Abstract
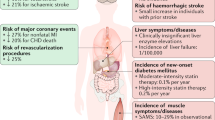
Statins are currently the primary treatment for hyperlipidemia, particularly for the treatment of high levels of low-density lipoprotein cholesterol (LDL-C), as many studies have proven benefit in a variety of populations. The benefits of statin treatment for high cholesterol have been proven in many trials. Forefront among different adverse events is statin-induced myopathy, which still eludes complete understanding, and may range anywhere from muscle soreness or fatigue to potentially extremely rare occurrence of rhabdomyolysis.
As most adverse events are rare and not life-threatening, in high-risk patients, a high-dose statin should be started initially as data suggests that clinicians rarely up titrate statin therapy after initial prescription leading to under-treatment of many patients requiring high-dose statin therapy. As we will discuss in this paper, musculoskeletal side effects are the main concern and reason for discontinuing statin therapy. The occurrence and true association of other adverse events in patients on statin such as new onset of diabetes, hepatic toxicity, or cognitive impairment are rare, controversial, and not proven. In placebo-controlled studies, abnormal liver function occurs to a similar degree in statin- and placebo-treated patients. This led to FDA removal of the requirement to monitor liver function tests in patients on statin therapy.
The combination of statins with other compounds such as ezetimibe or PCSK9 inhibitors has shown some additional benefits in the treatment of hypercholesterolemia. The goal of this manuscript is to conduct a comprehensive review about most commonly used statins and compare data on their history, structures, benefits, adverse effects, and clinical outcomes.







Similar content being viewed by others
References
Dimmler S. Cardiovascular disease review series. Embo Mol Med. 2011;3:697.
Benjamin EJ, Virani SS, Callaway CW, et al. Heart disease and stroke statistics—2018 update: a report from the American Heart Association. Circulation. 2018; 137(12).
Stone NJ, Robinson JG, Lichtenstein AH, Bairey Merz CN, Blum CB, Eckel RH, et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults. J Am Coll Cardiol. 2014;63:2889–934.
Patel B. Pharmacology of statins: a brief overview. Nurse Prescribing. 2014;12(9):451–6.
Chakravartri R, Sahai V. Compactin—a review. Appl Microbiol Biotechnol. 2004;64:618–24.
Stancu C, Sima A. Statins: mechanism of action and effects. J Cell Mol Med. 2001;5(4):378–87.
Endo A. The origin of the statins. Atherosclerosis (Supplements) (Component). 2004;5:125–30.
Istvan ES, Deisenhofer J. Structural mechanism for statin inhibition of HMG-CoA reductase. Am Heart J. 2002;144(6 suppl):S27–32.
Lawrence CM, Rodwell VW, Stauffacher CV. Crystal structure of Pseudomonas mevalonii HMG-CoA reductase at 3.0 angstrom resolution. Science. 1995;268(1758).
Benjamin EJ, Virani SS, Callaway CW, et al. Heart disease and stroke statistics—2018 update: a report from the American Heart Association. Circulation. 2018; 137(12).
Baigent C, Keech A, Kearney PM, Blackwell L, Buck G, Pollicino C, et al. Efficacy and safety of cholesterol-lowering treatment: prospective meta-analysis of data from 90,056 participants in 14 randomised trials of statins. Lancet. 2005;366(9493):1267–78.
Liao JK, Laufs U. Pleiotropic effects of statins. Annu Rev Pharmacol Toxicol. 2005;45:89–118.
Tawakol A, Fayad ZA, Mogg R, Alon A, Klimas MT, Dansky H, et al. Intensification of statin therapy results in a rapid reduction in atherosclerotic inflammation: results of a multicenter fluorodeoxyglucose-positron emission tomography/computed tomography feasibility study. J Am Coll Cardiol. 2013;62(10):909–17.
Lovastatin Study Groups I Through IV. Lovastatin 5-year safety and efficacy study. Arch Intern Med. 1993;153:1079–87.
Shepherd J, Blauw GJ, Murphy MB, Bollen ELEM, Buckley BM, Cobbe SM, et al. Pravastatin in elderly individuals at risk of vascular disease (PROSPER): a randomised controlled trial. Lancet. 2002;360:1623–30.
Adams SP, Tsang M, Wright JM. Lipid-lowering efficacy of atorvastatin. Cochrane Database Syst Rev. 2015;3:CD008226.
