Abstract
Purpose
Angiotensin II type 1 receptor blockers (ARBs) are widely used in treating hypertension. In the present study, we tested the hypothesis that a novel ARB, azilsartan medoxomil (AZL-M) will prevent renal and cardiovascular injury in the spontaneously hypertensive obese rat (SHROB), a model of cardiometabolic syndrome.
Methods
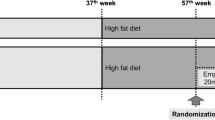
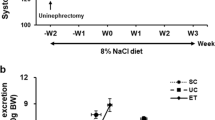
Male SHROB were treated with vehicle or AZL-M orally for 56 days. Vehicle treated normotensive Wistar-Kyoto (WKY) rats served as controls. The effects of AZL-M on kidney injury, vascular endothelial and heart functions, lipid profile, and glucose tolerance were assessed.
Results
AZL-M demonstrated anti-hypertensive effects along with markedly improved vascular endothelial function in SHROB. In these rats, AZL-M demonstrates strong kidney protective effects with lower albuminuria and nephrinuria along with reduced tubular cast formation and glomerular injury. AZL-M treatment also improved left ventricular heart function, attenuated development of left ventricular hypertrophy, and reduced cardiac fibrosis in SHROB.
Conclusion
Overall, these findings demonstrate kidney and heart protective effects of AZL-M in SHROB, and these effects were associated with its ability to lower blood pressure and improve endothelial function.







Similar content being viewed by others
References
Paul M, Poyan Mehr A, Kreutz R. Physiology of local renin-angiotensin system. Physiol Rev. 2008;86:747–803.
Iwanami J, Mogi M, Iwai M, Horiuchi M. Inhibition of renin-angiotensin system and target organ protection. Hypertens Res. 2009;32:229–37.
Cole BK, Keller SR, Wu R, Carter JD, Nadler JL, Numemaker CS. Valsartan protects pancreatic islets and adipose tissue from the inflammatory and metabolic consequences of a high-fat diet in mice. Hypertens. 2010;55:715–21.
Sofue T, Kiyomoto H. Angiotensin II receptor blocker is a renoprotective remedy for metabolic syndrome. Hypertens Res. 2009;32:735–7.
Elmarakby AA, Imig JD. Obesity is the major contributor to vascular dysfunction and inflammation in high-fat diet hypertensive rats. Clin Sci Lond. 2010;118:291–301.
Weir MR. The renoprotective effects of RAS inhibition: focus on prevention and treatment of chronic kidney disease. Postgrad Med. 2009;121:96–103.
Wassmann S, Laufs U, Bäumer AT, Müller K, Ahlbory K, Linz W, et al. MHG-CoA reductase inhibitors improve endothelial dysfunction in normocholesterolemic hypertension via reduced production of reactive oxygen species. Hypertens. 2001;37:1450–7.
Vieira Jr JM, Rodrigues LT, Mantovani E, Dellê H, Mattar AL, Malheiros DM, et al. Statin monotherapy attenuates renal injury in a salt-sensitive hypertension model of renal disease. Nephron Physiol. 2005;101:82–91.
Baker WL, White WB. Azilsartan medoxomil: a new angiotensin II receptor antagonist for treatment of hypertension. Ann Pharmacother. 2011;45:1506–15.
Vople M, Savoia C. New treatment options in the management of hypertension: appraising the potential role of azilsartan medoxomil. Integr Blood Press Control. 2012;5:19–25.
Kohara Y, Kubo K, Imamiya E, Wada T, Inada Y, Naka T. Synthesis and angiotensin II receptor antagonist activities of benzimidazole derivatives bearing acidic heterocycles as novel tetrazolebioisosteres. J Med Chem. 1996;39:5228–35.
Ojima M, Igata H, Tanaka M, Sakamoto H, Kuroita T, Kohara Y, et al. In vitro antagonistic properties of a new angiotensin type 1 receptor blocker, azilsartan, in receptor binding and function studies. J Pharmacol Exp Ther. 2011;336:801–8.
Kajiya T, Ho C, Wang J, Vilardi R, Kurtz TW. Molecular and cellular effects of azilsartan: a new generation angiotensin II receptor blocker. J Hypertens. 2011;29:2476–83.
Ye Y, Keyes KT, Zhang CF, Perez-Polo JR, Lin Y, Birnbaum Y. Additive effect of TAK-491, a new angiotensin receptor blocker and pioglitazone, in reducing myocardial infarct size. Cardiovasc Drugs Ther. 2010;24:107–20.
