Abstract
EpCAM (epithelial cell adhesion molecule) was discovered four decades ago as a tumor antigen on colorectal carcinomas. Owing to its frequent and high expression on carcinomas and their metastases, EpCAM serves as a prognostic marker, a therapeutic target, and an anchor molecule on circulating and disseminated tumor cells (CTCs/DTCs), which are considered the major source for metastatic cancer cells. Today, EpCAM is reckoned as a multi-functional transmembrane protein involved in the regulation of cell adhesion, proliferation, migration, stemness, and epithelial-to-mesenchymal transition (EMT) of carcinoma cells. To fulfill these functions, EpCAM is instrumental in intra- and intercellular signaling as a full-length molecule and following regulated intramembrane proteolysis, generating functionally active extra- and intracellular fragments. Intact EpCAM and its proteolytic fragments interact with claudins, CD44, E-cadherin, epidermal growth factor receptor (EGFR), and intracellular signaling components of the WNT and Ras/Raf pathways, respectively. This plethora of functions contributes to shaping intratumor heterogeneity and partial EMT, which are major determinants of the clinical outcome of carcinoma patients. EpCAM represents a marker for the epithelial status of primary and systemic tumor cells and emerges as a measure for the metastatic capacity of CTCs. Consequentially, EpCAM has reclaimed potential as a prognostic marker and target on primary and systemic tumor cells.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
The epithelial cell adhesion molecule (EpCAM) has first been described in 1979 as a humoral antigen expressed on colon carcinoma cells [1]. Here, we have summarized the impressive progress in the biology of EpCAM in the past four decades. Expression patterns, regulation, and the multiple functions of EpCAM in normal epithelia, in carcinoma, and in pluripotent stem cells are reviewed. Furthermore, the clinical implications and applications related to EpCAM are discussed. Lastly, the most recently discovered involvement of EpCAM in the regulation of epithelial-to-mesenchymal transition, which is of paramount importance during metastases formation and therapy resistance, is delineated.
1.1 Initial description
EpCAM was first described in 1979 as a humoral antigen recognized by monoclonal antibody 1083-17-1A (Co17-1A or mAb 17-1A) following inoculation of human colorectal cancer cells in mice [1]. Today, PubMed-listed publications on “EpCAM” exceed 8000 entries. Publications have steadily increased (Fig. 1) reflecting an enhanced interest in EpCAM along with broadening functional roles.
Publication numbers retrieved from PubMed using “EpCAM” as a search term. Two time points of increase in publication numbers are marked by dashed lines. The first wave of increased publications maps to the cloning of the EpCAM cDNA in 1989. The second wave coincides with the description of EpCAM function in proliferation and migration in 2004
1.2 EpCAM cDNA cloning and protein structure
The coding sequence of human EpCAM was deciphered in 1989 and predicted a single transmembrane protein of 314 amino acids (aa) with a 265-aa extracellular domain, a 23-aa hydrophobic transmembrane domain, and a hydrophilic 26-aa intracellular domain [2]. In 2014, the crystal structure of the extracellular domain of EpCAM was resolved and was shown to represent heart-shaped homodimers [3].
1.3 Cell adhesion
The first function as a homophilic cell adhesion molecule and a role in the integrity of epithelium was proposed in conjunction with the name EpCAM by Litvinov et al. [4]. They reported that ectopic expression of EpCAM in murine fibroblasts and mouse mammary carcinoma cells induced clustering and segregation of cells and reduced invasive growth. Later on, inhibitory activity towards cadherin-mediated adhesion in epithelial cells was reported [5].
1.4 Proliferation and differentiation
First evidence for a correlation of EpCAM in proliferation and differentiation surfaced in 1994 [6] and 1996 [7] in keratinocytes, transformed epithelial cells, and carcinoma cell lines. In 2004, a role for EpCAM in the regulation of proliferation, migration, and invasion was shown [8, 9]. A role of EpCAM in differentiation was reported in pluripotent embryonic stem cells (ESCs), progenitor cells, and carcinoma stem cells [10].
1.5 Clinical significance in cancer
Frequent and high-level expression of EpCAM on various carcinomas (98 out of 131 tested) [11, 12] and metastases [13, 14], and a correlation with clinical outcome qualified it as prognostic marker and therapeutic target [15]. EpCAM-specific antibody Panorex® (edrecolomab; 17-1A) first attained market approval for treating colorectal carcinomas in 1995 [16]. Furthermore, EpCAM served to enrich, identify, and characterize metastatic cells that have disseminated from primary tumor into blood and bone marrow of advanced carcinoma patients [17, 18]. Despite existing challenges, EpCAM remains the surface antigen of choice in clinical use to isolate circulating tumor cells (CTCs) with prognostic value and metastatic potential [15, 19,20,21].
1.6 EpCAM in non-malignant diseases
A major breakthrough in understanding congenital tufting enteropathy (CTE), a severe form of early-onset autosomal recessive diarrhea, was achieved when Mamata Sivagnanam and colleagues reported on the linkage of CTE with mutations in the EPCAM gene that precluded its correct expression at the plasma membrane [22]. Lack of EpCAM expression results in villus atrophy and in the formation of intestinal tufts, which eventually induces a dysfunctional intestinal barrier and unbalanced ion transport [23, 24].
Furthermore, mutations in the 3′-end of the EPCAM gene induce epigenetic silencing of genes downstream of EPCAM that are involved in mismatch repair, including the MutL homolog 1 (MLH1) and MutS protein homolog 2 (MSH2) genes. EPCAM 3′-mutations and subsequent deregulation of MLH1 and MSH2 protein expression are the cause of Lynch syndrome (hereditary non-polyposis colorectal cancer (HNPCC)) [25, 26].
A chronic of major advances on EpCAM in basic research and clinical application is summarized in Fig. 2.
2 EpCAM gene and protein structure
The human EPCAM gene is encoded on the plus strand of chromosome 2p21 and consists of 9 exons covering 41.88 kilobases (kb). Exon 1 encodes the 5′-untranslated region and the signal peptide, exon 2 the EGF-like motif, exon 3 the thyroglobulin domain, exons 4–6 the cysteine-poor part of the domain, exon 7 the transmembrane domain, exon 8 parts of the intracellular domain, and exon 9 the remaining intracellular domain and the 3′-untranslated region [27]. A 1.1-kb fragment of the EPCAM promoter sufficient to drive gene expression and confers epithelial specificity was cloned [28, 29]. The promoter can be further subdivided in a gene proximal part composed of 570 base pairs (bp) and a distal part of 550 bp that act synergistically in EPCAM expression and are negatively regulated by nuclear factor kappa B (NF-κB) [29]. Sankpal et al. further described the usage of an extracellular-regulated kinase 2 (ERK2) binding site within the EPCAM promoter [30], while Yamashita et al. reported on the regulation of the EPCAM promoter by a Wnt-β-catenin-Tcf4 complex in hepatocellular carcinoma cells [31]. Furthermore, the EMT-inducing transcription factor Zeb1 represses EPCAM expression in zebrafish [32].
EpCAM is a transmembrane protein with a single membrane-spanning domain (23-aa) that connects the larger extracellular domain (265-aa) to a short intracellular domain (26-aa) (Fig. 3). The extracellular domain contains a signal peptide, an EGF-like, cysteine-rich domain, and a thyroglobulin-like domain, which was initially referred to as a second EGF-like repeat [36], followed by a cysteine-poor region [37]. Mass spectrometry and Edman sequencing of the extracellular domain of EpCAM demonstrated the cleavage of the signal peptide after aa 23, resulting in an N-terminus starting with a modified pyroglutamate [38]. Disulfide bonds were mapped to Cys27–Cys46, Cys29–Cys59, Cys38–Cys48, Cys110–Cys116, and Cys118–Cys135 (Fig. 3) [38].
Schematic representation of the EpCAM protein. EpCAM is composed of a signal peptide (SP) that is removed from the mature protein. Mature EpCAM comprises an extracellular domain (EpEX), a single transmembrane domain (TMD), and a short intracellular domain (EpICD). N-Terminal (N-domain), thyroglobulin (TY-domain), and C-terminal domains (C-domain) within EpEX, as defined by Pavsic et al. [3], are marked. N- and TY-domains are cysteine-rich protein stretches that have initially been defined as EGF-like domains. Disulfide bonds involving cysteines, N-glycosylation at asparagines, ubiquitylation at lysines, and cleavage sites related to regulated intramembrane proteolysis of EpCAM (α-, β-, γ-, and ε-sites) [33, 34] are annotated. The approximated additional cleavage site reported by Schnell et al. [35] is indicated. Sizes are not at scale
N-Glycosylation of EpCAM has been reported with no evidence of O-glycosylation [2]. N-Glycosylation sites have been mapped to Asn74, Asn111, and Asn198 of EpCAM [38]. Initially complete glycosylation of Asn111, partial glycosylation of Asn74, and no glycosylation at Asn198 were reported [38]. However, single and dual mutations of Asn74 and Asn111 revealed that mutations retained a certain degree of glycosylation, which was lost when all positions including Asn198 were mutated [39]. Loss of glycosylation at this site resulted in severe reduction of protein stability and half-life at the membrane from 21 to 7 h [39]. Glycosylation of EpCAM may impact on EpCAM stability and expression in tumor cells, as it was found increased in cancerous versus healthy tissue [40].
Crystal structure analysis of the extracellular domain of EpCAM, termed EpEX, at 1.86 Å resolution revealed a three-partite fold in amino-terminal (puroGlu24–Leu62), thyroglobulin-like (Ala63–Arg138), and carboxy-terminal (Val139–Lys265) domains (Fig. 3). The respective ND, TY, and CD domains are each in contact with the other two domains, forming a triangle [3]. EpEX molecules form cis-dimers with strongest interactions between the TY loop of one EpEX molecule with the βC sheet of a second molecule [3]. Coarse grain modelling of the intramembrane domain demonstrated a dimeric structure in which two helices of the membrane-spanning parts are symmetrically arranged and cross each other between Val276 and Val280 [3]. There is so far no structural information of the intracellular domain of EpCAM termed EpICD.
3 EpCAM and cell adhesion
Initial characterization of EpCAM functions was conducted in murine fibroblasts and L153S mammary carcinoma cells, which are characterized by loss of cell adhesion and the adoption of a spindle-shaped morphology. Ectopic expression resulted in increased intercellular adhesion and cell aggregation in suspension, along with the segregation of EpCAM-positive and EpCAM-negative cells, and a reduced capacity of fibroblast to grow invasively [4, 41]. Membrane-proximal thyroglobulin-like domains, initially referred to as a second EGF-like domain, mediate lateral interactions of EpCAM in cis on one cell. Membrane-distal EGF-like repeats are required for interactions of EpCAM in trans on adjacent cells [42]. Taken together, formation of functional EpCAM tetramers as the initiating event in the formation of cell adhesion complexes was proposed [42].
Surprisingly, overexpression of EpCAM in epithelial cell lines that depend on cadherin-mediated cell-cell connections decreased adhesion by impairing functional adherens junctions through disruption of E-cadherin, α-catenin, and F-actin interactions [43, 44]. EpCAM’s capacity to inhibit cadherin-mediated adhesion in breast epithelial cells depended on phosphoinositide 3-kinase (PI3K) and its shifted interaction with N-cadherin to EpCAM [45].
Knockout of EpCAM in mice supported its role in orchestrating the structure and functionality of epithelium in the intestinal tract [46,47,48]. EpCAM knockout induced an abnormal placental development associated with death in utero at gestation day E12.5 [46]. Subsequent knockouts did not reproduce an embryonic lethality; however, mice died of severe intestinal erosion and hemorrhagic diarrhea shortly after birth [44, 45]. Intestinal defects were reminiscent of human CTE where mutations cause a loss of EpCAM expression at the plasma membrane [22, 49]. Despite agreeing on the observed phenotype, Lei et al. [48] and Guerra et al. [47] disagreed on the molecular mechanisms. Lei et al. observed a loss of tight junction formation owing to substantially reduced recruitment of murine claudin 7 to tight junctions in the absence of EpCAM [48]. These findings are supported by the direct interaction of EpCAM with claudin 7 [50], which was demonstrated to support tumor progression in colorectal cancer [51, 52]. Guerra et al. demonstrated a dysregulation of E-cadherin and ß-catenin functions leading to partial disruption of adherens junctions [47]. A cooperation of E-cadherin and EpCAM in epithelial adhesion regulation is further supported by work in zebrafish, where EpCAM knockout impaired the integrity of the skin periderm through reduced cell surface levels of E-cadherin and increased levels of tight junction protein 1 (Tjp1) [53].
More discrepancies exist on EpCAM’s role in cell-cell adhesion. Gaber et al. [54] could not confirm intercellular homo-oligomers, despite formation of cis-dimers [54], leading to the conclusion that EpCAM’s role in adhesion is not assumed as a homophilic cell adhesion molecule. Furthermore, neither regulated intramembrane proteolysis of EpCAM nor EPCAM knockout in cell lines had any measurable impact on cell-matrix and cell-cell adhesion in cancer cells [33]. Hence, EpCAM’s molecular function in adhesion has not been satisfactorily resolved yet. EpCAM is undeniably involved in maintenance of epithelial integrity in various animal models and human conditions where it acts in concert with established cell adhesion molecules. Therefore, EpCAM might support cell adhesion primarily mediated by other molecules such as claudins and cadherins, and/or might preferentially play a role in adhesion of normal but not tumor cells.
