Abstract
Background and Purpose
The safety and efficacy of uninterrupted, minimally interrupted (one dose skipped) or completely interrupted (24 h skipped) oral anticoagulant therapy in patients with atrial fibrillation (AF) ablation are poorly defined. We conducted a network meta-analysis to explore the effect of interrupted or uninterrupted oral anticoagulants in patients with AF undergoing ablation.
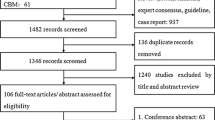
Methods
The Cochrane Library, PubMed and Embase databases were systematically searched for studies comparing uninterrupted, minimally interrupted or completely interrupted non-vitamin K antagonist oral anticoagulants (NOACs) with continuous or interrupted warfarin in patients undergoing AF ablation.
Results
Twelve randomized clinical trials (RCTs) with a total of 5597 patients with AF undergoing catheter ablation were included. For thromboembolism, minimally interrupted NOACs (OR 0.03, 95% CI 0.01–0.35), uninterrupted NOACs (OR 0.04, 95% CI 0.01–0.23) and continuous VKAs (OR 0.05, 95% CI 0.01–0.21) were better than interrupted warfarin. The risk of total bleeding appeared higher in the completely interrupted NOAC group compared with the minimally interrupted NOACs (OR 2.74, 95% CI 1.18–6.37), uninterrupted NOACs (OR 2.15, 95% CI 1.05–4.38) and uninterrupted warfarin (OR 2.04, 95% CI 1.02–4.08). To reduce the risk of total bleeding, minimally interrupted NOACs (OR 0.15, 95% CI 0.08–0.27), uninterrupted NOACs (OR 0.19, 95% CI 0.14–0.42) and uninterrupted warfarin (OR 0.24, 95% CI 0.15–0.39) were better than interrupted warfarin. In the event of major bleeding, there was no significant difference in the interrupted NOAC, uninterrupted NOAC, interrupted VKA and uninterrupted VKA groups.
Conclusions
These three NOAC strategies may have similar safety and efficacy in terms of thromboembolism and major bleeding complications. The total bleeding risk of completely interrupted oral anticoagulants is higher than that of uninterrupted and minimally interrupted NOACs. For thromboembolism, minimally interrupted NOACs, uninterrupted NOACs and continuous VKAs were better than interrupted warfarin.




Similar content being viewed by others
References
Benjamin EJ, Virani SS, Callaway CW, Chamberlain AM, Chang AR, Cheng S, et al. Heart disease and stroke statistics 2018 update: a report from the American Heart Association. Circulation. 2018;137(12):e67–e492.
Wolf PA, Abbott RD, Kannel WB. Atrial fibrillation as an independent risk factor for stroke: the Framingham study. Stroke. 1991;22(8):983–8.
Calkins H, Hindricks G, Cappato R, Kim YH, Saad EB, Aguinaga L, et al. 2017 HRS/EHRA/ECAS/APHRS/SOLAECE expert consensus statement on catheter and surgical ablation of atrial fibrillation. Heart Rhythm. 2017;14(10):e275–444.
January CT, Wann LS, Calkins H, et al. 2019 AHA/ACC/HRS focused update of the 2014 AHA/ACC/HRS guideline for the Management of Patients with Atrial Fibrillation: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines and the Heart Rhythm Society. Heart Rhythm. 2019;16(8):e66–e93.
Belhassen B. A 1 per 1,000 mortality rate after catheter ablation of atrial fibrillation: an acceptable risk? J Am Coll Cardiol. 2009;53(19):1804–6.
Cappato R, Calkins H, Chen SA, Davies W, Iesaka Y, Kalman J, et al. Updated worldwide survey on the methods, efficacy, and safety of catheter ablation for human atrial fibrillation. Circ Arrhythm Electrophysiol. 2010;3(1):32–8.
Haeusler KG, Kirchhof P, Endres M. Left atrial catheter ablation and ischemic stroke. Stroke. 2012;43(1):265–70.
Di Biase L, Burkhardt JD, Santangeli P, et al. Periprocedural stroke and bleeding complications in patients undergoing catheter ablation of atrial fibrillation with different anticoagulation management: results from the role of coumadin in preventing thromboembolism in atrial fibrillation (AF) patients undergoing catheter ablation (COMPARE) randomized trial. Circulation. 2014;129(25):2638–44.
January CT, Wann LS, Alpert JS, Calkins H, Cigarroa JE, Cleveland JC Jr, et al. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines and the Heart Rhythm Society. Circulation. 2014;130(23):e199–267.