Baumann PQ, Zaman T, McElroy-Yaggy K, Sobel BE. The efficacy and tolerability of azilsartan in mice with left ventricular pressure overload or acute myocardial infarction. J Cardiovasc Pharmacol. 2013;61:437–43.
Kusumoto K, Igata H, Ojima M, Tsuboi A, Imanishi M, Yamaguchi F, et al. Antihypertensive, insulin-sensitising and renoprotective effects of a novel, potent and long-acting angiotensin II type 1 receptor blocker, azilsartan medoxomil, in rat and dog models. Eur J Pharmacol. 2011;669:84–93.
Koletsky. Pathologic findings and laboratory data in a new strain of obese hypertensive rats. Am J Pathol. 1975;80:129–42.
Ernsberger P, Johnson JL, Rosenthal T, Mirelman D, Koletsky RJ. Therapeutic actions of allylmercaptocaptopril and captopril in a rat model of metabolic syndrome. Am J Hypertens. 2007;20:866–74.
Ernsberger P, Koletsky RJ, Friedman JE. Molecular pathology in the obese spontaneous hypertensive Koletsky rat: a model of syndrome X. Ann N Y Acad Sci. 1999;892:272–88.
Imig JD, Walsh KA, Hye Khan MA, Nagasawa T, Cherian-Shaw M, Shaw SM, et al. Soluble epoxide hydrolase inhibition and peroxisome proliferator activated receptor γ agonist improve vascular function and decrease renal injury in hypertensive obese rats. Exp Biol Med. 2012;237:1402–12.
Purves RD. Optimum numerical integration methods for estimation of area-under-the-curve (AUC) and area-under-the-moment-curve (AUMC). J Pharmacokinet Biopharm. 1992;20:211–26.
Scheen AJ. Management of the metabolic syndrome. Minerva Endocrinol. 2004;29:31–45.
White WB, Weber MA, Sica D, Bakris GL, Perez A, Cao C, et al. Effects of the angiotensin receptor blocker azilsartan medoxomil versus olmesartan and valsartan on ambulatory and clinic blood pressure in patients with stages 1 and 2 hypertension. Hypertens. 2011;57:413–20.
Bakris GL, Sica D, Weber M, White WB, Roberts A, Perez A, et al. The comparative effect of azilsartan medoxomil and olmesartan on ambulatory and clinic blood pressure. J Clin Hypertens Greenwich. 2011;13:81–8.
Sueta D, Kataoka K, Koibuchi N, Toyama K, Uekawa K, Katayama T, et al. Novel mechanism for disrupted circadial blood pressure rhythm in a rat model of metabolic syndrome-the critical role of angiotensin II. J Am Heart Assoc. 2013;2:e000035.
Kurtz TW, Kajiya T. Differential pharmacology and benefit/risk of azilsartan compared to other sartans. Vasc Health Risk Manag. 2012;8:133–43.
Galili O, Versari D, Sattler KJ, Olson ML, Mannheim D, McConnell JP, et al. Early experimental obesity is associated with coronary endothelial dysfunction and oxidative stress. Am J Physiol Heart Circ Physiol. 2007;292:H904–11.
Knight SF, Imig JD. Obesity, insulin resistance, and renal function. Microcirc. 2007;14:349–62.
Picchhi A, Gao X, Belmandani S, Potter BJ, Focardi M, Chilian WM, et al. Tumor necrosis factor-α induces endothelial dysfunction in the prediabetic metabolic syndrome. Circ Res. 2006;99:69–77.
Tziomalos K, Athyros VG, Karagiannis A, Mikhailidis DP. Endothelial dysfunction in metabolic syndrome: prevalence, pathogenesis and management. Nutr Metab Cardiovasc Dis. 2010;20:140–6.
Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circ. 2005;112:2735–52.
Negro R. Endothelial effects of antihypertensive treatment: focus on irbesartan. Vasc Health Risk Manag. 2008;4:89–101.
Russell JC, Kelly SE, Vine DF, Proctor SD. Irbesartan-mediated reduction of renal and cardiac damage in insulin resistant JCR:LA-cp rats. Br J Pharmacol. 2009;158:1588–96.
Lee MH, Song HK, Ko GJ, Kang YS, Han SY, Han KH, et al. Angiotensin receptor blockers improve insulin resistance in type 2 diabetic rats by modulating adipose tissue. Kidney Int. 2008;74:890–900.
