Abstract
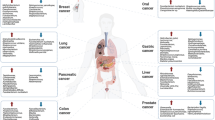
A dynamic mucosal layer shields the epithelial cells lining the body cavities and is made up of high molecular weight, heavily glycosylated, multidomain proteins called mucins. Mucins, broadly grouped into transmembrane and secreted mucins, are the first responders to any mechanical or chemical insult to the epithelia and help maintain tissue homeostasis. However, their intrinsic properties to protect and repair the epithelia are exploited during oncogenic processes, where mucins are metamorphosed to aid the tumor cells in their malignant journey. Diverse domains, like the variable number tandem repeats (VNTR), sea urchin sperm protein enterokinase and agrin (SEA), adhesion-associated domain (AMOP), nidogen-like domain (NIDO), epidermal growth factor-like domain (EGF), and von Willebrand factor type D domain (vWD) on mucins, including MUC1, MUC4, MUC5AC, MUC5B, and MUC16, have been shown to facilitate cell-to-cell and cell-to-matrix interactions, and cell-autonomous signaling to promote tumorigenesis and distant dissemination of tumor cells. Several obstacles have limited the study of mucins, including technical difficulties in working with these huge glycoproteins, the dearth of scientific tools, and lack of animal models; thus, the tissue-dependent and domain-specific roles of mucins during mucosal protection, chronic inflammation, tumorigenesis, and hematological dissemination of malignant cells are still unclear. Future studies should try to integrate information on the rheological, molecular, and biological characteristics of mucins to comprehensively delineate their pathophysiological role and evaluate their suitability as targets in future diagnostic and therapeutic strategies.



Similar content being viewed by others
References
Peterson, L. W., & Artis, D. (2014). Intestinal epithelial cells: regulators of barrier function and immune homeostasis. Nature Reviews Immunology, 14(3), 141–153.
Linden, S., Sutton, P., Karlsson, N., Korolik, V., & McGuckin, M. (2008). Mucins in the mucosal barrier to infection. Mucosal Immunology, 1(3), 183–197.
Johansson, M. E., Sjövall, H., & Hansson, G. C. (2013). The gastrointestinal mucus system in health and disease. Nature Reviews Gastroenterology & Hepatology, 10(6), 352–361.
Lillehoj, E. P., Kato, K., Lu, W., & Kim, K. C. (2013). Cellular and molecular biology of airway mucins. In International review of cell and molecular biology (Vol. 303, pp. 139–202). Elsevier.
Kufe, D. W. (2009). Mucins in cancer: function, prognosis and therapy. Nature Reviews Cancer, 9(12), 874–885.
Desseyn, J.-L., Buisine, M.-P., Porchet, N., Aubert, J.-P., Degand, P., & Laine, A. (1998). Evolutionary history of the 11p15 human mucin gene family. Journal of Molecular Evolution, 46(1), 102–106.
Duraisamy, S., Ramasamy, S., Kharbanda, S., & Kufe, D. (2006). Distinct evolution of the human carcinoma-associated transmembrane mucins, MUC1, MUC4 AND MUC16. Gene, 373, 28–34.
van Putten, J. P., & Strijbis, K. (2017). Transmembrane mucins: signaling receptors at the intersection of inflammation and cancer. Journal of Innate Immunity, 9(3), 281–299.
Lakshmanan, I., Ponnusamy, M. P., Macha, M. A., Haridas, D., Majhi, P. D., Kaur, S., Jain, M., Batra, S. K., & Ganti, A. K. (2015). Mucins in lung cancer: diagnostic, prognostic, and therapeutic implications. Journal of Thoracic Oncology, 10(1), 19–27.
Hollingsworth, M. A., & Swanson, B. J. (2004). Mucins in cancer: protection and control of the cell surface. Nature Reviews Cancer, 4(1), 45–60.
Kaur, S., Kumar, S., Momi, N., Sasson, A. R., & Batra, S. K. (2013). Mucins in pancreatic cancer and its microenvironment. Nature Reviews Gastroenterology & Hepatology, 10(10), 607–620.
Pothuraju, R., Krishn, S. R., Gautam, S. K., Pai, P., Ganguly, K., Chaudhary, S., Rachagani, S., Kaur, S., & Batra, S. K. (2020). Mechanistic and functional shades of mucins and associated glycans in colon cancer. Cancers, 12(3), 649.