Potpara TS, Larsen TB, Deharo JC, et al. Oral anticoagulant therapy for stroke prevention in patients with atrial fibrillation undergoing ablation: results from the first European snapshot survey on procedural routines for atrial fibrillation ablation (ESS-PRAFA). Europace. 2015;17(6):986–93.
Konduru SV, Cheema AA, Jones P, Li Y, Ramza B, Wimmer AP. Differences in intraprocedural ACTs with standardized heparin dosing during catheter ablation for atrial fibrillation in patients treated with dabigatran vs. patients on uninterrupted warfarin. J Interv Card Electrophysiol. 2012;35(3):277–84.
Dillier R, Ammar S, Hessling G, Kaess B, Pavaci H, Buiatti A, et al. Safety of continuous periprocedural rivaroxaban for patients undergoing left atrial catheter ablation procedures. Circ Arrhythm Electrophysiol. 2014;7(4):576–82.
Lakkireddy D, Reddy YM, Di Biase L, et al. Feasibility and safety of uninterrupted rivaroxaban for periprocedural anticoagulation in patients undergoing radiofrequency ablation for atrial fibrillation: results from a multicenter prospective registry. J Am Coll Cardiol. 2014;63(10):982–8.
Di Biase L, Lakkireddy D, Trivedi C, et al. Feasibility and safety of uninterrupted periprocedural apixaban administration in patients undergoing radiofrequency catheter ablation for atrial fibrillation: results from a multicenter study. Heart Rhythm. 2015;12(6):1162–8.
Cappato R, Marchlinski FE, Hohnloser SH, Naccarelli GV, Xiang J, Wilber DJ, et al. Uninterrupted rivaroxaban vs. uninterrupted vitamin K antagonists for catheter ablation in non-valvular atrial fibrillation. Eur Heart J. 2015;36(28):1805–11.
Kuwahara T, Abe M, Yamaki M, Fujieda H, Abe Y, Hashimoto K, et al. Apixaban versus warfarin for the prevention of periprocedural cerebral thromboembolism in atrial fibrillation ablation: multicenter prospective randomized study. J Cardiovasc Electrophysiol. 2016;27(5):549–54.
Calkins H, Willems S, Gerstenfeld EP, Verma A, Schilling R, Hohnloser SH, et al. Uninterrupted dabigatran versus warfarin for ablation in atrial fibrillation. N Engl J Med. 2017;376(17):1627–36.
Kirchhof P, Haeusler KG, Blank B, de Bono J, Callans D, Elvan A, et al. Apixaban in patients at risk of stroke undergoing atrial fibrillation ablation. Eur Heart J. 2018;39(32):2942–55.
Hohnloser SH, Camm J, Cappato R, et al. Uninterrupted edoxaban vs. vitamin K antagonists for ablation of atrial fibrillation: the ELIMINATE-AF trial. Eur Heart J. 2019;40(36):3013–3021.
Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ (Clinical Research Ed.). 2009;339:b2700.
Schulman S, Kearon C, Subcommittee on Control of Anticoagulation of the S, Standardization Committee of the International Society on T, Haemostasis. Definition of major bleeding in clinical investigations of antihemostatic medicinal products in non-surgical patients. J Thromb Haemost. 2005;3(4):692–4.
Yang P, Shen W, Chen X, Zhu D, Xu X, Wu T, et al. Comparative efficacy and safety of mineralocorticoid receptor antagonists in heart failure: a network meta-analysis of randomized controlled trials. Heart Fail Rev. 2019;24:637–46.
Salanti G, Ades AE, Ioannidis JP. Graphical methods and numerical summaries for presenting results from multipletreatment meta-analysis: an overview and tutorial. J Clin Epidemiol. 2011;64:163–71.
Lu G, Ades AE. Combination of direct and indirect evidence in mixed treatment comparisons. Stat Med. 2004;23:3105–24.
Kimura T, Kashimura S, Nishiyama T, Katsumata Y, Inagawa K, Ikegami Y, et al. Asymptomatic cerebral infarction during catheter ablation for atrial fibrillation: comparing uninterrupted rivaroxaban and warfarin (ASCERTAIN). JACC Clin Electrophysiol. 2018;4(12):1598–609.
Nin T, Sairaku A, Yoshida Y, Kamiya H, Tatematsu Y, Nanasato M, et al. A randomized controlled trial of dabigatran versus warfarin for periablation anticoagulation in patients undergoing ablation of atrial fibrillation. Pacing Clin Electrophysiol. 2013;36(2):172–9.
Nogami A, Harada T, Sekiguchi Y, Otani R, Yoshida Y, Yoshida K, et al. Safety and efficacy of minimally interrupted dabigatran vs uninterrupted warfarin therapy in adults undergoing atrial fibrillation catheter ablation: a randomized clinical trial. JAMA Netw Open. 2019;2(4):e191994.
