Abstract
Purpose
Studies of prognosis following acute myocardial infarction (AMI) conventionally examine the first recurrent coronary heart disease (CHD) event which may not adequately characterize the full burden of CHD hospitalizations. We therefore examined the cumulative number of CHD rehospitalizations following AMI among older adults in the United States.
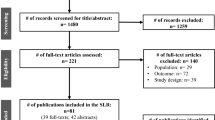
Methods
We conducted a retrospective cohort study of 78,085 Medicare beneficiaries aged ≥66 years without recent CHD history who were hospitalized for AMI in 2000–2010. Counts of CHD rehospitalizations over a maximum of 10 years of follow-up were calculated. Characteristics were assessed through claims and enrollment information and associations with CHD rehospitalizations were evaluated using Poisson models.
Results
Over 25 % of beneficiaries were aged ≥85 years, 55 % were women, and 89 % were white. Comorbidities were common, including diabetes (22.9 %), hypertension (46.7 %), heart failure (10.3 %), and chronic obstructive pulmonary disease (19.2 %). Following AMI, 16,078 beneficiaries (20.6 %) were hospitalized for CHD a total of 23,132 times. Among those who experienced at least one CHD rehospitalization, 35.9 % had ≥2 CHD rehospitalizations (n = 5773, 7.4 % of all beneficiaries with AMI) in the ensuing decade. Associations of demographics, comorbidities, and index hospitalization characteristics with rates of first and total CHD rehospitalizations were largely similar. Age ≥85 years versus 66–69 years was more strongly associated with first (rate ratio [RR] 1.43) than total (RR 1.35) CHD rehospitalization (p < 0.05), as was male versus female sex (RR 1.13 and 1.07).
Conclusions
Emphasizing the first recurrent CHD rehospitalization underestimates the burden of disease experienced among older adults with AMI.


Similar content being viewed by others
References
Rao SR, Schoenfeld DA. Survival methods. Circulation. 2007;115(1):109–13.
Nissen SE. Cardiovascular outcomes in randomized trials: should time to first event for “hard” end points remain the standard approach? J Am Coll Cardiol. 2009;54(25):2363–5.
Smith SC, Benjamin EJ, Bonow RO, Braun LT, Creager MA, Franklin BA, et al. AHA/ACCF secondary prevention and risk reduction therapy for patients with coronary and other atherosclerotic vascular disease: 2011 Update: a guideline from the American Heart Association and American College of Cardiology Foundation. Circulation. 2011;124(22):2458–73.
Stone NJ, Robinson J, Lichtenstein AH, Merz CNB, Blum CB, Eckel RH et al. 2013 ACC/AHA Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2013.
Eckel RH, Jakicic JM, Ard JD, de Jesus JM, Houston Miller N, Hubbard VS, et al. 2013 AHA/ACC guideline on lifestyle management to reduce cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129(25 suppl 2):S76–99.
Eagle KA, Lim MJ, Dabbous OH, Pieper KS, Goldberg RJ, Van de Werf F, et al. A validated prediction model for all forms of acute coronary syndrome: estimating the risk of 6-month postdischarge death in an international registry. JAMA. 2004;291(22):2727–33.
Anavekar NS, McMurray JJ, Velazquez EJ, Solomon SD, Kober L, Rouleau JL, et al. Relation between renal dysfunction and cardiovascular outcomes after myocardial infarction. N Engl J Med. 2004;351(13):1285–95.
Murphy SA, Cannon CP, Wiviott SD, McCabe CH, Braunwald E. Reduction in recurrent cardiovascular events with intensive lipid-lowering statin therapy compared with moderate lipid-lowering statin therapy after acute coronary syndromes from the PROVE IT-TIMI 22 (Pravastatin or Atorvastatin Evaluation and Infection Therapy-Thrombolysis In Myocardial Infarction 22) trial. J Am Coll Cardiol. 2009;54(25):2358–62.
Tikkanen MJ, Szarek M, Fayyad R, Holme I, Cater NB, Faergeman O, et al. Total cardiovascular disease burden: comparing intensive with moderate statin therapy insights from the IDEAL (Incremental Decrease in End Points Through Aggressive Lipid Lowering) trial. J Am Coll Cardiol. 2009;54(25):2353–7.
Kent ST, Safford MM, Zhao H, Levitan EB, Curtis JR, Kilpatrick RD, et al. Optimal use of available claims to identify a medicare population free of coronary heart disease. Am J Epidemiol. 2015;182(9):808–19.
Kiyota Y, Schneeweiss S, Glynn RJ, Cannuscio CC, Avorn J, Solomon DH. Accuracy of medicare claims-based diagnosis of acute myocardial infarction: estimating positive predictive value on the basis of review of hospital records. Am Heart J. 2004;148(1):99–104.
Gooley TA, Leisenring W, Crowley J, Storer BE. Estimation of failure probabilities in the presence of competing risks: new representations of old estimators. Stat Med. 1999;18(6):695–706.
Davison AC, Hinkley DV. Bootstrap methods and their application. New York: Cambridge University Press; 1997.
Prentice RL, Williams BJ, Peterson AV. On the regression analysis of multivariate failure time data. Biometrika. 1981;68(2):373–9.
Box-Steffensmeier JM, De Boef S. Repeated events survival models: the conditional frailty model. Stat Med. 2006;25(20):3518–33.
Rogers JK, Pocock SJ, McMurray JJ, Granger CB, Michelson EL, Ostergren J, et al. Analysing recurrent hospitalizations in heart failure: a review of statistical methodology, with application to CHARM-Preserved. Eur J Heart Fail. 2014;16(1):33–40.
Borer JS, Bohm M, Ford I, Komajda M, Tavazzi L, Sendon JL, et al. Effect of ivabradine on recurrent hospitalization for worsening heart failure in patients with chronic systolic heart failure: the SHIFT Study. Eur Heart J. 2012;33(22):2813–20.
Anderson JL, Heidenreich PA, Barnett PG, Creager MA, Fonarow GC, Gibbons RJ, et al. ACC/AHA statement on cost/value methodology in clinical practice guidelines and performance measures: a report of the American College of Cardiology/American Heart Association Task Force on Performance Measures and Task Force on Practice Guidelines. Circulation. 2014;129(22):2329–45.
Weintraub WS, Cohen DJ. The limits of cost-effectiveness analysis. Circ: Cardiovasc Qual Outcomes. 2009;2(1):55–8.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding Sources
This research, including design and conduct of the study, analysis and interpretation of the data, and preparation of the manuscript, was supported through an academic collaboration between University of Alabama at Birmingham, Icahn School of Medicine at Mount Sinai and Amgen Inc. The funders provided comments on the design and interpretation of this work. The academic authors conducted all analyses and maintained the rights to publish this manuscript.
Conflict of Interest
EBL, PM, LC, LD, MLK, DB, SPG, MMS, GH, and RSR report research support from Amgen Inc. EBL reports consulting for Amgen and Robinson Calcagnie Robinson Shapiro Davis. RK reports employment by Amgen Inc and Baxter BioScience.
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(DOCX 63 kb)
Rights and permissions
About this article
Cite this article
Levitan, E.B., Muntner, P., Chen, L. et al. Burden of Coronary Heart Disease Rehospitalizations Following Acute Myocardial Infarction in Older Adults. Cardiovasc Drugs Ther 30, 323–331 (2016). https://doi.org/10.1007/s10557-016-6653-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10557-016-6653-6