Jones P, Kafonek S, Laurora I, Hunninghake D. Comparative dose efficacy study of atorvastatin versus simvastatin, pravastatin, lovastatin, and fluvastatin in patients with hypercholesterolemia (the CURVES study). Am J Cardiol. 1998;81(5):582–7.
Adams SP, Sekhon SS, Wright JM. Lipid-lowering efficacy of rosuvastatin. Cochrane Database Syst Rev. 2014:11.
Jones P, Davidson M, Stein E, Bays HE, McKenney J, Miller E, et al. Comparison of the efficacy and safety of rosuvastatin versus atorvastatin, simvastatin, and pravastatin across doses (STELLAR trial). Am J Cardiol. 2003;92:152–60.
Wang C-Y, Liu P-Y, Liao JK. Pleiotropic effects of statin therapy: molecular mechanisms and clinical results. Trends Mol Med. 2008;14(1):37–44.
Kavalipati N, Shah J, Ramakrishan A, Vasnawala H. Pleiotropic effects of statins. Advances in pediatrics. Indian J Endocrinol Metab. 2015;19(5):554–62.
Ridker PM. The JUPITER trial: results, controversies, and implications for prevention. Circulation Cardiovasc Qual Outcomes. 2009;2:279–85.
Katz DH, Intwala SS, Stone NJ. Addressing statin adverse effects in the clinic: the 5 Ms. J Cardiovasc Pharmacol Ther. 2014;19(6):533–42.
Denus S, Spinler SA, Miller K, Peterson AM. Statins and liver toxicity: a meta-analysis. Pharmacotherapy. 2004;24:584–91.
Trompet S, van Vliet P, de Craen AJM, et al. Pravastatin and cognitive function in the elderly. Results of the PROSPER study. J Neurol. 2010;257:85–90.
Bruckert E, Hayem G, Dejager S, Yau C, Bégaud B. Mild to moderate muscular symptoms with high-dosage statin therapy in hyperlipidemic patients the PRIMO study. Cardiovasc Drugs Ther. 2005;19:403–14.
Ahmed W, Khan N, Glueck CJ, Pandey S, Wang P, Goldenberg N, et al. Low serum 25 (OH) vitamin D levels (<32 ng/mL) are associated with reversible myositis-myalgia in statin-treated patients. Transl Res. 2009;153(1):11–6.
Ovesjö M-L, Skilving I, Bergman P, Rane A, Ekström L, Björkhem-Bergman L. Low vitamin D levels and genetic polymorphism in the vitamin D receptor are associated with increased risk of statin-induced myopathy. Basic ClinPharmacol Toxicol. 2015;118(3):214–8.
Riche KD, Arnall J, Rieser K, East HE, Riche DM. Impact of vitamin D status on statin-induced myopathy. J Clin Transl Endocrinol. 2016;6:56–9.
Kang J, Nguyen Q, Mutka J, Le Q. Rechallenging statin therapy in veterans with statin-induced myopathy post vitamin D replenishment. J Pharm Pract. 2016;30(5):521–7.
Golomb BA, Evans MA. Statin adverse effects: a review of the literature and evidence for a mitochondrial mechanism. Am J Cardiovasc Drugs. 2008;8(6):373–418.
Bitzur R, Cohen H, Kamari Y, Harats D. Intolerance to statins: mechanisms and management. Diabetes Care. 2013;36(Suppl 2):S325–30.
Pinal-Fernandez I, Casal-Dominguez M, Mammen AL. Statins: pros and cons. Med Clin (Barc). 2018;150(10):398–402.
Ahmadi Y, Ghorbanihaghjo A, Naghi-Zadeh M, Yagin N. Oxidative stress as a possible mechanism of statin-induced myopathy. Inflammopharmacology. 2018;26.3:667–74 Web.
Bagley WH, Yang H, Shah KH. Rhabdomyolysis. Intern Emerg Med. 2007;2:210–8.
Staffa JA, Chang J, Green L. Cerivastatin and reports of fatal rhabdomyolysis. N Engl J Med. 2002;346(7):539–40.
Thompson PD, Clarkson P, Karas RH. Statin-associated myopathy. JAMA. 2003;289(13):1681–90.
Mohassel P, Mammen AL. Anti-HMGCR Myopathy. J Neuromuscular Dis. 2018;5(1):11–20.