Rong X, Li Y, Ebihara K, Zhao M, Kusakabe T, Tomita T, et al. Irbesartan treatment up-regulates hepatic expression of PPARα and its target genes in obese Koletsky (fak/fak) rats: a link to amelioration of hypertrigyceridaemia. Br J Pharmacol. 2010;160:1796–807.
Fruchart JC. Peroxisome proliferator-activated receptor-alpha (PPARalpha): at the crossroads of obesity, diabetes and cardiovascular disease. Atheroscler. 2009;205:1–8.
Ecelbarger CM, Rash A, Sinha RK, Tiwari S. The effect of chronic candesartan therapy on the metabolic profile and renal tissue cytokine levels in the obese Zucker rat. Mediat Inflamm. 2010;2010:841343.
Zhao M, Li Y, Wang J, Ebihara K, Rong X, Hosoda K, et al. Azilsartan treatment improves insulin sensitivity in obese spontaneously hypertensive Koletsky rats. Diabetes Obes Metab. 2011;13:1123–9.
Lea J, Cheek D, Thornley-Brown D, Appel L, Agodoa L, Contreras G, et al. AASK Study Investigators. Metabolic syndrome, proteinuria, and the risk of progressive CKD in hypertensive African Americans. Am J Kidney Dis. 2008;51:732–40.
Pugsley MK. The angiotensin-II (AT-II) receptor blocker olmesartan reduces renal damage in animal models of hypertension and diabetes. Proc West Pharmacol Soc. 2005;48:35–8.
Khan MAH, Imig JD. Telmisartan provides better renal protection than valsartan in a rat model of metabolic syndrome. Am J Hypertens. 2011;24:816–21.
Mizuno M, Sada T, Kato M, Koike H. Renoprotective effect of blockade of angiotensin II AT1 receptors in an animal model of type 2 diabetes. Hypertens Res. 2002;25:271–8.
Ishimitsu T, Honda T, Ohno E, Furukata S, Sudo Y, Nakano N, et al. Year-long antihypertensive therapy with candesartan completely prevents development of cardiovascular injuries in spontaneously hypertensive rats. Int Heart J. 2010;51:359–64.
Nakamura Y, Suzuki S, Saitoh S, Takeishi Y. New angiotensin II type 1 receptor blocker, azilsartan, attenuates cardiac remodeling after myocardial infarction. Biol Pharm Bull. 2013;36:1326–31.
Varagic J, Frohlich ED, Susic D, Ahn J, Matavelli L, López B, et al. AT1 receptor antagonism attenuates target organ effects of salt excess in SHRs without affecting pressure. Am J Physiol Heart Circ Physiol. 2008;294:H853–8.
Susic D, Fares H, Frohlich ED. Telmisartan prevents excess-salt-induced exacerbated (malignant) hypertension in spontaneous hypertensive rats. J Cardiovasc Pharmacol Ther. 2013;18:126–32.
Acknowledgments
We thank Katherine A. Walsh and Priyanka Nervatla from Department of Pharmacology & Toxicology, Medical College of Wisconsin for their excellent technical assistance. We also thank Dr Frantisek Papousek from Institute of Physiology, Academy of Science of the Czech Republic for his valuable comments in interpreting echocardiographic data. These studies were supported by a grant from Takeda Pharmaceuticals Inc., USA. Jan Neckář is supported by Czech Science Foundation grant (13-10267S). Md. Abdul Hye Khan is supported by a Postdoctoral Fellowship from the Midwest Affiliate of the American Heart Association.
Disclosure
No conflicts of interest, financial or otherwise, are declared by the author(s).
Author’s contribution
Md. Abdul Hye Khan designed the study, performed experiments, analyzed data and wrote the manuscript. Jan Neckář designed the study, performed experiments, analyzed data and wrote the manuscript. John D. Imig designed the study and wrote the manuscript. Breana Cummens and Geneva M. Wahl performed experiments, analyzed the data. All authors have thoroughly read the manuscript, agreed on the data interpretation, and approved the final draft submitted.
Author information
Authors and Affiliations
Corresponding author
Additional information
Md. Abdul Hye Khan and Jan Neckář contributed equally to the work.
Rights and permissions
About this article
Cite this article
Khan, M.A.H., Neckář, J., Cummens, B. et al. Azilsartan Decreases Renal and Cardiovascular Injury in the Spontaneously Hypertensive Obese Rat. Cardiovasc Drugs Ther 28, 313–322 (2014). https://doi.org/10.1007/s10557-014-6530-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10557-014-6530-0