Mukhopadhyay, P., Chakraborty, S., Ponnusamy, M. P., Lakshmanan, I., Jain, M., & Batra, S. K. (2011). Mucins in the pathogenesis of breast cancer: implications in diagnosis, prognosis and therapy. Biochimica et Biophysica Acta (BBA)-Reviews on Cancer, 1815(2), 224–240.
Singh, A. P., Senapati, S., Ponnusamy, M. P., Jain, M., Lele, S. M., Davis, J. S., Remmenga, S., & Batra, S. K. (2008). Clinical potential of mucins in diagnosis, prognosis, and therapy of ovarian cancer. The Lancet Oncology, 9(11), 1076–1085.
Bafna, S., Kaur, S., & Batra, S. K. (2010). Membrane-bound mucins: the mechanistic basis for alterations in the growth and survival of cancer cells. Oncogene, 29(20), 2893–2904.
Krishn, S. R., Ganguly, K., Kaur, S., & Batra, S. K. (2018). Ramifications of secreted mucin MUC5AC in malignant journey: a holistic view. Carcinogenesis, 39(5), 633–651.
Bhatia, R., Gautam, S. K., Cannon, A., Thompson, C., Hall, B. R., Aithal, A., Banerjee, K., Jain, M., Solheim, J. C., Kumar, S., & Batra, S. K. (2019). Cancer-associated mucins: role in immune modulation and metastasis. Cancer and Metastasis Reviews, 38(1–2), 223–236.
Cavey, M., & Lecuit, T. (2009). Molecular bases of cell–cell junctions stability and dynamics. Cold Spring Harbor Perspectives in Biology, 1(5), a002998.
Tepass, U., Tanentzapf, G., Ward, R., & Fehon, R. (2001). Epithelial cell polarity and cell junctions in Drosophila. Annual Review of Genetics, 35(1), 747–784.
Wagner, C., Wheeler, K., & Ribbeck, K. (2018). Mucins and their role in shaping the functions of mucus barriers. Annual Review of Cell and Developmental Biology, 34, 189–215.
Silverman, H. S., Parry, S., Sutton-Smith, M., Burdick, M. D., McDermott, K., Reid, C. J., Batra, S. K., Morris, H. R., Hollingsworth, M. A., Dell, A., & Harris, A. (2001). In vivo glycosylation of mucin tandem repeats. Glycobiology, 11(6), 459–471.
Dhanisha, S. S., Guruvayoorappan, C., Drishya, S., & Abeesh, P. (2018). Mucins: structural diversity, biosynthesis, its role in pathogenesis and as possible therapeutic targets. Critical Reviews in Oncology/Hematology, 122, 98–122.
Hayashi, T., Takahashi, T., Motoya, S., Ishida, T., Itoh, F., Adachi, M., Hinoda, Y., & Imai, K. (2001). MUC1 mucin core protein binds to the domain 1 of ICAM-1. Digestion, 63(Suppl 1), 87–92. https://doi.org/10.1159/000051917.
Rajabi, H., Hata, T., Li, W., Long, M. D., Hu, Q., Liu, S., Raina, D., Kui, L., Yasumizu, Y., Hong, D., Samur, M., & Kufe, D. (2019). MUC1-C represses the RASSF1A tumor suppressor in human carcinoma cells. Oncogene, 38(47), 7266–7277. https://doi.org/10.1038/s41388-019-0940-1.
Kinlough, C. L., Poland, P. A., Bruns, J. B., Harkleroad, K. L., & Hughey, R. P. (2004). MUC1 membrane trafficking is modulated by multiple interactions. Journal of Biological Chemistry, 279(51), 53071–53077.
Kinlough, C. L., McMahan, R. J., Poland, P. A., Bruns, J. B., Harkleroad, K. L., Stremple, R. J., Kashlan, O. B., Weixel, K. M., Weisz, O. A., & Hughey, R. P. (2006). Recycling of MUC1 is dependent on its palmitoylation. Journal of Biological Chemistry, 281(17), 12112–12122.
Singh, P. K., & Hollingsworth, M. A. (2006). Cell surface-associated mucins in signal transduction. Trends in Cell Biology, 16(9), 467–476.
