lowers blood pressure via a nitric oxidedependentmechanism. Regul Pept. 2001. https://doi.org/10.1016/s0167-0115(01)00236-1.
Cheng Hai, Chen Yuhan, Li Xueling, et al. Involvement of Apelin/APJ Axis in Thrombogenesis in Valve Heart Disease Patients with Atrial Fibrillation. Int Heart J. 2019;60:145–50.
Hu H, He L, Li L, Chen L. Apelin/APJ system as a therapeutic target in diabetes and its complications. Mol Genet Metab. 2016. https://doi.org/10.1016/j.ymgme.2016.07.012.
Vinel C, Lukjanenko L, Batut A, et al. The exerkine apelinreverses age-associated sarcopenia. Nat Med. 2018. https://doi.org/10.1038/s41591-018-0131-6.
Chandrasekeran B, Dar O, McDonagh T. The role of apelin in cardiovascular function and heart failure. Eur JHeart Fail. 2008. https://doi.org/10.1016/j.ejheart.2008.06.002.
Chen MM, Ashley EA, Deng DXF, et al. Novel role for the potent endogenous inotrope apelin in human cardiac dysfunction. Circulation. 2003. https://doi.org/10.1161/01.cir.0000091235.94914.75.
Boal F, Timotin A, Roumegoux J, et al. Apelin-13administration protects against ischaemia/reperfusion-mediated apoptosis through the FoxO1 pathway in high-fatdiet induced obesity. Br J Pharmacol. 2016. https://doi.org/10.1111/bph.13485.
Chun HJ, Ali ZA, Kojima Y, et al. Apelin signaling antagonizes Ang II effects in mouse models of atherosclerosis. J Clin Invest. 2008. https://doi.org/10.1172/jci34871.
Japp AG, Cruden NL, Barnes G, et al. Acute cardiovascular effects of apelin in humans: potential role in patients with chronic heart failure. Circulation. 2010. https://doi.org/10.1161/circulationaha.109.911339.
Maguire JJ, Kleinz MJ, Pitkin SL, Davenport AP. [Pyr1]apelin-13 identified as the predominant apelin isoform in the human heart: vasoactive mechanisms and inotropic action in disease. Hypertension. 2009. https://doi.org/10.1161/hypertensionaha.109.134619.
Zhong JC, Zhang ZZ, Wang W, McKinnie SMK, Vederas JC, Oudit GY. Targeting the apelin pathway as a novel therapeutic approach for cardiovascular diseases. Biochim Biophys Acta Mol Basis Dis. 2017. https://doi.org/10.1016/j.bbadis.2016.11.007.
Brash L, Barnes GD, Brewis MJ, et al. Short-term hemodynamiceffects of apelin in patients with pulmonary arterial hypertension. JACC Basic Trans Sci. 2018. https://doi.org/10.1016/j.jacbts.2018.01.013.
Ason B, Chen Y, Guo Q, et al. Cardiovascular response to small-molecule APJ activation. JCI Insight. 2020. https://doi.org/10.1172/jci.insight.132898.
Trivedi A, Mather O, Vega S, Simiens MA, Hellawell J, Lee E. Effect of severe renal impairment on the safety, Tolerability, and Pharmacokinetics of AMG 986. Accepted for publication in Clinical Drug Investigation 2022.
Trivedi A, Mather O, Vega S, Hutton S, Hellawell J, Lee E. A phase 1 open-label study to evaluate the effect of food and concomitant itraconazole administration on the Pharmacokinetics of AMG 986 in Healthy Subjects. Accepted for publication in Clinical Pharmacology in Drug Development. 2022. https://doi.org/10.1002/cpdd.1074.
Luis SA, Chan J, Pellikka PA. Echocardiographic assessment of left ventricular systolic function: an overview of contemporary techniques, including speckle-tracking echocardiography. Mayo Clin Proc. 2019. https://doi.org/10.1016/j.mayocp.2018.07.017.
Butler J, Hamo CE, Udelson JE, et al. Reassessing phase II heart failure clinical trials: Consensus recommendations. Circ Heart Fail. 2017. https://doi.org/10.1161/circheartfailure.116.003800.
Acknowledgements
Employees of Amgen were involved in the study design, collection, analysis and interpretation of data, writing of the report, and decision to submit the article for publication. We would like to thank the investigators, clinical staff, and patients who participated in this study. Medical writing and editorial support was provided by Eric Justice of BioScience Communications, New York, New York, USA (on behalf of Amgen), and Liam Gillies, PhD, funded by Amgen.
Funding
This study was sponsored by Amgen Inc.
Author information
Authors and Affiliations
Contributions
JH: study design, study oversight, data collection, analysis and interpretation of data, writing of the report; AT: analysis and interpretation of data, writing of the report; KT: analysis and interpretation of data, writing of the report; SAA: analysis and interpretation of data, writing of the report; AK: study design, study oversight, data collection, analysis and interpretation of data, writing of the report; all other authors (external clinical PIs): enrollment of human subjects, analysis and interpretation of data, writing of the report.
Corresponding author
Ethics declarations
Ethics Approval
This study was conducted in accordance with the Declaration of Helsinki and Good Clinical Practice guidelines. Independent ethics committees and regulatory agencies (as appropriate) approved the study protocol before the study was initiated.
Consent to Participate
All subjects provided their written informed consent to participate.
Consent for Publication
All authors have approved the decision to submit the manuscript for publication.
Conflict of Interest
P. Winkle has no competing interests to declare. S. Goldsmith has no competing interests to declare. M.J. Koren is an employee of a company that received research grants and consulting fees from Amgen. S. Lepage has no competing interests to declare. J. Hellawell, A. Trivedi, K. Tsirtsonis, and S.A. Abbasi are employees and shareholders of Amgen. A. Kaufman is a former employee and shareholder of Amgen. R. Troughton has received grant funding from American Regent, Amgen, Bayer, Merck, and Roche Diagnostics, and personal fees from Merck and Roche Diagnostics. A. Voors has received research support and/or consulting fees from Amgen, AstraZeneca, Bayer AG, Boehringer Ingelheim, Cytokinetics, Merck, MyoKardia, Novartis, Novo Nordisk, and Roche Diagnostics. The Assistance Publique–Hôpitaux de Paris, which employs J.-S. Hulot, has received research grants from BioSerenity, Novo Nordisk, Sanofi, and Servier. J.-S. Hulot has also received speaker, advisory board, and consultancy fees from Amgen, AstraZeneca, Bayer, Bristol-Myers Squibb, Novartis, and Novo Nordisk. E. Donal has had research facilities provided by and received fees from Abbott and General Electric Healthcare. N. Kazemi has no competing interests to declare. J. Neutel has no competing interests to declare. All authors reviewed this manuscript in draft form, provided critical input during the development process, and approved its submission for publication.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Winkle, P., Goldsmith, S., Koren, M.J. et al. A First-in-Human Study of AMG 986, a Novel Apelin Receptor Agonist, in Healthy Subjects and Heart Failure Patients. Cardiovasc Drugs Ther 37, 743–755 (2023). https://doi.org/10.1007/s10557-022-07328-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10557-022-07328-w