Abstract
Background and Aims
Diabetes mellitus (DM) can cause left ventricular (LV) diastolic dysfunction, leading to heart failure with preserved ejection fraction (HFpEF). Dipeptidyl peptidase IV (DPP-IV) inhibitors have failed to reduce hospitalization due to HF in type 2 DM (T2D) patients in a large-scale clinical trial, despite their cardiovascular protective effects. Therefore, it is important to investigate whether DPP-IV inhibitors can improve LV diastolic dysfunction in T2D patients. The aim of the study was to evaluate whether teneligliptin, the strongest of the DPP-IV inhibitors, improves LV dysfunction or prevents the worsening of LV diastolic function in T2D patients.
Methods
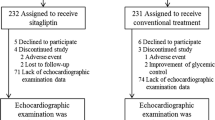
The TOPLEVEL study is designed as an open-labeled, marker-stratified randomized, parallel-group comparison, standard treatment-controlled multicenter study. TOPLEVEL includes two marker-defined subgroups to give treatment recommendations for T2D patients with normal (E/e′ < 8) or impaired LV diastolic function (E/e′ ≥ 8), where E/e′ is the ratio of peak velocity of early transmitral diastolic filling by echocardiography to early diastolic mitral annular velocity by tissue Doppler echocardiography as LV diastolic function. Patients are randomly assigned to either teneligliptin (20 or 40 mg) or the standard treatment group. All patients are followed up for 2 years. The primary endpoint measure is the change in E/e′ from baseline and 2 years after enrollment.
Conclusion and Perspectives
TOPLEVEL is a clinical trial of teneligliptin targeting LV diastolic dysfunction in T2D patients. This study demonstrates the effectiveness of DPP-IV inhibitors on LV diastolic dysfunction, an important surrogate endpoint to predict the cardiovascular outcomes of HFpEF (UMIN000014589).

Similar content being viewed by others
Availability of Data and Materials
To avoid potential bias of the analysis, the data set supporting the conclusions of this article will not be available until the final report of this trial is published.
References
Devereux RB, Roman MJ, Paranicas M, O'Grady MJ, Lee ET, Welty TK, et al. Impact of diabetes on cardiac structure and function: the strong heart study. Circulation. 2000;101(19):2271–6.
Eguchi K, Boden-Albala B, Jin Z, Rundek T, Sacco RL, Homma S, et al. Association between diabetes mellitus and left ventricular hypertrophy in a multiethnic population. Am J Cardiol. 2008;101(12):1787–91.
From AM, Scott CG, Chen HH. The development of heart failure in patients with diabetes mellitus and pre-clinical diastolic dysfunction a population-based study. J Am Coll Cardiol. 2010;55(4):300–5.
Vinereanu D, Nicolaides E, Tweddel AC, Madler CF, Holst B, Boden LE, et al. Subclinical left ventricular dysfunction in asymptomatic patients with type II diabetes mellitus, related to serum lipids and glycated haemoglobin. Clin Sci (London, England : 1979). 2003;105(5):591–9.
Aneja A, Tang WH, Bansilal S, Garcia MJ, Farkouh ME. Diabetic cardiomyopathy: insights into pathogenesis, diagnostic challenges, and therapeutic options. Am J Med. 2008;121(9):748–57.
Owan TE, Hodge DO, Herges RM, Jacobsen SJ, Roger VL, Redfield MM. Trends in prevalence and outcome of heart failure with preserved ejection fraction. N Engl J Med. 2006;355(3):251–9.
Gomez N, Touihri K, Matheeussen V, Mendes Da Costa A, Mahmoudabady M, Mathieu M, et al. Dipeptidyl peptidase IV inhibition improves cardiorenal function in overpacing-induced heart failure. Eur J Heart Fail. 2012;14(1):14–21.
Shigeta T, Aoyama M, Bando YK, Monji A, Mitsui T, Takatsu M, et al. Dipeptidyl peptidase-4 modulates left ventricular dysfunction in chronic heart failure via angiogenesis-dependent and -independent actions. Circulation. 2012;126(15):1838–51.
Son JW, Kim S. Dipeptidyl peptidase 4 inhibitors and the risk of cardiovascular disease in patients with type 2 diabetes: a tale of three studies. Diabetes Metab J. 2015;39(5):373–83.
Fukuda-Tsuru S, Anabuki J, Abe Y, Yoshida K, Ishii S. A novel, potent, and long-lasting dipeptidyl peptidase-4 inhibitor, teneligliptin, improves postprandial hyperglycemia and dyslipidemia after single and repeated administrations. Eur J Pharmacol. 2012;696(1–3):194–202.