4 EpCAM as a prognostic marker in cancer
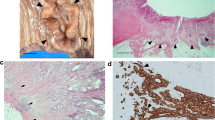
EpCAM received considerable attention as a prognostic marker based on its strong expression in various carcinomas and their metastases as compared to normal epithelia of the same localization [11,12,13]. EpCAM is highly and frequently expressed in the vast majority of carcinomas that have been analyzed [11, 12] and its expression in metastases frequently correlates with levels in the corresponding primary tumors (Fig. 4 and [13, 14, 21, 55]). As such, EpCAM bears potential as a prognostic and therapeutic marker in carcinomas and during cancer progression and metastasis formation. However, EpCAM’s prognostic value varies depending on the tumor entity. High expression in primary carcinomas is associated with poor prognosis in breast [56, 57], colorectal [58], prostate [59], gallbladder [60], ovarian [61], bladder [62], pancreas [63, 64], and adenoid cystic carcinomas [65]. Oppositely, high expression of EpCAM is associated with better prognosis in colonic [12], esophageal [66], renal [67, 68], gastric [69], endometrial [70], thyroid [71], and head and neck carcinomas [72]. Multiple cellular functions of EpCAM may deploy in dependency of tumor types and localization, and might differently affect single cells within tumors. High expression of EpCAM can promote sustained proliferation and tumor/metastatic growth and might thereby be associated with poor prognosis. EpCAM also represents a marker of epithelial differentiation and might therefore associate with a more differentiated, less migratory/invasive phenotypes, with reduced resistance to irradiation and chemotherapy, and hence with better survival. Therefore, EpCAM’s association with differential clinical outcome is complex and might vary depending on the origin of the tumor or even the stage of tumor progression. This unsolved discrepancy in the prognostic value of EpCAM expression remains poorly understood and requires further investigation.
Another essential aspect is that cancer-related lethality is primarily caused by therapy-resistant cells and frequently untreatable metastases. Numerous studies on EpCAM’s prognostic value have initially concentrated on primary tumors rather than disseminated cells [12, 57,58,59,60,61,62,63,64,65, 67,68,69,70,71,72,73]. However, primary tumor biopsies represent a specific region of the tumor at a given time point. Based on growing evidence of intratumor heterogeneity and temporal variation in tumor antigen expression [74,75,76,77,78,79,80], a singular measurement of primary tumors might suffer from bias. Consequently, numbers of disseminated tumor cells, which are considered primary sources of relapse and metastases, have been implemented as additional prognostic marker [81,82,83]. Here, tumor cells found in the blood are termed circulating tumor cells (CTCs) and tumor cells in distant organs, for example, in the bone marrow, are termed disseminated tumor cells (DTCs). Clinical assessment of CTCs in the blood is minimally invasive and allows for longitudinal measurements [82, 84] and aims at the prediction of metastasis formation [19]. Measurement of CTCs in the blood of metastatic breast cancer (MCB) patients was performed using EpCAM-specific antibodies for the enrichment of rare circulating tumor cells, which were subsequently further characterized by the expression of cytokeratins, presence of a nucleus, and lack of white blood cell marker CD45. CTC numbers in the blood showed prognostic value and patients with five CTCs or more per 7.5 mL blood had decreased overall and progression-free survival [18]. More recently, 3173 patients with non-metastatic (stages I–III) breast cancer were analyzed and a CTC threshold of ≥ 1 cell per 7.5 mL of blood correlated with decreased OS, disease-free survival, distant disease-free survival, and cancer-specific survival [85]. The prognostic value of EpCAM-positive CTCs has been confirmed for further tumor entities, including lung cancer [86], advanced ovarian cancer [87], gastric cancer [88], colorectal cancer [89], and head and neck squamous cell carcinoma (HNSCC) [90]. Hence, the enrichment of rare EpCAM-positive systemic tumor cells in the blood in the frame of liquid biopsies has the potential to evaluate disease outcome including the patients’ burden of metastatic cells [20, 21, 85].
5 EpCAM as a target in clinical trials for cancer therapy
EpCAM is highly and frequently expressed in the vast majority of carcinomas, in tumor-initiating cells, and in disseminated tumor cells, which qualified EpCAM as a potential target for cancer therapies [15, 91, 92]. Several publications demonstrated that EpCAM-specific antibodies can eliminate cancer cells by various mechanisms [93,94,95,96,97,98,99,100,101,102] and detect DTC in the bone marrow of patients [103, 104]. Monoclonal antibody 17-1A was clinically tested alone and in combination with γ-interferon for the treatment of gastrointestinal and metastasized colorectal carcinomas [105, 106]. Induction of complete remissions by mAb 17-1A were reported in metastasized colorectal cancer [107, 108]. Positive overall survival data with mAb 17-1A in a pivotal study with metastasized colorectal cancer patients [96, 99] resulted in approval of the antibody in Germany under the trade name Panorex®. However, when compared to standard care with 5-fluorouracil-based chemotherapy in a later trial [109], edrecolomab was found inferior, leading to its market withdrawal. EpCAM-specific humanized antibodies ING-1 and 3622W94, bearing higher binding affinity than edrecolomab, were tested in clinical trials but were discontinued because of low tolerability. While edrecolomab might have suffered from an insufficient binding affinity, ING-1 and 3622W94 displayed too high affinity that no longer allowed to distinguish normal and malignant cells, leading to pancreatitis [110, 111].
Micromet Inc. developed fully human IgG1 EpCAM-specific antibody MT201 (adecatumumab) that had an intermediate binding affinity for EpCAM in an attempt to improve therapeutic efficacy [112]. Adecatumumab was investigated as monotherapy in a phase II clinical trial in MBC patients. Adecatumumab did not induce measurable tumor regression; however, patients treated with high-dose antibody and expressing high levels of EpCAM retrospectively showed reduced development of new metastases (3/18 versus 14/29 patients) [113]. In a dose-escalating phase I trial enrolling prostate cancer patients, reduction of prostate-specific antigen levels was observed [114]. While having a favorable safety profile, the antibody program is no longer pursued because it did not reach its clinical endpoints.
EpCAM was also targeted with T cell-engaging antibodies designed to connect cytotoxic T cells with cancer cells for redirected lysis. Antibody catumaxomab (Removab®) developed by Trion Pharma has an EpCAM- and a CD3-binding arm and its Fc domain binds Fc gamma-receptor expressing antigen-presenting cells [115]. Catumaxomab was approved by the European Medicines Agency (EMA) to treat malignant ascites [116], but was eventually terminated. MT110 (solitomab) is a tandem single-chain antibody construct comprised of an EpCAM- and CD3-specific binding domain developed by Micromet Inc. [117]. Pharmacokinetics, tolerability, safety, and anti-tumor activity of MT110 were assessed in a dose-escalating phase I clinical trial in metastatic colorectal, gastric, and lung carcinomas (129) with disease stabilization in 7/19 patients. Due to gastrointestinal toxicities, solitomab could not be escalated to more efficacious dose levels, and the program was abandoned.
Recently, EpCAM-specific antibody EpAb2-6 was developed, which binds to an epitope within the thyroglobulin domain and demonstrated inhibitory potential [118]. EpAb2-6 induces apoptosis, inhibits tumor growth in mouse models, and represses EpCAM cleavage to form the signaling moiety EpICD in pancreatic and colon carcinoma cells [118, 119]. Thus, EpAb2-6 is an anti-EpCAM antibody that inhibits central EpCAM signaling functions, which might represent a novel approach to treatment methods targeting EpCAM in carcinomas. Furthermore, EpCAM-specific antibodies were conjugated with bouganin (citatuzumab bogatox) [120], Pseudomonas exotoxin A (oportuzumab monatox) [121] and alpha-amanitin [122], with interleukin-2 to activate T cells in the vicinity of EpCAM-positive tumor cells (huKS-IL2) [123], and with encapsulated inhibitory RNAs [124,125,126]. In 2015, a phase I clinical trial of patients with EpCAM-positive metastatic cancers aimed at evaluating the maximum tolerated doses, pharmacokinetics, and immunogenicity of the anti-EpCAM-based immunotoxin MOC31PE that is coupled to Pseudomonas exotoxin A. MOC31PE was intravenously combined with the immunosuppressant cyclosporin in n = 63 metastatic patients and revealed a safe profile with a half-life in plasma of 3 h and a reduction of [127]. Subsequently, MOC31PE was applied to address peritoneal metastasis in colorectal and ovarian cancers within the ImmunoPeCa phase I/II. Based on the promising cytotoxicity profile and a low systemic uptake, MOC31PE is currently further evaluated in a clinical phase II study [128, 129].
Further clinical trials including the usage of chimeric antigen receptor T cells (CAR T cells) targeting EpCAM are ongoing in order to address their potential for the treatment of recurrent and treatment-resistant solid tumors (https://clinicaltrials.gov/ct2/show/NCT04151186). Currently, a total of 64 clinical trials are listed by the US national library of medicine that involve EpCAM as a biological using CAR T cells, monoclonal antibodies, immunotoxins and immunocytokines, and EpCAM-based capture methods to enrich CTCs (https://clinicaltrials.gov/ct2/results?cond=&term=EpCAM&cntry=&state=&city=&dist=). While EpCAM expression on most carcinoma is a highly attractive feature for tumor-associated antigens, expression on healthy epithelia—mostly of the gastrointestinal tract—will limit the therapeutic window of EpCAM-targeted therapies and call for potential side effects. A next generation of EpCAM-targeted drugs that are selectively activated in the tumor microenvironment may finally allow to leverage this target antigen [130].
Finally, EpCAM serves as a target for image-guided surgery approaches that aim at improving resection margins. Residual tumor cells following incomplete tumor removal at the resection margin are a major source of local recurrence in solid tumors [131]. The employed strategies include the systemic application of EpCAM-specific antibodies labeled with fluorescent dyes such as fluorescein isothiocyanate (FITC) and near-infrared fluorescence dye (NIRF) IRDye800CW [132, 133]. Fluorescence-labeled anti-EpCAM antibodies allow the detection of residual tumor nodules in the millimeter size range using intraoperative imaging systems [133, 134].
6 Signaling of EpCAM
6.1 RIP-mediated EpCAM signaling
EpCAM regulates cell cycle progression and differentiation via regulated intramembrane proteolysis (RIP). Initial cleavage of EpCAM is conducted by membrane-resident ADAM (a disintegrin and metalloproteinase) family proteases ADAM 10 and 17 (Fig. 5). Thereby, the ectodomain of EpCAM is shed into the extracellular space as soluble EpEX [135]. The resulting membrane-tethered C-terminal fragment (EpCAM-CTF) is cleaved by the γ-secretase complex to form the extracellular, small, and soluble Aβ-like fragment and the intracellular EpICD fragment [33, 34, 135]. EpICD translocates into the nucleus and, in combination with transcription factors and adaptor molecules such as FHL2, β-catenin, and Lef1, binds to promoter regions of regulators of cell division (cyclin D1 [136]), pluripotency genes [137,138,139], and genes involved in the regulation of EMT-associated processes such as tight junctions, adherence, and cell migration [140]. However, regulation of EpCAM cleavage and EpICD signaling through activation of EGFR remains a matter of dispute [140,141,142,143].
Schematic representation of the signaling mechanisms associated with EpCAM. Signaling by EpCAM and degradation of EpCAM via regulated intramembrane proteolysis (RIP) is depicted in the left part of the scheme. Membrane-associated signaling, trafficking, and intracellular RIP in endocytic vesicles are depicted on the right part. Effects of distinct pathways and the associated molecules are color-coded and implemented in the schematic representation of the cell nucleus
Interactions between ADAM 10 and EpCAM in the tetraspanin web of human colon cancer cells were reported before EpCAM RIP [144]. A role for ADAM 17 (tumor necrosis factor-α-converting enzyme (TACE)) in EpCAM RIP was demonstrated using biochemical approaches and TACE inhibitors [135]. Chemical inhibition of ADAMs and TACE knockdown prevented the first cleavage and reduced EpCAM’s proliferative effects, which were restored through ectopic expression of EpICD [135, 136]. Cleavage sites for ADAM proteases (α-sites) were determined in human and mouse EpCAM [33, 34]. Murine EpCAM has one major α-site (serine230/lysin231), whereas human EpCAM has two (aspartate243/proline244 and proline244/glycine245) [33, 34]. Additionally, the aspartyl protease BACE1 (beta-site amyloid precursor protein-cleaving enzyme 1) cleaves human and murine EpCAM at position tyrosine250/tyrosine251 and tyrosine251/tyrosine252 (β-site), respectively (Fig. 3). BACE1 has an optimal catalytic activity at pH 4 [145] and is therefore active in acidified cytoplasmic vesicles [146]. Under acidic conditions, cleavage of EpCAM is considerably more efficient, and BACE1 overexpression resulted in enhanced release of EpEX [34]. Based on superpositions of cleavage sites on the crystal structure of human EpEX, α- and β-sites are masked within EpEX dimers [3, 33, 147]. Superior cleavage by BACE1 could thus be facilitated owing to the reported decomposition of EpEX dimers to monomers under acidic conditions [3, 147]. However, quantitative contributions of ADAM proteases and BACE1 to the cleavage of EpCAM varied with the cell type [34].