Schroeder, J. A., Thompson, M. C., Gardner, M. M., & Gendler, S. J. (2001). Transgenic MUC1 interacts with epidermal growth factor receptor and correlates with mitogen-activated protein kinase activation in the mouse mammary gland. Journal of Biological Chemistry, 276(16), 13057–13064.
Hattrup, C. L., & Gendler, S. J. (2006). MUC1 alters oncogenic events and transcription in human breast cancer cells. Breast Cancer Research, 8(4), R37.
Schroeder, J. A., Adriance, M. C., Thompson, M. C., Camenisch, T. D., & Gendler, S. J. (2003). MUC1 alters β-catenin-dependent tumor formation and promotes cellular invasion. Oncogene, 22(9), 1324–1332.
Bitler, B. G., Menzl, I., Huerta, C. L., Sands, B., Knowlton, W., Chang, A., & Schroeder, J. A. (2009). Intracellular MUC1 peptides inhibit cancer progression. Clinical Cancer Research, 15(1), 100–109.
Li, Y., Kuwahara, H., Ren, J., Wen, G., & Kufe, D. (2001). The c-Src tyrosine kinase regulates signaling of the human DF3/MUC1 carcinoma-associated antigen with GSK3β and β-catenin. Journal of Biological Chemistry, 276(9), 6061–6064.
Roy, L. D., Sahraei, M., Subramani, D. B., Besmer, D., Nath, S., Tinder, T. L., Bajaj, E., Shanmugam, K., Lee, Y. Y., Hwang, S. I. L., Gendler, S. J., & Mukherjee, P. (2011). MUC1 enhances invasiveness of pancreatic cancer cells by inducing epithelial to mesenchymal transition. Oncogene, 30(12), 1449–1459.
Ho, S. B., Dvorak, L. A., Moor, R. E., Jacobson, A. C., Frey, M. R., Corredor, J., Polk, D. B., & Shekels, L. L. (2006). Cysteine-rich domains of muc3 intestinal mucin promote cell migration, inhibit apoptosis, and accelerate wound healing. Gastroenterology, 131(5), 1501–1517.
Gum, J. R., Ho, J. J., Pratt, W. S., Hicks, J. W., Hill, A. S., Vinall, L. E., et al. (1997). MUC3 human intestinal mucin analysis of gene structure, the carboxyl terminus, and a novel upstream repetitive region. Journal of Biological Chemistry, 272(42), 26678–26686.
Tang, J., Zhu, Y., Xie, K., Zhang, X., Zhi, X., Wang, W., Li, Z., Zhang, Q., Wang, L., Wang, J., & Xu, Z. (2016). The role of the AMOP domain in MUC4/Y-promoted tumour angiogenesis and metastasis in pancreatic cancer. Journal of Experimental & Clinical Cancer Research, 35(1), 91.
Kargı, A., Dinç, Z. A., Başok, O., & Üçvet, A. (2006). MUC4 expression and its relation to ErbB2 expression, apoptosis, proliferation, differentiation, and tumor stage in non-small cell lung cancer (NSCLC). Pathology, Research and Practice, 202(8), 577–583.
Songyang, Z., Shoelson, S., McGlade, J., Olivier, P., Pawson, T., Bustelo, X., et al. (1994). Specific motifs recognized by the SH2 domains of Csk, 3BP2, fps/fes, GRB-2, HCP, SHC, Syk, and Vav. Molecular and Cellular Biology, 14(4), 2777–2785.
Williams, S. J., McGuckin, M. A., Gotley, D. C., Eyre, H. J., Sutherland, G. R., & Antalis, T. M. (1999). Two novel mucin genes down-regulated in colorectal cancer identified by differential display. Cancer Research, 59(16), 4083–4089.
Burgel, P., & Nadel, J. (2008). Epidermal growth factor receptor-mediated innate immune responses and their roles in airway diseases. European Respiratory Journal, 32(4), 1068–1081.
Chauhan, S. C., Ebeling, M. C., Maher, D. M., Koch, M. D., Watanabe, A., Aburatani, H., Lio, Y., & Jaggi, M. (2012). MUC13 mucin augments pancreatic tumorigenesis. Molecular Cancer Therapeutics, 11(1), 24–33.
Das, S., Rachagani, S., Torres-Gonzalez, M. P., Lakshmanan, I., Majhi, P. D., Smith, L. M., Wagner, K. U., & Batra, S. K. (2015). Carboxyl-terminal domain of MUC16 imparts tumorigenic and metastatic functions through nuclear translocation of JAK2 to pancreatic cancer cells. Oncotarget, 6(8), 5772–5787.