Yoshihara F, Imazu M, Hamasaki T, Anzai T, Yasuda S, Ito S, et al. An exploratory study of Dapagliflozin for the attenuation of albuminuria in patients with heart failure and type 2 diabetes mellitus (DAPPER). Cardiovasc Drugs Ther. 2018;32(2):183–90.
Gordon Lan K, DeMets DL. Discrete sequential boundaries for clinical trials. Biometrika. 1983;70(3):659–63.
Cui L, Hung HM, Wang SJ. Modification of sample size in group sequential clinical trials. Biometrics. 1999;55(3):853–7.
Matsushita K, Blecker S, Pazin-Filho A, Bertoni A, Chang PP, Coresh J, et al. The association of hemoglobin a1c with incident heart failure among people without diabetes: the atherosclerosis risk in communities study. Diabetes. 2010;59(8):2020–6.
Gonzalez-Vilchez F, Ayuela J, Ares M, Pi J, Castillo L, Martin-Duran R. Oxidative stress and fibrosis in incipient myocardial dysfunction in type 2 diabetic patients. Int J Cardiol. 2005;101(1):53–8.
Ihm SH, Youn HJ, Shin DI, Jang SW, Park CS, Kim PJ, et al. Serum carboxy-terminal propeptide of type I procollagen (PIP) is a marker of diastolic dysfunction in patients with early type 2 diabetes mellitus. Int J Cardiol. 2007;122(3):e36–8.
Borlaug BA, Melenovsky V, Redfield MM, Kessler K, Chang HJ, Abraham TP, et al. Impact of arterial load and loading sequence on left ventricular tissue velocities in humans. J Am Coll Cardiol. 2007;50(16):1570–7.
Saiki H, Moulay G, Guenzel AJ, Liu W, Decklever TD, Classic KL, et al. Experimental cardiac radiation exposure induces ventricular diastolic dysfunction with preserved ejection fraction. Am J Physiol Heart Circ Physiol. 2017;313(2):H392–h407.
Kawaguchi M, Hay I, Fetics B, Kass DA. Combined ventricular systolic and arterial stiffening in patients with heart failure and preserved ejection fraction: implications for systolic and diastolic reserve limitations. Circulation. 2003;107(5):714–20.
Elzinga G, Westerhof N. Pressure and flow generated by the left ventricle against different impedances. Circ Res. 1973;32(2):178–86.
Hori M, Inoue M, Kitakaze M, Tsujioka K, Ishida Y, Fukunami M, et al. Ejection timing as a major determinant of left ventricular relaxation rate in isolated perfused canine heart. Circ Res. 1984;55(1):31–8.
From AM, Scott CG, Chen HH. Changes in diastolic dysfunction in diabetes mellitus over time. Am J Cardiol. 2009;103(10):1463–6.
van den Hurk K, Alssema M, Kamp O, Henry RM, Stehouwer CD, Smulders YM, et al. Independent associations of glucose status and arterial stiffness with left ventricular diastolic dysfunction: an 8-year follow-up of the Hoorn study. Diabetes Care. 2012;35(6):1258–64.
Redfield MM, Jacobsen SJ, Burnett JC Jr, Mahoney DW, Bailey KR, Rodeheffer RJ. Burden of systolic and diastolic ventricular dysfunction in the community: appreciating the scope of the heart failure epidemic. JAMA. 2003;289(2):194–202.
Okura H, Kubo T, Asawa K, Toda I, Yoshiyama M, Yoshikawa J, et al. Elevated E/E' predicts prognosis in congestive heart failure patients with preserved systolic function. Circ J. 2009;73(1):86–91.
Akiyama E, Sugiyama S, Matsuzawa Y, Konishi M, Suzuki H, Nozaki T, et al. Incremental prognostic significance of peripheral endothelial dysfunction in patients with heart failure with normal left ventricular ejection fraction. J Am Coll Cardiol. 2012;60(18):1778–86.
Ommen SR, Nishimura RA, Appleton CP, Miller FA, Oh JK, Redfield MM, et al. Clinical utility of Doppler echocardiography and tissue Doppler imaging in the estimation of left ventricular filling pressures: a comparative simultaneous Doppler-catheterization study. Circulation. 2000;102(15):1788–94.
Mullens W, Borowski AG, Curtin RJ, Thomas JD, Tang WH. Tissue Doppler imaging in the estimation of intracardiac filling pressure in decompensated patients with advanced systolic heart failure. Circulation. 2009;119(1):62–70.
Mitter SS, Shah SJ, Thomas JD. A test in context: E/A and E/e' to Assess Diastolic Dysfunction and LV Filling Pressure. J Am Coll Cardiol. 2017;69(11):1451–64.
Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JG, Coats AJ, et al. 2016 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure: the task force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC)developed with the special contribution of the heart failure association (HFA) of the ESC. Eur Heart J. 2016;37(27):2129–200.
Takahashi A, Ihara M, Yamazaki S, Asanuma H, Asakura M, Kitakaze M. Impact of either GLP-1 agonists or DPP-4 inhibitors on pathophysiology of heart failure. Int Heart J. 2015;56(4):372–6.
Ihara M, Asanuma H, Yamazaki S, Kato H, Asano Y, Shinozaki Y, et al. An interaction between glucagon-like peptide-1 and adenosine contributes to cardioprotection of a dipeptidyl peptidase 4 inhibitor from myocardial ischemia-reperfusion injury. Am J Physiol Heart Circ Physiol. 2015;308(10):H1287–97.
Aoyama M, Kawase H, Bando YK, Monji A, Murohara T. Dipeptidyl peptidase 4 inhibition alleviates shortage of circulating glucagon-like Peptide-1 in heart failure and mitigates myocardial remodeling and apoptosis via the exchange protein directly activated by cyclic AMP 1/Ras-related protein 1 Axis. Circ Heart Fail. 2016;9(1):e002081.
Pyke C, Heller RS, Kirk RK, Orskov C, Reedtz-Runge S, Kaastrup P, et al. GLP-1 receptor localization in monkey and human tissue: novel distribution revealed with extensively validated monoclonal antibody. Endocrinology. 2014;155(4):1280–90.
Takashima S, Fujita H, Fujishima H, Shimizu T, Sato T, Morii T, et al. Stromal cell-derived factor-1 is upregulated by dipeptidyl peptidase-4 inhibition and has protective roles in progressive diabetic nephropathy. Kidney Int. 2016;90(4):783–96.
Kim M, Platt MJ, Shibasaki T, Quaggin SE, Backx PH, Seino S, et al. GLP-1 receptor activation and Epac2 link atrial natriuretic peptide secretion to control of blood pressure. Nat Med. 2013;19(5):567–75.
Lee MY, Tsai KB, Hsu JH, Shin SJ, Wu JR, Yeh JL. Liraglutide prevents and reverses monocrotaline-induced pulmonary arterial hypertension by suppressing ET-1 and enhancing eNOS/sGC/PKG pathways. Sci Rep. 2016;6:31788.
Acknowledgments
We gratefully acknowledge Ms. M. Yoda, Ms. M. Takahashi, Ms. R. Umezawa, and Ms. M. Saida for their secretarial assistance.
Funding
This study was conducted with funding provided by the Mitsubishi Tanabe Pharma Corporation.
Author information
Authors and Affiliations
Consortia
Contributions
MI conceived the study. MI and SI wrote the manuscript. TH performed statistical analyses and provided the biostatistical study design. MK conceived and supervised the study and is the Principal Investigator on the grant. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
Persons from Mitsubishi Tanabe Pharma Corporation were not involved in conducting this study and analysis, and the intentions of Mitsubishi Tanabe Pharma Corporation are not reflected in the results or interpretations of this study.
Disclosure
Drs. Imadu, Ito, and Hamasaki have nothing to disclose. Dr. Nakano is now an employee of GlaxoSmithKline K.K. Dr. Kitakaze reports receiving grants from the Japanese government during the course of the study: grants from the Japanese government, grants from the Japan Heart Foundation, grants from the Japan Cardiovascular Research Foundation, grants and personal fees from Asteras, personal fees from Daiichi-sankyo, grants and personal fees from Pfizer, grants and personal fees from Ono, personal fees from Bayer, grants from Novartis, grants and personal fees from Mitubishi Tanabe Pharma, personal fees from Kowa, personal fees from MSD, grants from Nihon Kohden, personal fees from Shionogi, personal fees from AstraZeneca, grants and personal fees from AstraZeneca, personal fees from Taisho-Toyama, personal fees from Toyama-Kagaku, grants and personal fees from Kureha, and personal fees from Toaeiyo, outside of the currently proposed work.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Imazu, M., Nakano, A., Ito, S. et al. Effects of Teneligliptin on the Progressive Left Ventricular Diastolic Dysfunction in Patients with Type 2 Diabetes Mellitus in Open-Label, Marker-Stratified Randomized, Parallel-Group Comparison, Standard Treatment-Controlled Multicenter Trial (TOPLEVEL Study): Rationale and Study Design. Cardiovasc Drugs Ther 33, 363–370 (2019). https://doi.org/10.1007/s10557-019-06871-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10557-019-06871-3