Reynolds MR, Allison JS, Natale A, Weisberg IL, Ellenbogen KA, Richards M, et al. A prospective randomized trial of apixaban dosing during atrial fibrillation ablation: the AEIOU trial. JACC Clin Electrophysiol. 2018;4(5):580–8.
Yoshida Y, Watarai M, Fujii K, Shimizu W, Satomi K, Inden Y, et al. Comparison of uninterrupted anticoagulation with dabigatran etexilate or warfarin in the periprocedural period for atrial fibrillation catheter ablation: results of the Japanese subgroup of the RE-CIRCUIT trial. J Arrhythm. 2018;34(2):148–57.
Yu HT, Shim J, Park J, Kim TH, Uhm JS, Kim JY, et al. When is it appropriate to stop non-vitamin K antagonist oral anticoagulants before catheter ablation of atrial fibrillation? A multicentre prospective randomized study. Eur Heart J. 2019;40(19):1531–7.
Page SP, Siddiqui MS, Finlay M, Hunter RJ, Abrams DJ, Dhinoja M, et al. Catheter ablation for atrial fibrillation on uninterrupted warfarin: can it be done without echo guidance? J Cardiovasc Electrophysiol. 2011;22(3):265–70.
Di Biase L, Burkhardt JD, Mohanty P, et al. Periprocedural stroke and management of major bleeding complications in patients undergoing catheter ablation of atrial fibrillation: the impact of periprocedural therapeutic international normalized ratio. Circulation. 2010;121(23):2550–6.
Jackson LR 2nd, Becker RC. Novel oral anticoagulants: pharmacology, coagulation measures, and considerations for reversal. J Thromb Thrombolysis. 2014;37(3):380–91.
Aryal MR, Ukaigwe A, Pandit A, Karmacharya P, Pradhan R, Mainali NR, et al. Meta-analysis of efficacy and safety of rivaroxaban compared with warfarin or dabigatran in patients undergoing catheter ablation for atrial fibrillation. Am J Cardiol. 2014;114(4):577–82.
Douketis JD, Spyropoulos AC, Duncan J, et al. Perioperative management of patients with atrial fibrillation receiving a direct oral anticoagulant. JAMA Intern Med. 2019;179(11):1469–78.
Nakamura R, Okishige K, Shigeta T, Nishimura T, Kurabayashi M, Yamauchi Y, et al. Clinical comparative study regarding interrupted and uninterrupted dabigatran therapy during perioperative periods of cryoballoon ablation for paroxysmal atrial fibrillation. J Cardiol. 2019;74(2):150–5.
Gorla R, Dentali F, Crippa M, Marazzato J, di Minno MND, Grandi AM, et al. Perioperative safety and efficacy of different anticoagulation strategies with direct oral anticoagulants in pulmonary vein isolation: a meta-analysis. JACC Clin Electrophysiol. 2018;4:794–806.
Jan S, Peter V, Tatjana SP, et al. The 2018 European heart rhythm association practical guide on the use of non-vitamin K antagonist oral anticoagulants in patients with atrial fibrillation. Eur Heart J. 2018;39:1330–93.
Verheugt FW, Granger CB. Oral anticoagulants for stroke prevention in atrial fibrillation: current status, special situations, and unmet needs. Lancet. 2015;386(9990):303–10.
Heidbuchel H, Verhamme P, Alings M, Antz M, Hacke W, Oldgren J, et al. European Heart Rhythm Association. And the European Heart Rhythm association. European Heart Rhythm Association Practical Guide on the use of new oral anticoagulants in patients with non-valvular atrial fibrillation. Europace. 2013;15:625–51.
Funding
This work was supported by the Provincial Plans - Social Development Areas - Major Projects of Jiangxi Province (No. 20161ACG70012), the Jiangxi Graduate Innovation Special Fund (No. YC2019-B039), and the State Scholarship Fund of the China Scholarship Council (grant number 201906820003).
Author information
Authors and Affiliations
Contributions
Y-PP, W-CX and Y-YQ performed the meta-analysis; H-TQ and Y-S were responsible for the statistical analysis; S-W and X-GS provided editing assistance; and W-QH prepared the manuscript. All the authors have reviewed and agreed to this information before submission.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yang, P., Wang, C., Ye, Y. et al. Interrupted or Uninterrupted Oral Anticoagulants in Patients Undergoing Atrial Fibrillation Ablation. Cardiovasc Drugs Ther 34, 371–381 (2020). https://doi.org/10.1007/s10557-020-06967-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10557-020-06967-1