Yang, B., Wu, A., Hu, Y., Tao, C., Wang, J. M., Lu, Y., & Xing, R. (2019). Mucin 17 inhibits the progression of human gastric cancer by limiting inflammatory responses through a MYH9-p53-RhoA regulatory feedback loop. Journal of Experimental & Clinical Cancer Research, 38(1), 283.
Sheehan, J. K., Brazeau, C., Kutay, S., Pigeon, H., Kirkham, S., Howard, M., et al. (2000). Physical characterization of the MUC5AC mucin: a highly oligomeric glycoprotein whether isolated from cell culture or in vivo from respiratory mucous secretions. Biochemical Journal, 347(1), 37–44.
Sheehan, J. K., Howard, M., Richardson, P. S., Longwill, T., & Thornton, D. J. (1999). Physical characterization of a low-charge glycoform of the MUC5B mucin comprising the gel-phase of an asthmatic respiratory mucous plug. Biochemical Journal, 338(2), 507–513.
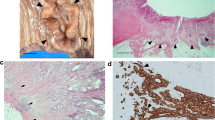
McAuley, J. L., Linden, S. K., Png, C. W., King, R. M., Pennington, H. L., Gendler, S. J., Florin, T. H., Hill, G. R., Korolik, V., & McGuckin, M. A. (2007). MUC1 cell surface mucin is a critical element of the mucosal barrier to infection. The Journal of Clinical Investigation, 117(8), 2313–2324.
McGuckin, M. A., Every, A. L., Skene, C. D., Linden, S. K., Chionh, Y. T., Swierczak, A., McAuley, J., Harbour, S., Kaparakis, M., Ferrero, R., & Sutton, P. (2007). Muc1 mucin limits both Helicobacter pylori colonization of the murine gastric mucosa and associated gastritis. Gastroenterology, 133(4), 1210–1218.
Blalock, T. D., Spurr-Michaud, S. J., Tisdale, A. S., Heimer, S. R., Gilmore, M. S., Ramesh, V., & Gipson, I. K. (2007). Functions of MUC16 in corneal epithelial cells. Investigative Ophthalmology & Visual Science, 48(10), 4509–4518.
Ahmad, R., Raina, D., Joshi, M. D., Kawano, T., Ren, J., Kharbanda, S., & Kufe, D. (2009). MUC1-C oncoprotein functions as a direct activator of the nuclear factor-κB p65 transcription factor. Cancer Research, 69(17), 7013–7021.
Lindén, S. K., Florin, T. H., & McGuckin, M. A. (2008). Mucin dynamics in intestinal bacterial infection. PLoS One, 3(12), e3952.
Ahmad, R., Raina, D., Trivedi, V., Ren, J., Rajabi, H., Kharbanda, S., & Kufe, D. (2007). MUC1 oncoprotein activates the IκB kinase β complex and constitutive NF-κB signalling. Nature Cell Biology, 9(12), 1419–1427.
Smirnova, M. G., Guo, L., Birchall, J. P., & Pearson, J. P. (2003). LPS up-regulates mucin and cytokine mRNA expression and stimulates mucin and cytokine secretion in goblet cells. Cellular Immunology, 221(1), 42–49.
Fischer, B. M., Cuellar, J. G., Diehl, M. L., deFreytas, A. M., Zhang, J., Carraway, K. L., et al. (2003). Neutrophil elastase increases MUC4 expression in normal human bronchial epithelial cells. American Journal of Physiology. Lung Cellular and Molecular Physiology, 284(4), L671–L679.
Delmotte, P., Degroote, S., Lafitte, J.-J., Lamblin, G., Perini, J.-M., & Roussel, P. (2002). Tumor necrosis factor α increases the expression of glycosyltransferases and sulfotransferases responsible for the biosynthesis of sialylated and/or sulfated Lewis x epitopes in the human bronchial mucosa. Journal of Biological Chemistry, 277(1), 424–431.
Lindén, S. K., Wickström, C., Lindell, G., Gilshenan, K., & Carlstedt, I. (2008). Four modes of adhesion are used during Helicobacter pylori binding to human mucins in the oral and gastric niches. Helicobacter, 13(2), 81–93.