Cleavage of ECAM-CTF is completed by the γ-secretase complex comprising presenilin-2 as catalytic subunit [135] (Fig. 5). Cleavages between residues Val273/Val274, Val274/Val275, and Val275/Val276 in human EpCAM-CTF and between Ala271/Val272 and Val274/Val275 (γ-sites) in murine EpCAM-CTF generate EpCAM-Aβ-like fragments. Cleavages between residues Val284/Val285 and Leu286/Val287 in human EpCAM-CTF and between Val285/Val286, Leu287/Val288, Val288/Iso289, and Ser290/Thr291 (ε-sites) in murine EpCAM-CTF produce EpICD molecules [33, 34]. Initial observation of a preferential proteolysis in malignant versus healthy colon tissue [135] was corroborated by independent findings. Firstly, RIP of EpCAM was not observed in fetal or adult liver cells, nor was it involved in regulating proliferation of these cells [148]. Secondly, EpICD nuclear translocation in various carcinomas correlated with more aggressive phenotypes and poorer outcome [149,150,151]. Lastly, generation of EpICD by γ-secretase is a particularly slow process with a 50% turnover of EpCAM-CTF between 0.75 and 5.5 h [152], as shown for other γ-secretase substrates [153]. Furthermore, EpICD is a highly labile protein that is degraded by the proteasome [34, 152], which might be controlled by two ubiquitylation sites at lysine299 and lysine303 within EpICD [154]. Based on all these findings, we believe RIP of EpCAM is most probably involved in a lengthy signaling process rather than in producing a signaling spike accompanied by comprehensive degradation of EpCAM.
The existence of a membrane version of EpCAM that is lacking the intracellular domain group has been reported [63], which correlated with a more aggressive phenotype of colorectal and pancreatic cancers and with reduced overall survival of the afflicted patients [58, 63]. Alternative EpCAM mRNA splicing was reported; however, none of these differentially spliced mRNAs would encode the truncated version of EpCAM (https://www.ncbi.nlm.nih.gov/ieb/research/acembly/av.cgi?db=human&term=EPCAM&submit=Go). Alternatively, rhomboid proteases and members of the signal peptide peptidase-like proteases (SPPL3) can cleave their substrates directly within the transmembrane domain. Thus, rhomboids could produce an EpCAM variant devoid of EpICD, but these proteases have only been demonstrated to cleave type II membrane proteins, whereas EpCAM is a type I membrane protein. Also, cleavage by SPPL3 and rhomboids is expected to release the substrates’ extracellular domains owing to the reduced hydrophobicity and lack of retention in the plasma membrane. Schnell et al. reported on γ-secretase-independent cleavage of EpCAM-CTF variants by membrane-associated proteases [35], which theoretically could cleave EpCAM without EpEX shedding. They further described an additional EpCAM cleavage at two sites within the cysteine-poor region that can alternatively generate EpICD [35]. Alternatively, the ectodomain of EpCAM may remain membrane-associated through the interaction with a yet unknown membrane component or post-translational modification such as acylation, which have not yet been described.
More recently, cleavage of EpCAM within the extracellular domain by the membrane-tethered serine peptidase matriptase was described [155]. Matriptase was found to catalyze dibasic cleavage of EpCAM between arginines 80 and 81, reducing the interaction of EpCAM with claudin-7 inducing its destabilization. This event has the potential to contribute to the disruption of the epithelial integrity of mouse intestine in CTE [156, 157].
6.2 Signaling by intact EpCAM
Intact EpCAM also signals through associated intracellular proteins. The regulatory p85 subunit of phosphatidylinositol 3-kinase (PI3K) shifts its binding affinity from N-cadherin to EpCAM following overexpression of the latter [45]. The EpCAM/p85 complex displayed kinase activity, suggesting a signaling pathway of EpCAM involving activation of PI3K [45]. More recently, the embryonic Ras GTPase (ERas) was isolated as an interaction partner of EpCAM in murine teratocarcinoma cells [158]. EpCAM and ERas are expressed in pluripotent ESC and in single cells of the epiblast and visceral endoderm of murine embryos and are co-regulated at the early onset of gastrulation [158]. EpCAM/ERas interaction was associated with enhanced activating phosphorylation of AKT at serine473, and cellular knockout of EpCAM resulted in diminished AKT phosphorylation [158]. Furthermore, EpCAM levels regulate the activating phosphorylation of NF-κB subunit Rel A, destabilization of the inhibitor of κB (IκB), and ultimately control interleukin-8 (IL-8) expression [159]. IL-8 in turns was instrumental in the regulation of EpCAM-dependent cell invasion and positively correlated with EpCAM expression in metastatic breast cancer [159].
Thus far, we have a limited understanding of ligands that activate EpCAM signaling. EpEX is the only known extracellular ligand inducing the RIP of EpCAM [135]. Cell-cell contact likewise induced EpCAM RIP [160]. Additional extracellular cues originating from tumor cells and/or cells of the tumor microenvironment remain elusive.
6.3 Spatiotemporal expression of EpCAM in normal tissue and carcinomas
Decades after its discovery on cancer cells, EpCAM was found to be highly expressed on murine and human ESCs [161, 162], and on murine embryonic germ cells [163]. High levels of EpCAM correlate with the pluripotent state of ESCs [137, 161, 162] and with the re-acquisition of pluripotency during reprogramming of somatic cells [138, 139, 164]. In fact, the uphold co-expression of EpCAM with reprogramming factors Nanog and Sox2 is mandatory for somatic cells to progress towards reprogrammed induced pluripotent stem cells (iPSCs) [165].
Single-cell RNA sequencing disclosed that EpCAM is expressed in cells of the inner cell mass (ICM) at gestation day E3.5 of mouse embryogenesis [158]. Epiblast, primitive and visceral endoderm, and earliest cells of the forming primitive streak express EpCAM, although to levels that are reduced compared to ICM cells. With the onset of gastrulation at E6.5, EpCAM expression was strongly reduced or absent in early mesodermal cells [158]. In Xenopus, EpCAM controls cell movements during embryonic development in the three germ layers [166]. Overexpression of EpCAM in a gain-of-function mutation in meso- and ectodermal cells enhanced their invasive potential and thereby induced an intermixing of the cell types based on the repression of the activity of novel protein kinase C variants [166, 167].
At later stages of murine embryogenesis (> E8.5), EpCAM expression was primarily detected in murine endodermal tissue [46, 158]. Spatiotemporal regulation of EpCAM expression was reproduced in murine ESCs after spontaneous differentiation in EBs and confirmed the lack of EpCAM in vimentin-positive mesodermal cells and its retention in Foxa2/Gata4-positive endodermal cells [158]. Balanced EpCAM expression in differentiating ESC appears mandatory as the co-existence of EpCAM-positive endodermal cells and EpCAM-negative mesodermal cells was required for full ESC differentiation [158]. Interference with this controlled expression yielded ESCs with reduced pluripotency and differentiation capacity, and with impaired capability to generate cardiomyocytes [158, 161]. Disturbance of ERas expression hampered spontaneous ESC differentiation in similar fashion [158], suggesting that EpCAM/ERas signaling is required in murine ESC for full pluripotency. The requirement of EpCAM-positive and EpCAM-negative cells for the development of contracting cardiomyocytes confirmed previous reports [168,169,170]. Through transcription factor Gata4, EpCAM-positive visceral and definitive endoderm is formed from pluripotent ESCs [168]. Both endoderm types support the generation of cardiomyocytes from mesodermal cells through the production of cardiac-inducing factors, and themselves differentiate towards liver progenitors [168, 169]. Accordingly, mature hepatocytes lack EpCAM, whereas human hepatic progenitors express EpCAM [171, 172] without activating it through RIP [148]. EpCAM’s role in hepatocyte differentiation was uncovered in zebrafish, where EpCAM is enriched in endodermal cells and counteracts the repression of WNT signaling to induce hepatocyte differentiation. Molecularly, EpCAM blocks Kremen-1 and Dickkopf-2 interactions through sequestration of Kremen-1, preventing Wnt receptor Lrp6 (lipoprotein receptor-related protein 6) withdrawal from the plasma membrane. As a result, Wnt2bb signaling is activated and promotes hepatocyte differentiation from endodermal cells [173].
Hence, spatiotemporal expression and functions of EpCAM during embryogenesis are tightly regulated and required for the proper development of endo- and mesodermal cells in cell-autonomous and non-autonomous ways.
6.4 Regulation of EpCAM in cancer progression: the EMT path and metastasis formation
In line with an absence of EpCAM in mesodermal cells, frequent loss of EpCAM occurs in malignant cells undergoing EMT [174,175,176]. First reports of a transient EpCAM regulation in cancer progression came from xenotransplantation models. Primary tumors and larger metastases (≥ 30 cells) expressed high levels of EpCAM, whereas smaller metastases (< 15 cells) lacked EpCAM [55]. Loss of EpCAM coincided with increased expression of mesenchymal marker vimentin in primary human tumors [72, 174, 176] and in disseminated tumor cells [21, 177, 178]. Because EMT is neither an all-or-nothing process nor does it apply to the totality of malignant cells in a tumor, EMT promotes inter- and intratumor heterogeneity [74, 80, 174, 179, 180], fostering tumor progression, metastasis formation, and therapy resistance within subsets of cells [76, 174, 180, 181]. An involvement of EMT in the metastatic cascade implies the transient and reversible acquisition of migratory and invasive traits by subsets of tumor cells through a partial mesenchymal transition that can be regulated at the epigenetic level [179, 182]. Alternatively, pre-existing subsets of tumor cells in an EMT state are present at earliest stages of tumor formation and represent metastatic progenitors that can co-evolve within primary tumors [183] or at distant sites following early detachment from primary tumors [184]. It must also be noted that the actual contribution of EMT to the metastatic cascade is a matter of strong debate [179] with reports on the lack of requirement for a mesenchymal shift for the generation of distant metastases [185, 186].
Single-cell RNA-seq of oropharyngeal carcinomas uncovered a huge degree of inter- and intratumor heterogeneity at the transcriptome level [187]. A signature of partial EMT associated with metastasis formation and poor prognosis and was inversely correlated with a signature of epithelial differentiation in which EpCAM was a major determinant [187]. Functionally, tumor cells in an EMT state are more refractory to therapy and possess increased migratory and invasive traits, supporting local and distant dissemination [179, 181, 187, 188]. Eventually, metastatic outgrowth requires that disseminated tumor cells re-adopt a proliferative, epithelial phenotype that is associated with the reversion of EMT (i.e., MET). In summary, EMT emerged as a transient state with gradual changes, which strongly contributes to tumor progression and which can be monitored using a panel of dominant markers including EpCAM.
Changes along the EMT path involving loss of EpCAM are likewise observed in CTCs [177, 178] and DTCs [189]. This may have repercussions at two levels: (i) loss of EpCAM in CTCs undergoing EMT will hamper their detection using the EpCAM-based CellSearch enrichment system and (ii) it raises the question as to whether EpCAM-negative CTCs and DTCs have metastatic potential. Clinical studies on CTCs using CellSearch underscored the prognostic value of EpCAM-positive CTCs in various cancers [20, 21, 82, 84,85,86,87,88,89,90]. A study in castration-resistant prostate cancer and MBC patients revealed that the frequency of EpCAM-low CTCs was not correlated with the patients’ overall survival, while of EpCAM-high CTC frequency was associated with poor overall survival [190]. CTCs and DTCs with differing EMT status—as measured by EpCAM expression—were likewise detected in a mouse model of MBC [21]. EpCAM-positive CTCs with an epithelial phenotype and a restricted mesenchymal shift showed the highest metastatic potential and were associated with distant metastases and poorer survival in MBC patients [21]. In contrast, the increase of EMT-type CTCs in MBC patients correlated with disease progression following therapy [178], and mouse-derived mesenchymal-type CTCs were less susceptible to chemotherapeutic drugs in vitro [21]. In conclusion, a variety of EMT types of CTCs and DTCs appear to coexist in individual animals and in patients, which can be classified using EpCAM as a marker. From the most recent reports, it seems that rather epithelial-type CTCs are the source of metastases, whereas more mesenchymal-type CTCs represent treatment-resistant cells.
In addition to being a valuable marker for the EMT status of tumor cells, EpCAM is also functionally involved in the regulation of EMT. A double-negative feedback loop, in which activated extracellular regulated kinase 2 (Erk2) directly and indirectly repressed the transcription of EPCAM through binding to its promoter region and through the induction of EMT transcription factors that repress EPCAM transcription, was reported [30]. EpCAM on the other hand repressed ERK activation and thereby dampened EMT induction [30]. In nasopharyngeal carcinomas, high expression of EpCAM correlated with metastasis formation in vitro and in vivo but had no effect on cell proliferation. Strong expression of EpCAM promoted EMT and a cancer stem cell phenotype in association with increased migration and invasion, via the activation of AKT, mTOR, p70S6K, and 4EBP1 [191]. In colon cancer cell lines, the expression of EpCAM enhanced the transcription of reprogramming factor genes c-Myc, Oct3/4, Sox2, and Nanog, and the EMT regulators Snail and Slug through EpICD signaling [192].