Dubuc G, Chamberland A, Wassef H, et al. Statins upregulate PCSK9, the gene encoding the proprotein convertase neural apoptosis-regulated convertase-1 implicated in familial hypercholesterolemia. Arterioscler Thromb Vasc Biol. 2004;24:1454–9.
Awan Z, Seidah NG, MacFadyen JG, et al. Rosuvastatin, proprotein convertase subtilisin/kexin type 9 concentrations, and LDL cholesterol response: the JUPITER trial. Clin Chem. 2012;58:183–9.
Lyu P-Y, Li R, Wang T-J, et al. Effects of plasma lipids and statins on cognitive function. Chin Med J. 2018;131(4):471.
MRC/BHF heart protection study of cholesterol lowering with simvastatin in 20,536 high-risk individuals: a randomized placebo-controlled trial. Lancet. 2002; 360(9326):7–22.
Strom BL, Schinnar R, Karlawish J, Hennessy S, Teal V, Bilker WB. Statin therapy and risk of acute memory impairment. JAMA Intern Med. 2015;175(8):1399–405.
Huang C-N, Li H-H, Lin C-L. Neuroprotective effects of statins against amyloid β-induced neurotoxicity. Neural Regen Res. 2018;13(2):198–206.
Chan D, Binks S, Nicholas JM, Frost C, Cardoso MJ, Ourselin S, et al. Effect of high-dose simvastatin on cognitive, neuropsychiatric, and health-related quality-of-life measures in secondary progressive multiple sclerosis: secondary analyses from the MS-STAT randomised, placebo-controlled trial. Lancet Neurol. 2017;16(8):591–600.
Xiaoxue L, Min Y, Shuya L, Zheng L. The association between apathy and mild cognitive impairment: a systematic review and meta-analysis. Alzheimers Dement. 2017;13(7).
Schultz BG, Patten DK, Berlau DJ. The role of statins in both cognitive impairment and protection against dementia: a tale of two mechanisms. Transl Neurodegener. 2018;7(1).
Orth M, Bellosta S. Cholesterol: its regulation and role in central nervous system disorders. Cholesterol. 2012;2012:1–19.
Golomb BA, Evans MA. Statin adverse effects. Am J Cardiovasc Drugs. 2008;8(6):373–418.
Agarwala A, Kulkarni S, Maddox T. The association of statin therapy with incident diabetes: evidence, mechanisms, and recommendations. Curr Cardiol Rep. 2018;20:50.
Anyanwagu U, Mamza J, Donnelly R, Idris I. Effects of background statin therapy on glycemic response and cardiovascular events following initiation of insulin therapy in type 2 diabetes: a large UK cohort study. Cardiovasc Diabetol. 2017;16:107.
Scattolini V, Luni C, Zambon A, et al. Simvastatin rapidly and reversibly inhibits insulin secretion in intact single-islet cultures. Diabetes Ther. 2016;7(4):679–93.
Betteridge DJ, Carmera R. The diabetogenic action of statins - mechanisms and clinical implications. Nat Rev Endocrinol. 2016;12(2):99–110.
Yaluri N, Modi S, Rodríguez ML, et al. Simvastatin impairs insulin secretion by multiple mechanisms in MIN6 cells. PLoS One. 2015;10(11).
Henriksbo B, Schertzer J. Is immunity a mechanism contributing to statin-induced diabetes? Adipocyte. 2015;4(4):1–7.
Brault M, Ray J, Gomez Y-H, Mantzoros CS, Daskalopoulou SS. Statin treatment and new-onset diabetes: a review of proposed mechanisms. Metabolism. 2014;63(6):735–45.
Brault M, Ray J, Gomez Y-H, Mantzoros CS, Daskalopoulou SS. Statin treatment and new-onset diabetes: a review of proposed mechanisms. Metabolism. 2014;63(6):735–45.
Karahalil B, Hare E, Koç G, Uslu I, Şentürk K, Özkan Y. Hepatotoxicity associated with statins. Arh Hig Rada Toksikol. 2017;68(4):254–60.
Farrag S, Hamzawy M, El-Yamany M, Saad M, Nassar N. Atorvastatin in nano-particulate formulation abates muscle and liver affliction when coalesced with coenzyme Q10 and/or vitamin E in hyperlipidemic rats. Life Sci. 2018;203:129–40.