Schulz, B. L., Sloane, A. J., Robinson, L. J., Prasad, S. S., Lindner, R. A., Robinson, M., Bye, P. T., Nielson, D. W., Harry, J. L., Packer, N. H., & Karlsson, N. G. (2007). Glycosylation of sputum mucins is altered in cystic fibrosis patients. Glycobiology, 17(7), 698–712.
Xavier, R., & Podolsky, D. (2007). Unravelling the pathogenesis of inflammatory bowel disease. Nature, 448(7152), 427–434.
Feagins, L. A., Souza, R. F., & Spechler, S. J. (2009). Carcinogenesis in IBD: potential targets for the prevention of colorectal cancer. Nature Reviews Gastroenterology & Hepatology, 6(5), 297–305.
Heazlewood, C. K., Cook, M. C., Eri, R., Price, G. R., Tauro, S. B., Taupin, D., Thornton, D. J., Png, C. W., Crockford, T. L., Cornall, R. J., Adams, R., Kato, M., Nelms, K. A., Hong, N. A., Florin, T. H. J., Goodnow, C. C., & McGuckin, M. A. (2008). Aberrant mucin assembly in mice causes endoplasmic reticulum stress and spontaneous inflammation resembling ulcerative colitis. PLoS Medicine, 5(3), e54.
Schwerbrock, N. M., Makkink, M. K., van der Sluis, M., Büller, H. A., Einerhand, A. W., Sartor, R. B., et al. (2004). Interleukin 10-deficient mice exhibit defective colonic Muc2 synthesis before and after induction of colitis by commensal bacteria. Inflammatory Bowel Diseases, 10(6), 811–823.
Karin, M., & Greten, F. R. (2005). NF-κB: linking inflammation and immunity to cancer development and progression. Nature Reviews Immunology, 5(10), 749–759.
Vinall, L. E., King, M., Novelli, M., Green, C. A., Daniels, G., Hilkens, J., Sarner, M., & Swallow, D. M. (2002). Altered expression and allelic association of the hypervariable membrane mucin MUC1 in Helicobacter pylori gastritis. Gastroenterology, 123(1), 41–49.
Kondo, S., Yoshizaki, T., Wakisaka, N., Horikawa, T., Murono, S., Jang, K. L., Joab, I., Furukawa, M., & Pagano, J. S. (2007). MUC1 induced by Epstein-Barr virus latent membrane protein 1 causes dissociation of the cell-matrix interaction and cellular invasiveness via STAT signaling. Journal of Virology, 81(4), 1554–1562.
Vermeer, P. D., Einwalter, L. A., Moninger, T. O., Rokhlina, T., Kern, J. A., Zabner, J., & Welsh, M. J. (2003). Segregation of receptor and ligand regulates activation of epithelial growth factor receptor. Nature, 422(6929), 322–326.
Shin, K., Fogg, V. C., & Margolis, B. (2006). Tight junctions and cell polarity. Annual Review of Cell and Developmental Biology, 22, 207–235.
Polyak, K., & Weinberg, R. A. (2009). Transitions between epithelial and mesenchymal states: acquisition of malignant and stem cell traits. Nature Reviews Cancer, 9(4), 265–273.
Huang, L., Chen, D., Liu, D., Yin, L., Kharbanda, S., & Kufe, D. (2005). MUC1 oncoprotein blocks glycogen synthase kinase 3β–mediated phosphorylation and degradation of β-catenin. Cancer Research, 65(22), 10413–10422.
Huang, L., Ren, J., Chen, D., Li, Y., Kharbanda, S., & Kufe, D. (2003). MUC1 cytoplasmic domain coactivates Wnt target gene transcription and confers transformation. Cancer Biology & Therapy, 2(6), 702–706.
Aranda, V., Haire, T., Nolan, M. E., Calarco, J. P., Rosenberg, A. Z., Fawcett, J. P., Pawson, T., & Muthuswamy, S. K. (2006). Par6–aPKC uncouples ErbB2 induced disruption of polarized epithelial organization from proliferation control. Nature Cell Biology, 8(11), 1235–1245.
Ren, J., Bharti, A., Raina, D., Chen, W., Ahmad, R., & Kufe, D. (2006). MUC1 oncoprotein is targeted to mitochondria by heregulin-induced activation of c-Src and the molecular chaperone HSP90. Oncogene, 25(1), 20–31.