Activation of EpCAM RIP through EGFR signaling was described in endometrial cells, which eventually results in the release of EpICD and the activation of EMT-relevant genes in cooperation with transcription factor LEF-1 [140]. For unknown reasons, the reported cleavage of EpCAM following EGF treatment could not be reproduced in a variety of carcinoma cell lines [143]. However, a functional connection of EpCAM and EGFR emerged very recently. We demonstrated that EGFR has a dual capacity to either induce proliferation or EMT in HNSCC cells, a phenomenon that was dependent upon the strength of activation of the downstream effector kinase Erk1/2 [143]. EpEX was revealed as a novel EGFR ligand in HNSCC [143] and in colon cancer cells [119]. EpEX induces classical EGFR-mediated pathways (i.e., AKT and Erk) but induces Erk1/2 activation to a lesser extent than EGF in HNSCC cell lines, resulting in a mild cell proliferation but no EMT. In contrast, treatment of HNSCC cell lines with EMT-inducing concentrations of EGF and equimolar amounts of EpEX blocked EMT through decreased Erk1/2 activation [143]. Patients suffering from EGFRhigh/EpCAMlow HNSCC were characterized by very poor survival, whereas EGFRlow/EpCAMhigh patients had an excellent clinical outcome [143]. Furthermore, EpEX was shown to activate EpCAM RIP via EGFR signaling, resulting EpICD generation [119]. EpICD was required for β-catenin accumulation in the nucleus and for activation of hypoxia-inducible factor 1 alpha (HIF1α). Accordingly, nuclear localization of EpICD in colon carcinoma patients was associated with metastasis formation and worsened clinical outcome [119]. Interestingly, anti-EpCAM monoclonal EpAb2-6 inhibited nuclear translocation of EpICD and induced apoptosis. Thus, EpAb2-6 might represent a novel and promising treatment to reduce metastasis formation in patients at risk [119].
Lastly, EpEX binding to EGFR promoted the multipotency of mesenchymal stem cells through enhancement of pluripotency factors. Mechanistically, EpEX induced an EGFR-dependent STAT3 activation and the blockade of Let7 microRNA through upregulation of LIN28 [193]. As a result, EpEX induces proliferation of bone marrow-derived mesenchymal stem cells. Hence, EpCAM regulates the fate of various stem cells through multiple mechanisms including membrane-associated signaling and as a ligand of EGFR. Furthermore, EpCAM is regulated during EMT and is itself a regulator of this trans-differentiation program in carcinoma and stem cells. Several modes of action have been reported that involve RIP products EpEX and EpICD, and full-length EpCAM. Interestingly, EMT-promoting and EMT-repressing functions of EpCAM have been described, a controversy that deserves further investigation.
7 Perspective
In the future, we expect further insight in the role of EpCAM in the regulation of cell fate in health and disease, which would eventually revive its usage as therapeutic target. The discovery of RIP of EpCAM and the generation of the signaling-active fragments EpEX and EpICD paved the way for a novel class of EpCAM inhibitors that target signaling in cancer and the metastatic cascade. Antagonizing antibodies such as EpAb2-6 and small molecule inhibitors that compete with EpCAM RIP or with EpICD functions could develop into promising candidate drugs for the treatment of EpCAM-positive carcinomas and the formation of lethal metastases.
EpCAM will retain a central role as of anchor molecule in the enrichment of CTCs that harbor metastatic potential in advanced cancer patients. Here, EpCAM has dual potential as a quantifier of systemic tumor cells in the frame of liquid biopsies and as a potential target for adjuvant therapy of residual tumor cells with specific biologicals.
Clinical studies on the predictive potential of EpCAM for carcinoma entities associated with a high degree of treatment resistance are required for the use of EpCAM as biomarker in clinical decision-making. For example, prospective studies on the expression of EGFR and EpCAM might shed light on the power of EpCAM expression to predict treatment response in carcinoma entities that implement a therapy with the anti-EGFR monoclonal antibody cetuximab or small molecule inhibitors of EGFR.
In the future, the role of EpCAM in pluripotent stem cells might gain momentum. Especially, the implication of EpCAM and EpICD in the generation of iPS is of relevance. Additionally, the use of EpEX in combination with the reprogramming factors Klf4 or Oct3/4 was instrumental in the generation of iPS and might therefore experience (pre-)clinical application.
Lastly, it can be anticipated that basic research on the expression dynamics and the molecular functions of EpCAM in cancer and healthy cells will further support the abovementioned clinical applications of this highly versatile molecule.
8 Conclusion
Over the past four decades, EpCAM has evolved from a humoral antigen expressed on the majority of carcinoma cells to a complex signaling molecule involved in central aspects of cell fate such as proliferation, pluripotency, differentiation, and organ integrity. Signaling by intact EpCAM and the proteolytic fragments EpEX and EpICD as well as signaling-independent functions of EpCAM serve these various purposes and represent novel handles to tackle metastatic malignancies. Furthermore, EpCAM remains an attractive target for antibody-based cancer therapies and as a biomarker for patient stratification. Importantly, EpCAM is the central target molecule for the enrichment and characterization of systemic tumor cells with prognostic and metastatic potential. Eventually, EpCAM became a multifaceted protein with a long-standing history in molecular oncology and in stem cell biology.
Data availability
Not applicable.
Abbreviations
- AKT:
-
serin/threonine kinase (protein kinase B; PKB)
- 4EBP1:
-
eukaryotic translation initiation 4E-binding protein 1
- c-Myc:
-
cellular Myc
- CTC:
-
circulating tumor cell
- CTE:
-
congenital tufting enteropathy
- DTC:
-
disseminated tumor cell
- EGF:
-
epidermal growth factor
- EGFR:
-
epidermal growth factor receptor
- EMT:
-
epithelial-to-mesenchymal transition
- EpCAM:
-
epithelial cell adhesion molecule
- EpEX:
-
EpCAM extracellular domain
- EpICD:
-
EpCAM intracellular domain
- Erk:
-
extracellular regulated kinase
- ESC:
-
embryonic stem cells
- FHL2:
-
four-and-a-half LIM domain 2
- GTPase:
-
guanine triphosphatase
- HNSCC:
-
head and neck squamous cell carcinoma
- ICM:
-
inner cell mass
- iPS:
-
induced pluripotent stem cells
- Klf4:
-
Krüppel-like factor 4
- LEF-1:
-
lymphoid enhancer factor 1
- Let7:
-
lethal 7
- LIN28:
-
abnormal cell lineage 28
- mAb:
-
monoclonal antibody
- MBC:
-
metastatic breast cancer
- mTOR:
-
mammalian target of rapamycin
- Oct3/4:
-
octamer-binding factor 3/4
- PI3K:
-
phosphatidylinositol 3-kinase
- p70S6K:
-
p70 S6-kinase
- RIP:
-
regulated intramembrane proteolysis
- STAT3:
-
signal transducer and activator of transcription 3
- Sox2:
-
SRY (sex-determining region Y)-box 2
References
Herlyn, M., Steplewski, Z., Herlyn, D., & Koprowski, H. (1979). Colorectal carcinoma-specific antigen: detection by means of monoclonal antibodies. Proceedings of the National Academy of Sciences of the United States of America, 76(3), 1438–1442.
Strnad, J., Hamilton, A. E., Beavers, L. S., Gamboa, G. C., Apelgren, L. D., Taber, L. D., et al. (1989). Molecular cloning and characterization of a human adenocarcinoma/epithelial cell surface antigen complementary DNA. Cancer Research, 49(2), 314–317.
Pavsic, M., Guncar, G., Djinovic-Carugo, K., & Lenarcic, B. (2014). Crystal structure and its bearing towards an understanding of key biological functions of EpCAM. Nature Communications, 5, 4764. https://doi.org/10.1038/ncomms5764.
Litvinov, S. V., Bakker, H. A., Gourevitch, M. M., Velders, M. P., & Warnaar, S. O. (1994). Evidence for a role of the epithelial glycoprotein 40 (Ep-CAM) in epithelial cell-cell adhesion. Cell Adhesion and Communication, 2(5), 417–428.
Litvinov, S. V., Balzar, M., Winter, M. J., Bakker, H. A., Briaire-de Bruijn, I. H., Prins, F., et al. (1997). Epithelial cell adhesion molecule (Ep-CAM) modulates cell-cell interactions mediated by classic cadherins. The Journal of Cell Biology, 139(5), 1337–1348.
Schon, M. P., Schon, M., Klein, C. E., Blume, U., Bisson, S., & Orfanos, C. E. (1994). Carcinoma-associated 38-kD membrane glycoprotein MH 99/KS 1/4 is related to proliferation and age of transformed epithelial cell lines. The Journal of Investigative Dermatology, 102(6), 987–991.
Litvinov, S. V., van Driel, W., van Rhijn, C. M., Bakker, H. A., van Krieken, H., Fleuren, G. J., et al. (1996). Expression of Ep-CAM in cervical squamous epithelia correlates with an increased proliferation and the disappearance of markers for terminal differentiation. The American Journal of Pathology, 148(3), 865–875.
Osta, W. A., Chen, Y., Mikhitarian, K., Mitas, M., Salem, M., Hannun, Y. A., et al. (2004). EpCAM is overexpressed in breast cancer and is a potential target for breast cancer gene therapy. Cancer Research, 64(16), 5818–5824.
Munz, M., Kieu, C., Mack, B., Schmitt, B., Zeidler, R., & Gires, O. (2004). The carcinoma-associated antigen EpCAM upregulates c-myc and induces cell proliferation. Oncogene, 23(34), 5748–5758.
Munz, M., Baeuerle, P. A., & Gires, O. (2009). The emerging role of EpCAM in cancer and stem cell signaling. Cancer Research, 69(14), 5627–5629. https://doi.org/10.1158/0008-5472.CAN-09-0654.
Went, P. T., Lugli, A., Meier, S., Bundi, M., Mirlacher, M., Sauter, G., et al. (2004). Frequent EpCam protein expression in human carcinomas. Human Pathology, 35(1), 122–128.
Went, P., Vasei, M., Bubendorf, L., Terracciano, L., Tornillo, L., Riede, U., et al. (2006). Frequent high-level expression of the immunotherapeutic target Ep-CAM in colon, stomach, prostate and lung cancers. British Journal of Cancer, 94(1), 128–135.
Spizzo, G., Fong, D., Wurm, M., Ensinger, C., Obrist, P., Hofer, C., et al. (2011). EpCAM expression in primary tumour tissues and metastases: an immunohistochemical analysis. Journal of Clinical Pathology, 64(5), 415–420. https://doi.org/10.1136/jcp.2011.090274.
van der Fels, C. A. M., Rosati, S., & de Jong, I. J. (2017). EpCAM expression in lymph node metastases of urothelial cell carcinoma of the bladder: a pilot study. International Journal of Molecular Sciences, 18(8). https://doi.org/10.3390/ijms18081802.
Keller, L., Werner, S., & Pantel, K. (2019). Biology and clinical relevance of EpCAM. Cell Stress, 3(6), 165–180. https://doi.org/10.15698/cst2019.06.188.
White, C. A., Weaver, R. L., & Grillo-Lopez, A. J. (2001). Antibody-targeted immunotherapy for treatment of malignancy. Annual Review of Medicine, 52, 125–145. https://doi.org/10.1146/annurev.med.52.1.125.
Pantel, K., Brakenhoff, R. H., & Brandt, B. (2008). Detection, clinical relevance and specific biological properties of disseminating tumour cells. Nature Reviews. Cancer, 8(5), 329–340.
Cristofanilli, M., Budd, G. T., Ellis, M. J., Stopeck, A., Matera, J., Miller, M. C., et al. (2004). Circulating tumor cells, disease progression, and survival in metastatic breast cancer. [clinical trial multicenter study]. The New England Journal of Medicine, 351(8), 781–791. https://doi.org/10.1056/NEJMoa040766.
Coumans, F. A., Siesling, S., & Terstappen, L. W. (2013). Detection of cancer before distant metastasis. BMC Cancer, 13(1), 283. https://doi.org/10.1186/1471-2407-13-283.
Baccelli, I., Schneeweiss, A., Riethdorf, S., Stenzinger, A., Schillert, A., Vogel, V., et al. (2013). Identification of a population of blood circulating tumor cells from breast cancer patients that initiates metastasis in a xenograft assay. [Research Support, Non-U.S. Gov't]. Nature Biotechnology, 31(6), 539–544. https://doi.org/10.1038/nbt.2576.
Liu, X., Li, J., Cadilha, B. L., Markota, A., Voigt, C., Huang, Z., et al. (2019). Epithelial-type systemic breast carcinoma cells with a restricted mesenchymal transition are a major source of metastasis. Science Advances, 5(6), eaav4275. https://doi.org/10.1126/sciadv.aav4275.
Sivagnanam, M., Mueller, J. L., Lee, H., Chen, Z., Nelson, S. F., Turner, D., et al. (2008). Identification of EpCAM as the gene for congenital tufting enteropathy. Gastroenterology.
Kozan, P. A., McGeough, M. D., Pena, C. A., Mueller, J. L., Barrett, K. E., Marchelletta, R. R., et al. (2015). Mutation of EpCAM leads to intestinal barrier and ion transport dysfunction. Journal of Molecular Medicine (Berlin, Germany), 93(5), 535–545. https://doi.org/10.1007/s00109-014-1239-x.
Mueller, J. L., McGeough, M. D., Pena, C. A., & Sivagnanam, M. (2014). Functional consequences of EpCam mutation in mice and men. American Journal of Physiology. Gastrointestinal and Liver Physiology, 306(4), G278–G288. https://doi.org/10.1152/ajpgi.00286.2013.