Mach F, Ray KK, Wiklund O, Corsini A, Catapano AL, Bruckert E, et al. Adverse effects of statin therapy: perception vs. the evidence – focus on glucose homeostasis, cognitive, renal and hepatic function, haemorrhagic stroke and cataract. Eur Heart J. 2018;39(27):2526–39.
Naci H, Brugts J, Ades T. Comparative tolerability and harms of individual statins: a study-level network meta-analysis of 246 955 participants from 135 randomized, controlled trials. Circ Cardiovacs Qual Outcomes. 2013;6(4):390–9.
Clarke AT, Johnson PCD, Hall GC, Ford I, Mills PR. High dose atorvastatin associated with increased risk of significant hepatotoxicity in comparison to simvastatin in UK GPRD cohort. PLoS One. 2016;11(3).
Awad K, Serban M-C, Penson P. Effects of morning vs evening statin administration on lipid profile: a systematic review and meta-analysis. J Clin Lipidol. 2017;11(4):972–985.e9.
Lee J, Morris J, Wald N. Grapefruit juice and statins. Am J Med. 2016;129(1):26–9.
Awad K, Banach M. The optimal time of day for statin administration: a review of current evidence. Curr Opin Lipidol. 2018;29(4):340–5.
Quinn KL, Macdonald EM, Mamdani MM, Diong C, Juurlink DN. Lipophilic statins and the risk of intracranial hemorrhage following ischemic stroke: a population-based study. Drug Saf. 2017;40(10):887–93.
Gaist D, Goldstein LB, Soriano LC, Rodríguez LAG. Statins and the risk of intracerebral hemorrhage in patients with previous ischemic stroke or transient ischemic attack. Stroke. 2017;48(12):3245–51.
Naci H, Brugts J, Ades T. Comparative tolerability and harms of individual statins: a study-level network meta-analysis of 246955 participants from 135 randomized controlled trials. Circ Cardiovasc Qual Outcomes. 2013;6(4):390–9.
Karlson BW, Palmer MK, Nicholls SJ, Lundman P, Barter PJ. Doses of rosuvastatin, atorvastatin and simvastatin that induce equal reductions in LDL-C and non-HDL-C: results from the VOYAGER meta-analysis. Eur J Prev Cardiol. 2016;23(7):744–7.
Welty FK, Lewis SJ, Friday KE, Cain VA, Anzalone DA. A comparison of statin therapies in hypercholesterolemia in women: a subgroup analysis of the STELLAR study. J Women's Health. 2016;25(1):50–6.
Intensive lowering of LDL cholesterol with 80 mg versus 20 mg simvastatin daily in 12 064 survivors of myocardial infarction: a double-blind randomized trial. The Lancet. 2010; 376(9753): 1658–1669.
Tayal U, Carroll R. Should anyone still be taking simvastatin 80 mg? BMJ Case Rep. 2013;bcr2013200415.
Tayal U, Carroll R. Should anyone still be taking simvastatin 80 mg? BMJ Case Rep. 2013;bcr2013200415.
Wong N. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63(25 Pt B):2889–934.
Adams SP, Tsang M, Wright JM. Lipid lowering efficacy of atorvastatin. Cochrane Database Syst Rev. 2015;3:CD008226.
Karlson BW, Palmer MK, Nicholls SJ, Lundman P, Barter PJ. To what extent do high-intensity statins reduce low-density lipoprotein cholesterol in each of the four statin benefit groups identified by the 2013 American College of Cardiology/American Heart Association guidelines? A VOYAGER meta-analysis Atherosclerosis. 2015;241(2):450–4.
Lee H, Choi J, Cho J, Kim T, Lee H, Jung B. Regulation of endogenic metabolites by rosuvastatin in hyperlipidemia patients: an integration of metabolomics and lipidomics. Chem Phys Lipids. 2018;214:69–83.
Giral P, Neumann A, Weill A, Coste J. Cardiovascular effect of discontinuing statins for primary prevention at the age of 75 years: a nationwide population-based cohort study in France. Eur Heart J. 2019;Epub ahead of print.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Azemawah, V., Movahed, M.R., Centuori, P. et al. State of the Art Comprehensive Review of Individual Statins, Their Differences, Pharmacology, and Clinical Implications. Cardiovasc Drugs Ther 33, 625–639 (2019). https://doi.org/10.1007/s10557-019-06904-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10557-019-06904-x