Chaturvedi, P., Singh, A. P., Chakraborty, S., Chauhan, S. C., Bafna, S., Meza, J. L., Singh, P. K., Hollingsworth, M. A., Mehta, P. P., & Batra, S. K. (2008). MUC4 mucin interacts with and stabilizes the HER2 oncoprotein in human pancreatic cancer cells. Cancer Research, 68(7), 2065–2070.
Funes, M., Miller, J. K., Lai, C., Carraway, K. L., & Sweeney, C. (2006). The mucin Muc4 potentiates neuregulin signaling by increasing the cell-surface populations of ErbB2 and ErbB3. Journal of Biological Chemistry, 281(28), 19310–19319.
Pokutta, S., & Weis, W. I. (2007). Structure and mechanism of cadherins and catenins in cell-cell contacts. Annual Review of Cell and Developmental Biology, 23, 237–261.
Inaguma, S., Kasai, K., & Ikeda, H. (2011). GLI1 facilitates the migration and invasion of pancreatic cancer cells through MUC5AC-mediated attenuation of E-cadherin. Oncogene, 30(6), 714–723.
Labelle, M., & Hynes, R. O. (2012). The initial hours of metastasis: the importance of cooperative host–tumor cell interactions during hematogenous dissemination. Cancer Discovery, 2(12), 1091–1099.
Kumar, S., Cruz, E., Joshi, S., Patel, A., Jahan, R., Batra, S. K., & Jain, M. (2017). Genetic variants of mucins: unexplored conundrum. Carcinogenesis, 38(7), 671–679.
Ponnusamy, P. M., Seshacharyulu, P., Lakshmanan, I., Vaz, A. P., Chugh, S., & Batra, K. S. (2013). Emerging role of mucins in epithelial to mesenchymal transition. Current Cancer Drug Targets, 13(9), 945–956.
Chugh, S., Gnanapragassam, V. S., Jain, M., Rachagani, S., Ponnusamy, M. P., & Batra, S. K. (2015). Pathobiological implications of mucin glycans in cancer: sweet poison and novel targets. Biochimica et Biophysica Acta (BBA)-Reviews on Cancer, 1856(2), 211–225.
Byrd, J. C., & Bresalier, R. S. (2004). Mucins and mucin binding proteins in colorectal cancer. Cancer and Metastasis Reviews, 23(1–2), 77–99.
Horn, G., Gaziel, A., Wreschner, D. H., Smorodinsky, N. I., & Ehrlich, M. (2009). ERK and PI3K regulate different aspects of the epithelial to mesenchymal transition of mammary tumor cells induced by truncated MUC1. Experimental Cell Research, 315(8), 1490–1504.
Rajabi, H., Ahmad, R., Jin, C., Joshi, M. D., Guha, M., Alam, M., Kharbanda, S., & Kufe, D. (2012). MUC1-C oncoprotein confers androgen-independent growth of human prostate cancer cells. Prostate, 72(15), 1659–1668. https://doi.org/10.1002/pros.22519.
Chaturvedi, P., Singh, A. P., Chakraborty, S., Chauhan, S. C., Bafna, S., Meza, J. L., Singh, P. K., Hollingsworth, M. A., Mehta, P. P., & Batra, S. K. (2008). MUC4 mucin interacts with and stabilizes the HER2 oncoprotein in human pancreatic cancer cells. Cancer Research, 68(7), 2065–2070. https://doi.org/10.1158/0008-5472.CAN-07-6041.
Ponnusamy, M. P., Singh, A. P., Jain, M., Chakraborty, S., Moniaux, N., & Batra, S. K. (2008). MUC4 activates HER2 signalling and enhances the motility of human ovarian cancer cells. British Journal of Cancer, 99(3), 520–526. https://doi.org/10.1038/sj.bjc.6604517.
Rachagani, S., Macha, M. A., Ponnusamy, M. P., Haridas, D., Kaur, S., Jain, M., & Batra, S. K. (2012). MUC4 potentiates invasion and metastasis of pancreatic cancer cells through stabilization of fibroblast growth factor receptor 1. Carcinogenesis, 33(10), 1953–1964. https://doi.org/10.1093/carcin/bgs225.