Kastrinos, F., & Stoffel, E. M. (2014). History, genetics, and strategies for cancer prevention in Lynch syndrome. Clinical Gastroenterology and Hepatology, 12(5), 715–727. https://doi.org/10.1016/j.cgh.2013.06.031.
Lynch, H. T., Lynch, J. F., Snyder, C. L., & Riegert-Johnson, D. (2011). EPCAM deletions, Lynch syndrome, and cancer risk. The Lancet Oncology, 12(1), 5–6. https://doi.org/10.1016/S1470-2045(10)70291-6.
Linnenbach, A. J., Seng, B. A., Wu, S., Robbins, S., Scollon, M., Pyrc, J. J., et al. (1993). Retroposition in a family of carcinoma-associated antigen genes. Molecular and Cellular Biology, 13(3), 1507–1515.
McLaughlin, P. M., Harmsen, M. C., Dokter, W. H., Kroesen, B. J., van der Molen, H., Brinker, M. G., et al. (2001). The epithelial glycoprotein 2 (EGP-2) promoter-driven epithelial-specific expression of EGP-2 in transgenic mice: a new model to study carcinoma-directed immunotherapy. Cancer Research, 61(10), 4105–4111.
Gires, O., Kieu, C., Fix, P., Schmitt, B., Munz, M., Wollenberg, B., et al. (2001). Tumor necrosis factor alpha negatively regulates the expression of the carcinoma-associated antigen epithelial cell adhesion molecule. Cancer, 92(3), 620–628.
Sankpal, N. V., Fleming, T. P., Sharma, P. K., Wiedner, H. J., & Gillanders, W. E. (2017). A double-negative feedback loop between EpCAM and ERK contributes to the regulation of epithelial-mesenchymal transition in cancer. Oncogene. https://doi.org/10.1038/onc.2016.504.
Yamashita, T., Budhu, A., Forgues, M., & Wang, X. W. (2007). Activation of hepatic stem cell marker EpCAM by Wnt-beta-catenin signaling in hepatocellular carcinoma. Cancer Research, 67(22), 10831–10839.
Vannier, C., Mock, K., Brabletz, T., & Driever, W. (2013). Zeb1 regulates E-cadherin and Epcam expression to control cell behavior in early zebrafish development. The Journal of Biological Chemistry. https://doi.org/10.1074/jbc.M113.467787.
Tsaktanis, T., Kremling, H., Pavsic, M., von Stackelberg, R., Mack, B., Fukumori, A., et al. (2015). Cleavage and cell adhesion properties of human epithelial cell adhesion molecule (HEPCAM). The Journal of Biological Chemistry, 290(40), 24574–24591. https://doi.org/10.1074/jbc.M115.662700.
Hachmeister, M., Bobowski, K. D., Hogl, S., Dislich, B., Fukumori, A., Eggert, C., et al. (2013). Regulated intramembrane proteolysis and degradation of murine epithelial cell adhesion molecule mEpCAM. [Research Support, Non-U.S. Gov't]. PLoS One, 8(8), e71836. https://doi.org/10.1371/journal.pone.0071836.
Schnell, U., Kuipers, J., & Giepmans, B. N. (2013). EpCAM proteolysis: new fragments with distinct functions? Bioscience Reports, 33(2), e00030. https://doi.org/10.1042/BSR20120128.
Baeuerle, P. A., & Gires, O. (2007). EpCAM (CD326) finding its role in cancer. British Journal of Cancer, 96(3), 417–423.
Mohtar, M. A., Syafruddin, S. E., Nasir, S. N., & Yew, L. T. (2020). Revisiting the roles of pro-metastatic EpCAM in cancer. Biomolecules, 10(2). https://doi.org/10.3390/biom10020255.
Chong, J. M., & Speicher, D. W. (2001). Determination of disulfide bond assignments and N-glycosylation sites of the human gastrointestinal carcinoma antigen GA733-2 (CO17-1A, EGP, KS1-4, KSA, and Ep-CAM). The Journal of Biological Chemistry, 276(8), 5804–5813.
Munz, M., Fellinger, K., Hofmann, T., Schmitt, B., & Gires, O. (2008). Glycosylation is crucial for stability of tumour and cancer stem cell antigen EpCAM. Frontiers in Bioscience, 13, 5195–5201.
Pauli, C., Munz, M., Kieu, C., Mack, B., Breinl, P., Wollenberg, B., et al. (2003). Tumor-specific glycosylation of the carcinoma-associated epithelial cell adhesion molecule EpCAM in head and neck carcinomas. Cancer Letters, 193(1), 25–32.
Litvinov, S. V., Velders, M. P., Bakker, H. A., Fleuren, G. J., & Warnaar, S. O. (1994). Ep-CAM: a human epithelial antigen is a homophilic cell-cell adhesion molecule. The Journal of Cell Biology, 125(2), 437–446.
Balzar, M., Briaire-de Bruijn, I. H., Rees-Bakker, H. A., Prins, F. A., Helfrich, W., de Leij, L., et al. (2001). Epidermal growth factor-like repeats mediate lateral and reciprocal interactions of Ep-CAM molecules in homophilic adhesions. Molecular and Cellular Biology, 21(7), 2570–2580.
Balzar, M., Bakker, H. A., Briaire-de-Bruijn, I. H., Fleuren, G. J., Warnaar, S. O., & Litvinov, S. V. (1998). Cytoplasmic tail regulates the intercellular adhesion function of the epithelial cell adhesion molecule. Molecular and Cellular Biology, 18(8), 4833–4843.
Winter, M. J., Nagelkerken, B., Mertens, A. E., Rees-Bakker, H. A., Briaire-de Bruijn, I. H., & Litvinov, S. V. (2003). Expression of Ep-CAM shifts the state of cadherin-mediated adhesions from strong to weak. Experimental Cell Research, 285(1), 50–58.
Winter, M. J., Cirulli, V., Briaire-de Bruijn, I. H., & Litvinov, S. V. (2007). Cadherins are regulated by Ep-CAM via phosphaditylinositol-3 kinase. Molecular and Cellular Biochemistry, 302(1-2), 19–26.
Nagao, K., Zhu, J., Heneghan, M. B., Hanson, J. C., Morasso, M. I., Tessarollo, L., et al. (2009). Abnormal placental development and early embryonic lethality in EpCAM-null mice. PLoS One, 4(12), e8543. https://doi.org/10.1371/journal.pone.0008543.
Guerra, E., Lattanzio, R., La Sorda, R., Dini, F., Tiboni, G. M., Piantelli, M., et al. (2012). mTrop1/Epcam knockout mice develop congenital tufting enteropathy through dysregulation of intestinal E-cadherin/beta-catenin. PLoS One, 7(11), e49302. https://doi.org/10.1371/journal.pone.0049302.
Lei, Z., Maeda, T., Tamura, A., Nakamura, T., Yamazaki, Y., Shiratori, H., et al. (2012). EpCAM contributes to formation of functional tight junction in the intestinal epithelium by recruiting claudin proteins. Developmental Biology, 371(2), 136–145. https://doi.org/10.1016/j.ydbio.2012.07.005.
Sivagnanam, M., Schaible, T., Szigeti, R., Byrd, R. H., Finegold, M. J., Ranganathan, S., et al. (2010). Further evidence for EpCAM as the gene for congenital tufting enteropathy. American Journal of Medical Genetics. Part A, 152A(1), 222–224. https://doi.org/10.1002/ajmg.a.33186.
Ladwein, M., Pape, U. F., Schmidt, D. S., Schnolzer, M., Fiedler, S., Langbein, L., et al. (2005). The cell-cell adhesion molecule EpCAM interacts directly with the tight junction protein claudin-7. Experimental Cell Research, 309(2), 345–357.
Kuhn, S., Koch, M., Nubel, T., Ladwein, M., Antolovic, D., Klingbeil, P., et al. (2007). A complex of EpCAM, claudin-7, CD44 variant isoforms, and tetraspanins promotes colorectal cancer progression. Molecular Cancer Research, 5(6), 553–567.
Nubel, T., Preobraschenski, J., Tuncay, H., Weiss, T., Kuhn, S., Ladwein, M., et al. (2009). Claudin-7 regulates EpCAM-mediated functions in tumor progression. Molecular Cancer Research, 7(3), 285–299. https://doi.org/10.1158/1541-7786.MCR-08-0200.
Slanchev, K., Carney, T. J., Stemmler, M. P., Koschorz, B., Amsterdam, A., Schwarz, H., et al. (2009). The epithelial cell adhesion molecule EpCAM is required for epithelial morphogenesis and integrity during zebrafish epiboly and skin development. PLoS Genetics, 5(7), e1000563. https://doi.org/10.1371/journal.pgen.1000563.
Gaber, A., Kim, S. J., Kaake, R. M., Bencina, M., Krogan, N., Sali, A., et al. (2018). EpCAM homo-oligomerization is not the basis for its role in cell-cell adhesion. Scientific Reports, 8(1), 13269. https://doi.org/10.1038/s41598-018-31482-7.
Jojovic, M., Adam, E., Zangemeister-Wittke, U., & Schumacher, U. H. (1998). Epithelial glycoprotein-2 expression is subject to regulatory processes in epithelial-mesenchymal transitions during metastases: an investigation of human cancers transplanted into severe combined immunodeficient mice. The Histochemical Journal, 30(10), 723–729.
Gastl, G., Spizzo, G., Obrist, P., Dunser, M., & Mikuz, G. (2000). Ep-CAM overexpression in breast cancer as a predictor of survival. Lancet, 356(9246), 1981–1982.
Spizzo, G., Went, P., Dirnhofer, S., Obrist, P., Simon, R., Spichtin, H., et al. (2004). High Ep-CAM expression is associated with poor prognosis in node-positive breast cancer. Breast Cancer Research and Treatment, 86(3), 207–213.
Seeber, A., Untergasser, G., Spizzo, G., Terracciano, L., Lugli, A., Kasal, A., et al. (2016). Predominant expression of truncated EpCAM is associated with a more aggressive phenotype and predicts poor overall survival in colorectal cancer. International Journal of Cancer, 139(3), 657–663. https://doi.org/10.1002/ijc.30099.
Massoner, P., Thomm, T., Mack, B., Untergasser, G., Martowicz, A., Bobowski, K., et al. (2014). EpCAM is overexpressed in local and metastatic prostate cancer, suppressed by chemotherapy and modulated by MET-associated miRNA-200c/205. British Journal of Cancer, 111(5), 955–964. https://doi.org/10.1038/bjc.2014.366.
Varga, M., Obrist, P., Schneeberger, S., Muhlmann, G., Felgel-Farnholz, C., Fong, D., et al. (2004). Overexpression of epithelial cell adhesion molecule antigen in gallbladder carcinoma is an independent marker for poor survival. Clinical Cancer Research, 10(9), 3131–3136.
Spizzo, G., Went, P., Dirnhofer, S., Obrist, P., Moch, H., Baeuerle, P. A., et al. (2006). Overexpression of epithelial cell adhesion molecule (Ep-CAM) is an independent prognostic marker for reduced survival of patients with epithelial ovarian cancer. Gynecologic Oncology.
Brunner, A., Prelog, M., Verdorfer, I., Tzankov, A., Mikuz, G., & Ensinger, C. (2008). EpCAM is predominantly expressed in high grade and advanced stage urothelial carcinoma of the bladder. Journal of Clinical Pathology, 61(3), 307–310. https://doi.org/10.1136/jcp.2007.049460.
Fong, D., Moser, P., Kasal, A., Seeber, A., Gastl, G., Martowicz, A., et al. (2014). Loss of membranous expression of the intracellular domain of EpCAM is a frequent event and predicts poor survival in patients with pancreatic cancer. Histopathology, 64(5), 683–692. https://doi.org/10.1111/his.12307.
Fong, D., Steurer, M., Obrist, P., Barbieri, V., Margreiter, R., Amberger, A., et al. (2006). Ep-CAM expression in pancreatic and ampullary carcinomas: frequency and prognostic relevance. Journal of Clinical Pathology.
Lee, S. J., Chung, K. Y., Kwon, J. E., Yoon, S. O., & Kim, S. K. (2018). Expression of EpCAM in adenoid cystic carcinoma. Pathology, 50(7), 737–741. https://doi.org/10.1016/j.pathol.2018.08.013.
Kimura, H., Kato, H., Faried, A., Sohda, M., Nakajima, M., Fukai, Y., et al. (2007). Prognostic significance of EpCAM expression in human esophageal cancer. International Journal of Oncology, 30(1), 171–179.
Went, P., Dirnhofer, S., Salvisberg, T., Amin, M. B., Lim, S. D., Diener, P. A., et al. (2005). Expression of epithelial cell adhesion molecule (EpCam) in renal epithelial tumors. The American Journal of Surgical Pathology, 29(1), 83–88.
Seligson, D. B., Pantuck, A. J., Liu, X., Huang, Y., Horvath, S., Bui, M. H., et al. (2004). Epithelial cell adhesion molecule (KSA) expression: pathobiology and its role as an independent predictor of survival in renal cell carcinoma. Clinical Cancer Research, 10(8), 2659–2669. https://doi.org/10.1158/1078-0432.ccr-1132-03.
Songun, I., Litvinov, S. V., van de Velde, C. J., Pals, S. T., Hermans, J., & van Krieken, J. H. (2005). Loss of Ep-CAM (CO17-1A) expression predicts survival in patients with gastric cancer. British Journal of Cancer, 92(9), 1767–1772.
Wen, K. C., Sung, P. L., Chou, Y. T., Pan, C. M., Wang, P. H., Lee, O. K., et al. (2018). The role of EpCAM in tumor progression and the clinical prognosis of endometrial carcinoma. Gynecologic Oncology, 148(2), 383–392. https://doi.org/10.1016/j.ygyno.2017.11.033.
Ensinger, C., Kremser, R., Prommegger, R., Spizzo, G., & Schmid, K. W. (2006). EpCAM overexpression in thyroid carcinomas: a histopathological study of 121 cases. Journal of Immunotherapy, 29(5), 569–573. https://doi.org/10.1097/01.cji.0000211303.52503.da.
Baumeister, P., Hollmann, A., Kitz, J., Afthonidou, A., Simon, F., Shakhtour, J., et al. (2018). High expression of EpCAM and Sox2 is a positive prognosticator of clinical outcome for head and neck carcinoma. Scientific Reports, 8(1), 14582. https://doi.org/10.1038/s41598-018-32178-8.
Spizzo, G., Gastl, G., Wolf, D., Gunsilius, E., Steurer, M., Fong, D., et al. (2003). Correlation of COX-2 and Ep-CAM overexpression in human invasive breast cancer and its impact on survival. British Journal of Cancer, 88(4), 574–578.
Hinohara, K., & Polyak, K. (2019). Intratumoral heterogeneity: more than just mutations. Trends in Cell Biology, 29(7), 569–579. https://doi.org/10.1016/j.tcb.2019.03.003.
Iacobuzio-Donahue, C. A., Litchfield, K., & Swanton, C. (2020). Intratumor heterogeneity reflects clinical disease course. Nature Cancer, 1(1), 3–6. https://doi.org/10.1038/s43018-019-0002-1.
Pribluda, A., de la Cruz, C. C., & Jackson, E. L. (2015). Intratumoral heterogeneity: from diversity comes resistance. Clinical Cancer Research, 21(13), 2916–2923. https://doi.org/10.1158/1078-0432.CCR-14-1213.
Saunders, N. A., Simpson, F., Thompson, E. W., Hill, M. M., Endo-Munoz, L., Leggatt, G., et al. (2012). Role of intratumoural heterogeneity in cancer drug resistance: molecular and clinical perspectives. EMBO Molecular Medicine, 4(8), 675–684. https://doi.org/10.1002/emmm.201101131.
Shackleton, M., Quintana, E., Fearon, E. R., & Morrison, S. J. (2009). Heterogeneity in cancer: cancer stem cells versus clonal evolution. Cell, 138(5), 822–829. https://doi.org/10.1016/j.cell.2009.08.017.
Shipitsin, M., Campbell, L. L., Argani, P., Weremowicz, S., Bloushtain-Qimron, N., Yao, J., et al. (2007). Molecular definition of breast tumor heterogeneity. Cancer Cell, 11(3), 259–273.
Wahl, G. M., & Spike, B. T. (2017). Cell state plasticity, stem cells, EMT, and the generation of intra-tumoral heterogeneity. NPJ Breast Cancer, 3, 14. https://doi.org/10.1038/s41523-017-0012-z.
Dasgupta, A., Lim, A. R., & Ghajar, C. M. (2017). Circulating and disseminated tumor cells: harbingers or initiators of metastasis? Molecular Oncology, 11(1), 40–61. https://doi.org/10.1002/1878-0261.12022.
Joosse, S. A., Gorges, T. M., & Pantel, K. (2015). Biology, detection, and clinical implications of circulating tumor cells. EMBO Molecular Medicine, 7(1), 1–11. https://doi.org/10.15252/emmm.201303698.
Kang, Y., & Pantel, K. (2013). Tumor cell dissemination: emerging biological insights from animal models and cancer patients. Cancer Cell, 23(5), 573–581. https://doi.org/10.1016/j.ccr.2013.04.017.
Alix-Panabieres, C., & Pantel, K. (2013). Circulating tumor cells: liquid biopsy of cancer. Clinical Chemistry, 59(1), 110–118. https://doi.org/10.1373/clinchem.2012.194258.
Janni, W., Rack, B., Terstappen, L. W., Pierga, J. Y., Taran, F. A., Fehm, T., et al. (2016). Pooled analysis of the prognostic relevance of circulating tumor cells in primary breast cancer. Clinical Cancer Research. https://doi.org/10.1158/1078-0432.CCR-15-1603.
Lindsay, C. R., Blackhall, F. H., Carmel, A., Fernandez-Gutierrez, F., Gazzaniga, P., Groen, H. J. M., et al. (2019). EPAC-lung: pooled analysis of circulating tumour cells in advanced non-small cell lung cancer. European Journal of Cancer, 117, 60–68. https://doi.org/10.1016/j.ejca.2019.04.019.
Poveda, A., Kaye, S. B., McCormack, R., Wang, S., Parekh, T., Ricci, D., et al. (2011). Circulating tumor cells predict progression free survival and overall survival in patients with relapsed/recurrent advanced ovarian cancer. Gynecologic Oncology, 122(3), 567–572. https://doi.org/10.1016/j.ygyno.2011.05.028.
Yang, C., Zou, K., Yuan, Z., Guo, T., & Xiong, B. (2018). Prognostic value of circulating tumor cells detected with the CellSearch System in patients with gastric cancer: evidence from a meta-analysis. Onco Targets Ther, 11, 1013-1023, doi:https://doi.org/10.2147/OTT.S154114.
Gorges, T. M., Stein, A., Quidde, J., Hauch, S., Rock, K., Riethdorf, S., et al. (2016). Improved detection of circulating tumor cells in metastatic colorectal cancer by the combination of the CellSearch(R) System and the AdnaTest(R). PLoS One, 11(5), e0155126. https://doi.org/10.1371/journal.pone.0155126.
Garrel, R., Mazel, M., Perriard, F., Vinches, M., Cayrefourcq, L., Guigay, J., et al. (2019). Circulating tumor cells as a prognostic factor in recurrent or metastatic head and neck squamous cell carcinoma: the CIRCUTEC prospective study. Clinical Chemistry, 65(10), 1267–1275. https://doi.org/10.1373/clinchem.2019.305904.
Wang, H., Stoecklein, N. H., Lin, P. P., & Gires, O. (2017). Circulating and disseminated tumor cells: diagnostic tools and therapeutic targets in motion. Oncotarget, 8(1), 1884–1912. https://doi.org/10.18632/oncotarget.12242.
Gires, O., Klein, C. A., & Baeuerle, P. A. (2009). On the abundance of EpCAM on cancer stem cells. Nature Reviews. Cancer, 9(2), 143; author reply 143. https://doi.org/10.1038/nrc2499-c1.
Gottlinger, H. G., Funke, I., Johnson, J. P., Gokel, J. M., & Riethmuller, G. (1986). The epithelial cell surface antigen 17-1A, a target for antibody-mediated tumor therapy: its biochemical nature, tissue distribution and recognition by different monoclonal antibodies. International Journal of Cancer, 38(1), 47–53.
Fogler, W. E., Klinger, M. R., Abraham, K. G., Gottlinger, H. G., Riethmuller, G., & Daddona, P. E. (1988). Enhanced cytotoxicity against colon carcinoma by combinations of noncompeting monoclonal antibodies to the 17-1A antigen. Cancer Research, 48(22), 6303–6308.
Pantel, K., Schlimok, G., Braun, S., Kutter, D., Lindemann, F., Schaller, G., et al. (1993). Differential expression of proliferation-associated molecules in individual micrometastatic carcinoma cells. Journal of the National Cancer Institute, 85(17), 1419–1424.
Riethmüller, G., Schneider Gadicke, E., Schlimok, G., Schmiegel, W., Raab, R., Hoffken, K., et al. (1994). Randomised trial of monoclonal antibody for adjuvant therapy of resected Dukes’ C colorectal carcinoma. Lancet, 343(8907), 1177–1183.
Kufer, P., Mack, M., Gruber, R., Lutterbuse, R., Zettl, F., & Riethmuller, G. (1997). Construction and biological activity of a recombinant bispecific single-chain antibody designed for therapy of minimal residual colorectal cancer. Cancer Immunology, Immunotherapy, 45(3-4), 193–197.
Mack, M., Gruber, R., Schmidt, S., Riethmuller, G., & Kufer, P. (1997). Biologic properties of a bispecific single-chain antibody directed against 17-1A (EpCAM) and CD3: tumor cell-dependent T cell stimulation and cytotoxic activity. Journal of Immunology, 158(8), 3965–3970.
Riethmuller, G., Holz, E., Schlimok, G., Schmiegel, W., Raab, R., Hoffken, K., et al. (1998). Monoclonal antibody therapy for resected Dukes’ C colorectal cancer: seven-year outcome of a multicenter randomized trial. Journal of Clinical Oncology, 16(5), 1788–1794.
Braun, S., Hepp, F., Kentenich, C. R., Janni, W., Pantel, K., Riethmuller, G., et al. (1999). Monoclonal antibody therapy with edrecolomab in breast cancer patients: monitoring of elimination of disseminated cytokeratin-positive tumor cells in bone marrow. Clinical Cancer Research, 5(12), 3999–4004.
Hempel, P., Muller, P., Oruzio, D., Behr, W., Brockmeyer, C., Wochner, M., et al. (2000). Combination of high-dose chemotherapy and monoclonal antibody in breast-cancer patients: a pilot trial to monitor treatment effects on disseminated tumor cells. Cytotherapy, 2(4), 287–295.
Steplewski, Z., Lubeck, M. D., & Koprowski, H. (1983). Human macrophages armed with murine immunoglobulin G2a antibodies to tumors destroy human cancer cells. Science, 221(4613), 865–867. https://doi.org/10.1126/science.6879183.
Schlimok, G., Gottlinger, H., Funke, I., Swierkot, S., Hauser, H., & Riethmuller, G. (1986). In vivo and in vitro labelling of epithelial tumor cells with anti 17-1A monoclonal antibodies in bone marrow of cancer patients. Hybridoma, 5(Suppl 1), S163–S170.
Pantel, K., Izbicki, J. R., Angstwurm, M., Braun, S., Passlick, B., Karg, O., et al. (1993). Immunocytological detection of bone marrow micrometastasis in operable non-small cell lung cancer. Cancer Research, 53(5), 1027–1031.
Weiner, L. M., Steplewski, Z., Koprowski, H., Sears, H. F., Litwin, S., & Comis, R. L. (1986). Biologic effects of gamma interferon pre-treatment followed by monoclonal antibody 17-1A administration in patients with gastrointestinal carcinoma. Hybridoma, 5(Suppl 1), S65–S77.
Verrill, H., Goldberg, M., Rosenbaum, R., Abbott, R., Simunovic, L., Steplewski, Z., et al. (1986). Clinical trial of Wistar Institute 17-1A monoclonal antibody in patients with advanced gastrointestinal adenocarcinoma: a preliminary report. Hybridoma, 5(Suppl 1), S175–S183.
Ragnhammar, P., Fagerberg, J., Frodin, J. E., Hjelm, A. L., Lindemalm, C., Magnusson, I., et al. (1993). Effect of monoclonal antibody 17-1A and GM-CSF in patients with advanced colorectal carcinoma—long-lasting, complete remissions can be induced. International Journal of Cancer, 53(5), 751–758.
Ragnhammar, P., Magnusson, I., Masucci, G., & Mellstedt, H. (1993). The therapeutic use of the unconjugated monoclonal antibodies (MAb) 17-1A in combination with GM-CSF in the treatment of colorectal carcinoma (CRC). Medical Oncology and Tumor Pharmacotherapy, 10(1-2), 61–70. https://doi.org/10.1007/bf02987770.
Punt, C. J., Nagy, A., Douillard, J. Y., Figer, A., Skovsgaard, T., Monson, J., et al. (2002). Edrecolomab alone or in combination with fluorouracil and folinic acid in the adjuvant treatment of stage III colon cancer: a randomised study. Lancet, 360(9334), 671–677.
de Bono, J. S., Tolcher, A. W., Forero, A., Vanhove, G. F., Takimoto, C., Bauer, R. J., et al. (2004). ING-1, a monoclonal antibody targeting Ep-CAM in patients with advanced adenocarcinomas. Clinical Cancer Research, 10(22), 7555–7565. https://doi.org/10.1158/1078-0432.CCR-04-0729.
Goel, S., Bauer, R. J., Desai, K., Bulgaru, A., Iqbal, T., Strachan, B. K., et al. (2007). Pharmacokinetic and safety study of subcutaneously administered weekly ING-1, a human engineere monoclonal antibody targeting human EpCAM, in patients with advanced solid tumors. Annals of Oncology, 18(10), 1704–1707.
Munz, M., Murr, A., Kvesic, M., Rau, D., Mangold, S., Pflanz, S., et al. (2010). Side-by-side analysis of five clinically tested anti-EpCAM monoclonal antibodies. Cancer Cell International, 10, 44. https://doi.org/10.1186/1475-2867-10-44.