Mukhopadhyay, P., Lakshmanan, I., Ponnusamy, M. P., Chakraborty, S., Jain, M., Pai, P., Smith, L. M., Lele, S. M., & Batra, S. K. (2013). MUC4 overexpression augments cell migration and metastasis through EGFR family proteins in triple negative breast cancer cells. PLoS One, 8(2), e54455. https://doi.org/10.1371/journal.pone.0054455.
Majhi, P. D., Lakshmanan, I., Ponnusamy, M. P., Jain, M., Das, S., Kaur, S., Shimizu, S. T., West, W. W., Johansson, S. L., Smith, L. M., Yu, F., Rolle, C. E., Sharma, P., Carey, G. B., Batra, S. K., & Ganti, A. K. (2013). Pathobiological implications of MUC4 in non-small-cell lung cancer. Journal of Thoracic Oncology, 8(4), 398–407. https://doi.org/10.1097/JTO.0b013e3182829e06.
Muniyan, S., Haridas, D., Chugh, S., Rachagani, S., Lakshmanan, I., Gupta, S., Seshacharyulu, P., Smith, L. M., Ponnusamy, M. P., & Batra, S. K. (2016). MUC16 contributes to the metastasis of pancreatic ductal adenocarcinoma through focal adhesion mediated signaling mechanism. Genes & Cancer, 7(3–4), 110–124.
Haridas, D., Ponnusamy, M. P., Chugh, S., Lakshmanan, I., Seshacharyulu, P., & Batra, S. K. (2014). MUC16: molecular analysis and its functional implications in benign and malignant conditions. The FASEB Journal, 28(10), 4183–4199. https://doi.org/10.1096/fj.14-257352.
Comamala, M., Pinard, M., Theriault, C., Matte, I., Albert, A., Boivin, M., et al. (2011). Downregulation of cell surface CA125/MUC16 induces epithelial-to-mesenchymal transition and restores EGFR signalling in NIH:OVCAR3 ovarian carcinoma cells. British Journal of Cancer, 104(6), 989–999. https://doi.org/10.1038/bjc.2011.34.
Thériault, C., Pinard, M., Comamala, M., Migneault, M., Beaudin, J., Matte, I., Boivin, M., Piché, A., & Rancourt, C. (2011). MUC16 (CA125) regulates epithelial ovarian cancer cell growth, tumorigenesis and metastasis. Gynecologic Oncology, 121(3), 434–443.
Lakshmanan, I., Rachagani, S., Hauke, R., Krishn, S. R., Paknikar, S., Seshacharyulu, P., Karmakar, S., Nimmakayala, R. K., Kaushik, G., Johansson, S. L., Carey, G. B., Ponnusamy, M. P., Kaur, S., Batra, S. K., & Ganti, A. K. (2016). MUC5AC interactions with integrin beta4 enhances the migration of lung cancer cells through FAK signaling. Oncogene, 35(31), 4112–4121. https://doi.org/10.1038/onc.2015.478.
Pothuraju, R., Rachagani, S., Krishn, S. R., Chaudhary, S., Nimmakayala, R. K., Siddiqui, J. A., Ganguly, K., Lakshmanan, I., Cox, J. L., Mallya, K., Kaur, S., & Batra, S. K. (2020). Molecular implications of MUC5AC-CD44 axis in colorectal cancer progression and chemoresistance. Molecular Cancer, 19(1), 37. https://doi.org/10.1186/s12943-020-01156-y.
Yamazoe, S., Tanaka, H., Sawada, T., Amano, R., Yamada, N., Ohira, M., & Hirakawa, K. (2010). RNA interference suppression of mucin 5AC (MUC5AC) reduces the adhesive and invasive capacity of human pancreatic cancer cells. Journal of Experimental & Clinical Cancer Research, 29, 53. https://doi.org/10.1186/1756-9966-29-53.
Truant, S., Bruyneel, E., Gouyer, V., De Wever, O., Pruvot, F. R., Mareel, M., et al. (2003). Requirement of both mucins and proteoglycans in cell-cell dissociation and invasiveness of colon carcinoma HT-29 cells. International Journal of Cancer, 104(6), 683–694. https://doi.org/10.1002/ijc.11011.
Chang, J., & Chaudhuri, O. (2019). Beyond proteases: basement membrane mechanics and cancer invasion. The Journal of Cell Biology, 218(8), 2456–2469. https://doi.org/10.1083/jcb.201903066.