Schmidt, M., Scheulen, M. E., Dittrich, C., Obrist, P., Marschner, N., Dirix, L., et al. (2009). An open-label, randomized phase II study of adecatumumab, a fully human anti-EpCAM antibody, as monotherapy in patients with metastatic breast cancer. Annals of Oncology. https://doi.org/10.1093/annonc/mdp314.
Marschner, N., Ruttinger, D., Zugmaier, G., Nemere, G., Lehmann, J., Obrist, P., et al. (2010). Phase II study of the human anti-epithelial cell adhesion molecule antibody adecatumumab in prostate cancer patients with increasing serum levels of prostate-specific antigen after radical prostatectomy. Urologia Internationalis, 85(4), 386–395. https://doi.org/10.1159/000318055.
Zeidler, R., Reisbach, G., Wollenberg, B., Lang, S., Chaubal, S., Schmitt, B., et al. (1999). Simultaneous activation of T cells and accessory cells by a new class of intact bispecific antibody results in efficient tumor cell killing. Journal of Immunology, 163(3), 1246–1252.
Heiss, M. M., Murawa, P., Koralewski, P., Kutarska, E., Kolesnik, O. O., Ivanchenko, V. V., et al. (2010). The trifunctional antibody catumaxomab for the treatment of malignant ascites due to epithelial cancer: results of a prospective randomized phase II/III trial. International Journal of Cancer. https://doi.org/10.1002/ijc.25423.
Cioffi, M., Dorado, J., Baeuerle, P. A., & Heeschen, C. (2012). EpCAM/CD3-bispecific T-cell engaging antibody MT110 eliminates primary human pancreatic cancer stem cells. Clinical Cancer Research, 18(2), 465–474. https://doi.org/10.1158/1078-0432.CCR-11-1270.
Liao, M. Y., Lai, J. K., Kuo, M. Y., Lu, R. M., Lin, C. W., Cheng, P. C., et al. (2015). An anti-EpCAM antibody EpAb2-6 for the treatment of colon cancer. Oncotarget, 6(28), 24947–24968. https://doi.org/10.18632/oncotarget.4453.
Liang, K. H., Tso, H. C., Hung, S. H., Kuan, I. I., Lai, J. K., Ke, F. Y., et al. (2018). Extracellular domain of EpCAM enhances tumor progression through EGFR signaling in colon cancer cells. Cancer Letters, 433, 165–175. https://doi.org/10.1016/j.canlet.2018.06.040.
Cizeau, J., Grenkow, D. M., Brown, J. G., Entwistle, J., & MacDonald, G. C. (2009). Engineering and biological characterization of VB6-845, an anti-EpCAM immunotoxin containing a T-cell epitope-depleted variant of the plant toxin bouganin. Journal of Immunotherapy, 32(6), 574–584. https://doi.org/10.1097/CJI.0b013e3181a6981c.
Brown, J., Rasamoelisolo, M., Spearman, M., Bosc, D., Cizeau, J., Entwistle, J., et al. (2009). Preclinical assessment of an anti-EpCAM immunotoxin: locoregional delivery provides a safer alternative to systemic administration. Cancer Biotherapy & Radiopharmaceuticals, 24(4), 477–487. https://doi.org/10.1089/cbr.2008.0579.
Moldenhauer, G., Salnikov, A. V., Luttgau, S., Herr, I., Anderl, J., & Faulstich, H. (2012). Therapeutic potential of amanitin-conjugated anti-epithelial cell adhesion molecule monoclonal antibody against pancreatic carcinoma. Journal of the National Cancer Institute, 104(8), 622–634. https://doi.org/10.1093/jnci/djs140.
Ko, Y. J., Bubley, G. J., Weber, R., Redfern, C., Gold, D. P., Finke, L., et al. (2004). Safety, pharmacokinetics, and biological pharmacodynamics of the immunocytokine EMD 273066 (huKS-IL2): results of a phase I trial in patients with prostate cancer. Journal of Immunotherapy, 27(3), 232–239. https://doi.org/10.1097/00002371-200405000-00008.
Hussain, S., Pluckthun, A., Allen, T. M., & Zangemeister-Wittke, U. (2006). Chemosensitization of carcinoma cells using epithelial cell adhesion molecule-targeted liposomal antisense against bcl-2/bcl-xL. Molecular Cancer Therapeutics, 5(12), 3170–3180.
MacDonald, G. C., Rasamoelisolo, M., Entwistle, J., Cuthbert, W., Kowalski, M., Spearman, M. A., et al. (2009). A phase I clinical study of intratumorally administered VB4-845, an anti-epithelial cell adhesion molecule recombinant fusion protein, in patients with squamous cell carcinoma of the head and neck. Medical Oncology, 26(3), 257–264. https://doi.org/10.1007/s12032-008-9111-x.
Kowalski, M., Entwistle, J., Cizeau, J., Niforos, D., Loewen, S., Chapman, W., et al. (2010). A phase I study of an intravesically administered immunotoxin targeting EpCAM for the treatment of nonmuscle-invasive bladder cancer in BCGrefractory and BCG-intolerant patients. Drug Design, Development and Therapy, 4, 313–320. https://doi.org/10.2147/DDDT.S14071.
Andersson, Y., Engebraaten, O., Juell, S., Aamdal, S., Brunsvig, P., Fodstad, O., et al. (2015). Phase I trial of EpCAM-targeting immunotoxin MOC31PE, alone and in combination with cyclosporin. British Journal of Cancer, 113(11), 1548–1555. https://doi.org/10.1038/bjc.2015.380.
Andersson, Y., Haavardtun, S. I., Davidson, B., Dorum, A., Fleten, K. G., Fodstad, O., et al. (2017). MOC31PE immunotoxin—targeting peritoneal metastasis from epithelial ovarian cancer. Oncotarget, 8(37), 61800–61809. https://doi.org/10.18632/oncotarget.18694.
Froysnes, I. S., Andersson, Y., Larsen, S. G., Davidson, B., Oien, J. T., Olsen, K. H., et al. (2017). Novel treatment with intraperitoneal MOC31PE immunotoxin in colorectal peritoneal metastasis: results from the ImmunoPeCa phase 1 trial. Annals of Surgical Oncology, 24(7), 1916–1922. https://doi.org/10.1245/s10434-017-5814-6.
Macdonald, J., Henri, J., Roy, K., Hays, E., Bauer, M., Veedu, R. N., et al. (2018). EpCAM immunotherapy versus specific targeted delivery of drugs. Cancers (Basel), 10(1). https://doi.org/10.3390/cancers10010019.
Baumeister, P., Baumuller, K., Harreus, U., Reiter, M., & Welz, C. (2018). Evaluation of margins in head and neck squamous cell carcinoma from the surgeon’s perspective. Head & Neck. https://doi.org/10.1002/hed.25061.
Englhard, A. S., Palaras, A., Volgger, V., Stepp, H., Mack, B., Libl, D., et al. (2017). Confocal laser endomicroscopy in head and neck malignancies using FITC-labelled EpCAM- and EGF-R-antibodies in cell lines and tumor biopsies. Journal of Biophotonics. https://doi.org/10.1002/jbio.201600238.
van Driel, P. B., Boonstra, M. C., Prevoo, H. A., van de Giessen, M., Snoeks, T. J., Tummers, Q. R., et al. (2016). EpCAM as multi-tumour target for near-infrared fluorescence guided surgery. BMC Cancer, 16(1), 884. https://doi.org/10.1186/s12885-016-2932-7.
Hoogstins, C. E., Weixler, B., Boogerd, L. S., Hoppener, D. J., Prevoo, H. A., Sier, C. F., et al. (2017). In search for optimal targets for intraoperative fluorescence imaging of peritoneal metastasis from colorectal cancer. Biomark Cancer, 9, 1179299X17728254. https://doi.org/10.1177/1179299X17728254.
Maetzel, D., Denzel, S., Mack, B., Canis, M., Went, P., Benk, M., et al. (2009). Nuclear signalling by tumour-associated antigen EpCAM. Nature Cell Biology, 11(2), 162–171.
Chaves-Perez, A., Mack, B., Maetzel, D., Kremling, H., Eggert, C., Harreus, U., et al. (2013). EpCAM regulates cell cycle progression via control of cyclin D1 expression. Oncogene, 32(5), 641–650. https://doi.org/10.1038/onc.2012.75.
Lu, T. Y., Lu, R. M., Liao, M. Y., Yu, J., Chung, C. H., Kao, C. F., et al. (2010). Epithelial cell adhesion molecule regulation is associated with the maintenance of the undifferentiated phenotype of human embryonic stem cells. The Journal of Biological Chemistry, 285(12), 8719–8732. https://doi.org/10.1074/jbc.M109.077081.
Huang, H. P., Chen, P. H., Yu, C. Y., Chuang, C. Y., Stone, L., Hsiao, W. C., et al. (2011). Epithelial cell adhesion molecule (EpCAM) complex proteins promote transcription factor-mediated pluripotency reprogramming. The Journal of Biological Chemistry, 286(38), 33520–33532. https://doi.org/10.1074/jbc.M111.256164.
Yu, T., Ma, Y., & Wang, H. (2017). EpCAM intracellular domain promotes porcine cell reprogramming by upregulation of pluripotent gene expression via beta-catenin signaling. Scientific Reports, 7, 46315. https://doi.org/10.1038/srep46315.
Hsu, Y. T., Osmulski, P., Wang, Y., Huang, Y. W., Liu, L., Ruan, J., et al. (2016). EpCAM-regulated transcription exerts influences on nanomechanical properties of endometrial cancer cells that promote epithelial-to-mesenchymal transition. Cancer Research, 76(21), 6171–6182. https://doi.org/10.1158/0008-5472.CAN-16-0752.
Hsu, Y. T., Gu, F., Huang, Y. W., Liu, J., Ruan, J., Huang, R. L., et al. (2013). Promoter hypomethylation of EpCAM-regulated bone morphogenetic protein gene family in recurrent endometrial cancer. [Research Support, N.I.H., Extramural Research Support, Non-U.S. Gov't]. Clinical Cancer Research, 19(22), 6272–6285. https://doi.org/10.1158/1078-0432.CCR-13-1734.
Gires, O. (2017). EGFR-dependent regulated intramembrane proteolysis of EpCAM—letter. Cancer Research, 77(7), 1775–1776. https://doi.org/10.1158/0008-5472.CAN-16-2456.
Pan, M., Schinke, H., Luxenburger, E., Kranz, G., Shakhtour, J., Libl, D., et al. (2018). EpCAM ectodomain EpEX is a ligand of EGFR that counteracts EGF-mediated epithelial-mesenchymal transition through modulation of phospho-ERK1/2 in head and neck cancers. PLoS Biology, 16(9), e2006624. https://doi.org/10.1371/journal.pbio.2006624.
Le Naour, F., Andre, M., Greco, C., Billard, M., Sordat, B., Emile, J. F., et al. (2006). Profiling of the tetraspanin web of human colon cancer cells. Molecular & Cellular Proteomics, 5(5), 845–857.
Shimizu, H., Tosaki, A., Kaneko, K., Hisano, T., Sakurai, T., & Nukina, N. (2008). Crystal structure of an active form of BACE1, an enzyme responsible for amyloid beta protein production. Molecular and Cellular Biology, 28(11), 3663–3671. https://doi.org/10.1128/MCB.02185-07.
Grbovic, O. M., Mathews, P. M., Jiang, Y., Schmidt, S. D., Dinakar, R., Summers-Terio, N. B., et al. (2003). Rab5-stimulated up-regulation of the endocytic pathway increases intracellular beta-cleaved amyloid precursor protein carboxyl-terminal fragment levels and Abeta production. The Journal of Biological Chemistry, 278(33), 31261–31268. https://doi.org/10.1074/jbc.M304122200.
Pavsic, M., & Lenarcic, B. (2011). Expression, crystallization and preliminary X-ray characterization of the human epithelial cell-adhesion molecule ectodomain. Acta Crystallographica. Section F, Structural Biology and Crystallization Communications, 67(Pt 11), 1363–1366. https://doi.org/10.1107/S1744309111031897.
Gerlach, J. C., Foka, H. G., Thompson, R. L., Gridelli, B., & Schmelzer, E. (2018). Epithelial cell adhesion molecule fragments and signaling in primary human liver cells. Journal of Cellular Physiology, 233(6), 4841–4851. https://doi.org/10.1002/jcp.26286.
Kunavisarut, T., Kak, I., Macmillan, C., Ralhan, R., & Walfish, P. G. (2012). Immunohistochemical analysis based Ep-ICD subcellular localization index (ESLI) is a novel marker for metastatic papillary thyroid microcarcinoma. BMC Cancer, 12(1), 523. https://doi.org/10.1186/1471-2407-12-523.
Ralhan, R., Cao, J., Lim, T., Macmillan, C., Freeman, J. L., & Walfish, P. G. (2010). EpCAM nuclear localization identifies aggressive thyroid cancer and is a marker for poor prognosis. BMC Cancer, 10(1), 331. https://doi.org/10.1186/1471-2407-10-331.
Ralhan, R., He, H. C., So, A. K., Tripathi, S. C., Kumar, M., Hasan, M. R., et al. (2010). Nuclear and cytoplasmic accumulation of Ep-ICD is frequently detected in human epithelial cancers. PLoS One, 5(11), e14130. https://doi.org/10.1371/journal.pone.0014130.
Huang, Y., Chanou, A., Kranz, G., Pan, M., Kohlbauer, V., Ettinger, A., et al. (2019). Membrane-associated epithelial cell adhesion molecule is slowly cleaved by gamma-secretase prior to efficient proteasomal degradation of its intracellular domain. The Journal of Biological Chemistry, 294(9), 3051–3064. https://doi.org/10.1074/jbc.RA118.005874.
Kamp, F., Winkler, E., Trambauer, J., Ebke, A., Fluhrer, R., & Steiner, H. (2015). Intramembrane proteolysis of beta-amyloid precursor protein by gamma-secretase is an unusually slow process. Biophysical Journal, 108(5), 1229–1237. https://doi.org/10.1016/j.bpj.2014.12.045.
Kim, W., Bennett, E. J., Huttlin, E. L., Guo, A., Li, J., Possemato, A., et al. (2011). Systematic and quantitative assessment of the ubiquitin-modified proteome. Molecular Cell, 44(2), 325–340. https://doi.org/10.1016/j.molcel.2011.08.025.
Wu, C. J., Feng, X., Lu, M., Morimura, S., & Udey, M. C. (2017). Matriptase-mediated cleavage of EpCAM destabilizes claudins and dysregulates intestinal epithelial homeostasis. The Journal of Clinical Investigation, 127(2), 623–634. https://doi.org/10.1172/JCI88428.
Kawaguchi, M., Yamamoto, K., Takeda, N., Fukushima, T., Yamashita, F., Sato, K., et al. (2019). Hepatocyte growth factor activator inhibitor-2 stabilizes Epcam and maintains epithelial organization in the mouse intestine. Commun Biol, 2, 11. https://doi.org/10.1038/s42003-018-0255-8.
Szabo, R., Callies, L. K., & Bugge, T. H. (2019). Matriptase drives early-onset intestinal failure in a mouse model of congenital tufting enteropathy. Development, 146(22). https://doi.org/10.1242/dev.183392.
Sarrach, S., Huang, Y., Niedermeyer, S., Hachmeister, M., Fischer, L., Gille, S., et al. (2018). Spatiotemporal patterning of EpCAM is important for murine embryonic endo- and mesodermal differentiation. Scientific Reports, 8(1), 1801. https://doi.org/10.1038/s41598-018-20131-8.
Sankpal, N. V., Fleming, T. P., & Gillanders, W. E. (2013). EpCAM modulates NF-kappaB signaling and interleukin-8 expression in breast cancer. Molecular Cancer Research, 11(4), 418–426. https://doi.org/10.1158/1541-7786.MCR-12-0518.
Denzel, S., Maetzel, D., Mack, B., Eggert, C., Barr, G., & Gires, O. (2009). Initial activation of EpCAM cleavage via cell-to-cell contact. BMC Cancer, 9, 402. https://doi.org/10.1186/1471-2407-9-402.
Gonzalez, B., Denzel, S., Mack, B., Conrad, M., & Gires, O. (2009). EpCAM is involved in maintenance of the murine embryonic stem cell phenotype. Stem Cells, 27(8), 1782–1791. https://doi.org/10.1002/stem.97.
Ng, V. Y., Ang, S. N., Chan, J. X., & Choo, A. B. (2009). Characterization of epithelial cell adhesion molecule as a surface marker on undifferentiated human embryonic stem cells. Stem Cells. https://doi.org/10.1002/stem.221.
Anderson, R., Schaible, K., Heasman, J., & Wylie, C. (1999). Expression of the homophilic adhesion molecule, Ep-CAM, in the mammalian germ line. Journal of Reproduction and Fertility, 116(2), 379–384.
Chen, H. F., Chuang, C. Y., Lee, W. C., Huang, H. P., Wu, H. C., Ho, H. N., et al. (2011). Surface marker epithelial cell adhesion molecule and E-cadherin facilitate the identification and selection of induced pluripotent stem cells. Stem Cell Reviews. https://doi.org/10.1007/s12015-011-9233-y.
Tran, K. A., Pietrzak, S. J., Zaidan, N. Z., Siahpirani, A. F., McCalla, S. G., Zhou, A. S., et al. (2019). Defining reprogramming checkpoints from single-cell analyses of induced pluripotency. Cell Reports, 27(6), 1726–1741 e1725. https://doi.org/10.1016/j.celrep.2019.04.056.
Maghzal, N., Vogt, E., Reintsch, W., Fraser, J. S., & Fagotto, F. (2010). The tumor-associated EpCAM regulates morphogenetic movements through intracellular signaling. The Journal of Cell Biology, 191(3), 645–659. https://doi.org/10.1083/jcb.201004074.
Maghzal, N., Kayali, H. A., Rohani, N., Kajava, A. V., & Fagotto, F. (2013). EpCAM controls actomyosin contractility and cell adhesion by direct inhibition of PKC. Developmental Cell, 27(3), 263–277. https://doi.org/10.1016/j.devcel.2013.10.003.
Holtzinger, A., Rosenfeld, G. E., & Evans, T. (2010). Gata4 directs development of cardiac-inducing endoderm from ES cells. Developmental Biology, 337(1), 63–73. https://doi.org/10.1016/j.ydbio.2009.10.003.
Pal, R., & Khanna, A. (2005). Role of hepatocyte-like cells in the differentiation of cardiomyocytes from mouse embryonic stem cells. Stem Cells and Development, 14(2), 153–161. https://doi.org/10.1089/scd.2005.14.153.
Foley, A. C., Gupta, R. W., Guzzo, R. M., Korol, O., & Mercola, M. (2006). Embryonic heart induction. Annals of the New York Academy of Sciences, 1080, 85–96. https://doi.org/10.1196/annals.1380.008.
Schmelzer, E., Zhang, L., Bruce, A., Wauthier, E., Ludlow, J., Yao, H. L., et al. (2007). Human hepatic stem cells from fetal and postnatal donors. The Journal of Experimental Medicine, 204(8), 1973–1987.
Schmelzer, E., Wauthier, E., & Reid, L. M. (2006). The phenotypes of pluripotent human hepatic progenitors. Stem Cells.
Lu, H., Ma, J., Yang, Y., Shi, W., & Luo, L. (2013). EpCAM is an endoderm-specific Wnt derepressor that licenses hepatic development. Developmental Cell, 24(5), 543–553. https://doi.org/10.1016/j.devcel.2013.01.021.
Dongre, A., & Weinberg, R. A. (2019). New insights into the mechanisms of epithelial-mesenchymal transition and implications for cancer. Nature Reviews. Molecular Cell Biology, 20(2), 69–84. https://doi.org/10.1038/s41580-018-0080-4.
Gires, O., & Stoecklein, N. H. (2014). Dynamic EpCAM expression on circulating and disseminating tumor cells: causes and consequences. Cellular and Molecular Life Sciences, 71(22), 4393–4402. https://doi.org/10.1007/s00018-014-1693-1.
Pastushenko, I., & Blanpain, C. (2019). EMT transition states during tumor progression and metastasis. Trends in Cell Biology, 29(3), 212–226. https://doi.org/10.1016/j.tcb.2018.12.001.
Gorges, T. M., Tinhofer, I., Drosch, M., Rose, L., Zollner, T. M., Krahn, T., et al. (2012). Circulating tumour cells escape from EpCAM-based detection due to epithelial-to-mesenchymal transition. BMC Cancer, 12, 178. https://doi.org/10.1186/1471-2407-12-178.
Yu, M., Bardia, A., Wittner, B. S., Stott, S. L., Smas, M. E., Ting, D. T., et al. (2013). Circulating breast tumor cells exhibit dynamic changes in epithelial and mesenchymal composition. [Research Support, N.I.H., Extramural Research Support, Non-U.S. Gov't]. Science, 339(6119), 580–584. https://doi.org/10.1126/science.1228522.
Brabletz, T., Kalluri, R., Nieto, M. A., & Weinberg, R. A. (2018). EMT in cancer. Nature Reviews. Cancer. https://doi.org/10.1038/nrc.2017.118.
Lambert, A. W., Pattabiraman, D. R., & Weinberg, R. A. (2017). Emerging biological principles of metastasis. Cell, 168(4), 670–691. https://doi.org/10.1016/j.cell.2016.11.037.
Ye, X., & Weinberg, R. A. (2015). Epithelial-mesenchymal plasticity: a central regulator of cancer progression. Trends in Cell Biology, 25(11), 675–686. https://doi.org/10.1016/j.tcb.2015.07.012.
Tam, W. L., & Weinberg, R. A. (2013). The epigenetics of epithelial-mesenchymal plasticity in cancer. Nature Medicine, 19(11), 1438–1449. https://doi.org/10.1038/nm.3336.
Harper, K. L., Sosa, M. S., Entenberg, D., Hosseini, H., Cheung, J. F., Nobre, R., et al. (2016). Mechanism of early dissemination and metastasis in Her2(+) mammary cancer. Nature, 540(7634), 588–592. https://doi.org/10.1038/nature20609.
Werner-Klein, M., Scheitler, S., Hoffmann, M., Hodak, I., Dietz, K., Lehnert, P., et al. (2018). Genetic alterations driving metastatic colony formation are acquired outside of the primary tumour in melanoma. Nature Communications, 9(1), 595. https://doi.org/10.1038/s41467-017-02674-y.
Fischer, K. R., Durrans, A., Lee, S., Sheng, J., Li, F., Wong, S. T., et al. (2015). Epithelial-to-mesenchymal transition is not required for lung metastasis but contributes to chemoresistance. Nature, 527(7579), 472–476. https://doi.org/10.1038/nature15748.
Zheng, X., Carstens, J. L., Kim, J., Scheible, M., Kaye, J., Sugimoto, H., et al. (2015). Epithelial-to-mesenchymal transition is dispensable for metastasis but induces chemoresistance in pancreatic cancer. Nature, 527(7579), 525–530. https://doi.org/10.1038/nature16064.
Puram, S. V., Tirosh, I., Parikh, A. S., Patel, A. P., Yizhak, K., Gillespie, S., et al. (2017). Single-cell transcriptomic analysis of primary and metastatic tumor ecosystems in head and neck cancer. Cell, 171(7), 1611–1624 e1624. https://doi.org/10.1016/j.cell.2017.10.044.
Yang, J., & Weinberg, R. A. (2008). Epithelial-mesenchymal transition: at the crossroads of development and tumor metastasis. Developmental Cell, 14(6), 818–829. https://doi.org/10.1016/j.devcel.2008.05.009.
Driemel, C., Kremling, H., Schumacher, S., Will, D., Wolters, J., Lindenlauf, N., et al. (2014). Context-dependent adaption of EpCAM expression in early systemic esophageal cancer. Oncogene, 33(41), 4904–4915. https://doi.org/10.1038/onc.2013.441.
de Wit, S., Manicone, M., Rossi, E., Lampignano, R., Yang, L., Zill, B., et al. (2018). EpCAM(high) and EpCAM(low) circulating tumor cells in metastatic prostate and breast cancer patients. Oncotarget, 9(86), 35705–35716. https://doi.org/10.18632/oncotarget.26298.
Wang, M. H., Sun, R., Zhou, X. M., Zhang, M. Y., Lu, J. B., Yang, Y., et al. (2018). Epithelial cell adhesion molecule overexpression regulates epithelial-mesenchymal transition, stemness and metastasis of nasopharyngeal carcinoma cells via the PTEN/AKT/mTOR pathway. Cell Death & Disease, 9(1), 2. https://doi.org/10.1038/s41419-017-0013-8.
Lin, C. W., Liao, M. Y., Lin, W. W., Wang, Y. P., Lu, T. Y., & Wu, H. C. (2012). Epithelial cell adhesion molecule regulates tumor initiation and tumorigenesis via activating reprogramming factors and epithelial-mesenchymal transition gene expression in colon cancer. The Journal of Biological Chemistry, 287(47), 39449–39459. https://doi.org/10.1074/jbc.M112.386235.
Kuan, II, Lee, C. C., Chen, C. H., Lu, J., Kuo, Y. S., & Wu, H. C. (2019). The extracellular domain of epithelial cell adhesion molecule (EpCAM) enhances multipotency of mesenchymal stem cells through EGFR-LIN28-LET7 signaling. The Journal of Biological Chemistry, 294(19), 7769-7786, doi:https://doi.org/10.1074/jbc.RA119.007386.
Code availability
Not applicable.
Funding
Open Access funding provided by Projekt DEAL. The work has been supported in parts by funding by the Deutsche Forschungsgemeinschaft (Gi540/3-2) and the Bayerisches Staatsministerium für Wirtschaft, Energie und Technologie BayBIO (BIO1803-0003) to OG.
Author information
Authors and Affiliations
Contributions
OG wrote the initial manuscript draft and generated figures. MP, HS, MC, and PAB contributed topics and helped writing the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
PAB is a consultant for MPM Capital LLC, Oncology Impact Management, Harpoon Therapeutics Inc., TCR2 Therapeutics Inc., Werewolf Therapeutics Inc., iOmx Therapeutics AG, and Cullinan Oncology LLC. The other authors declare that they have no competing interests.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Gires, O., Pan, M., Schinke, H. et al. Expression and function of epithelial cell adhesion molecule EpCAM: where are we after 40 years?. Cancer Metastasis Rev 39, 969–987 (2020). https://doi.org/10.1007/s10555-020-09898-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10555-020-09898-3