Senapati, S., Gnanapragassam, V. S., Moniaux, N., Momi, N., & Batra, S. K. (2012). Role of MUC4-NIDO domain in the MUC4-mediated metastasis of pancreatic cancer cells. Oncogene, 31(28), 3346–3356. https://doi.org/10.1038/onc.2011.505.
Jahan, R., Macha, M. A., Rachagani, S., Das, S., Smith, L. M., Kaur, S., & Batra, S. K. (2018). Axed MUC4 (MUC4/X) aggravates pancreatic malignant phenotype by activating integrin-beta1/FAK/ERK pathway. Biochimica et Biophysica Acta - Molecular Basis of Disease, 1864(8), 2538–2549. https://doi.org/10.1016/j.bbadis.2018.05.008.
Leir, S. H., & Harris, A. (2011). MUC6 mucin expression inhibits tumor cell invasion. Experimental Cell Research, 317(17), 2408–2419. https://doi.org/10.1016/j.yexcr.2011.07.021.
Erpenbeck, L., & Schon, M. P. (2010). Deadly allies: the fatal interplay between platelets and metastasizing cancer cells. Blood, 115(17), 3427–3436. https://doi.org/10.1182/blood-2009-10-247296.
Hook, P., Litvinov, R. I., Kim, O. V., Xu, S., Xu, Z., Bennett, J. S., et al. (2017). Strong binding of platelet integrin alphaIIbbeta3 to fibrin clots: potential target to destabilize thrombi. Scientific Reports, 7(1), 13001. https://doi.org/10.1038/s41598-017-12615-w.
Rowson-Hodel, A. R., Wald, J. H., Hatakeyama, J., O’Neal, W. K., Stonebraker, J. R., VanderVorst, K., Saldana, M. J., Borowsky, A. D., Sweeney, C., & Carraway 3rd, K. L. (2018). Membrane Mucin Muc4 promotes blood cell association with tumor cells and mediates efficient metastasis in a mouse model of breast cancer. Oncogene, 37(2), 197–207. https://doi.org/10.1038/onc.2017.327.
Bambach, S. K., & Lammermann, T. (2017). Platelets, on your marks, get set, migrate! Cell, 171(6), 1256–1258. https://doi.org/10.1016/j.cell.2017.11.026.
Joyce, J. A., & Pollard, J. W. (2009). Microenvironmental regulation of metastasis. Nature Reviews. Cancer, 9(4), 239–252. https://doi.org/10.1038/nrc2618.
McEver, R. P. (2015). Selectins: initiators of leucocyte adhesion and signalling at the vascular wall. Cardiovascular Research, 107(3), 331–339. https://doi.org/10.1093/cvr/cvv154.
Kam, J. L., Regimbald, L. H., Hilgers, J. H., Hoffman, P., Krantz, M. J., Longenecker, B. M., & Hugh, J. C. (1998). MUC1 synthetic peptide inhibition of intercellular adhesion molecule-1 and MUC1 binding requires six tandem repeats. Cancer Research, 58(23), 5577–5581.
von Mensdorff-Pouilly, S., Snijdewint, F. G., Verstraeten, A. A., Verheijen, R. H., & Kenemans, P. (2000). Human MUC1 mucin: a multifaceted glycoprotein. The International Journal of Biological Markers, 15(4), 343–356.
Park, J., Wysocki, R. W., Amoozgar, Z., Maiorino, L., Fein, M. R., Jorns, J., et al. (2016). Cancer cells induce metastasis-supporting neutrophil extracellular DNA traps. Science Translational Medicine, 8(361), 361ra138. https://doi.org/10.1126/scitranslmed.aag1711.
Acknowledgments
We thank Dr. Jessica Mercer for editorial contribution to the manuscript.
Funding
This authors’ work was partly supported by funding from the National Institutes of Health (P01CA217798, U01 CA210240, U01 CA200466, R01 CA206444, R01 CA228524, and R01 CA195586).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
SKB is one of the co-founders of the Sanguine Diagnostic and Therapeutics, Inc.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ganguly, K., Rauth, S., Marimuthu, S. et al. Unraveling mucin domains in cancer and metastasis: when protectors become predators. Cancer Metastasis Rev 39, 647–659 (2020). https://doi.org/10.1007/s10555-020-09896-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10555-020-09896-5