Abstract
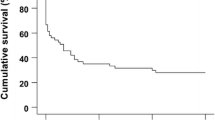
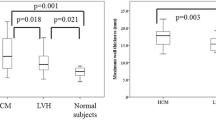
A large animal model of chronic coronary artery disease (CAD) is crucial for the understanding the underlying pathophysiological processes of chronic CAD and consequences for cardiac structure and function. The goal of this study was to develop a chronic model of CAD in a swine model and to evaluate the changes of myocardial structure, myocardial motility, and myocardial viability during coronary stenosis. A total of 30 swine (including 24 experimental animals and 6 controls) were enrolled. The chronic ischemia model was constructed by using Ameroid constrictor in experimental group. The 24 experimental animals were further divided into 4 groups (6 animals in each group) and were sacrificed at 1, 2, 3 and 4 weeks after operation for pathological examination, respectively. Cardiac magnetic resonance (CMR) was performed preoperatively and weekly postoperatively until sacrificed both in experimental and control group. CMR cine images, rest/adenosine triphosphate (ATP) stress myocardial contrast perfusion and LGE were performed and analyzed. The rest wall thickening (WT) score was calculated from rest cine images. The MPRI (myocardial perfusion reserve index) and MPR (myocardial perfusion reserve) were calculated based on rest and stress perfusion images. Pathology staining including triphenyltetrazolium chloride, HE and picrosirus red staining were performed after swine were sacrificed and collagen volume fraction (CVF) was calculated. The time to formation of ischemic, hibernating, and infarcted myocardium was recorded. In experimental group, from 1w to 4w after surgery, the rest WT score decreased gradually from 35.2 ± 2.0%, 32.0 ± 2.9% to 30.5 ± 3.0% and finally 29.06 ± 1.78%, p < 0.001. Left ventricular ejection fraction was gradually impaired after modeling (58.9 ± 12.6%, 56.3 ± 10.1%, 55.3 ± 9.0%, 53.8 ± 9.9%, respectively). And the MPR and MPRI also decreased stepwise with extent of surgery time (MPRI dropped from 2.1 ± 0.4, 2.0 ± 0.2 to 1.8 ± 0.3 and finally 1.7 ± 0.1, p = 0.004; MPR dropped from 2.3 ± 0.4, 2.1 ± 0.2 to 1.9 ± 0.4 and finally 1.8 ± 0.1, p < 0.001). Stronger associations between MPR, MPRI and CVF were paralleled lower wall thickening scores in fibrosis-affected areas. The ischemic myocardium was first appeared in the first week after surgery (involving ten segments), hibernated myocardium was first appeared in the second week after surgery (involving seventeen segments). LGE was first appeared in eight swine in the third weeks after surgery (16 segments). At 4w after surgery, average 9.6 g scar tissue was found among 6 swine. At the same time, histological analysis established the presence of fibrosis and ongoing apoptosis in the infarcted area. In conclusion, our study provided valuable insights into the pathophysiological processes of chronic CAD and its consequences for cardiac structure and function in a large animal model through combining myocardial motion and stress perfusion.





Similar content being viewed by others
References
Roger VL (2021) Epidemiology of Heart Failure: a contemporary perspective. Circ Res 128(10):1421–1434
Khatibzadeh S, Farzadfar F, Oliver J, Ezzati M, Moran A (2013) Worldwide risk factors for Heart Failure: a systematic review and pooled analysis. Int J Cardiol 168(2):1186–1194
Caillaud D, Calderon J, Reant P, Lafitte S, Dos Santos P, Couffinhal T, Roques X, Barandon L Echocardiographic analysis with a twodimensional strain of chronic myocardial ischemia induced with ameroid constrictor in the pig. Interact Cardiovasc Thorac Surg 10: 689 – 693, 2010.
Hughes GC, Post MJ, Simons M, Annex BH Translational physiology: porcine models of human coronary artery Disease: implications for preclinical trials of therapeutic angiogenesis. J Appl Physiol 94: 1689 – 1701, 2003.
Heusch G (2021) Myocardial stunning and hibernation revisited. Nat Rev Cardiol 18(7):522–536
Giordano C, Kuraitis D, Beanlands RS, Suuronen EJ, Ruel M (2013) Cell-based vasculogenic studies in preclinical models of chronic myocardial ischaemia and hibernation. Expert Opin Biol Ther 13(3):411–428
Keeran KJ, Jeffries KR, Zetts AD, Taylor J, Kozlov S, Hunt TJ (2017) A chronic Cardiac Ischemia Model in Swine using an Ameroid Constrictor. J Vis Exp. ;(128):56190
Russo V, Lovato L, Ligabue G (2020) Cardiac MRI: technical basis. Radiol Med 125(11):1040–1055
Arifin WN, Zahiruddin WM (2017) Sample size calculation in animal studies using resource equation approach. Malays J Med Sci 24(5):101–105
Cui C, Wang S, Lu M et al (2018) Detection of recent Myocardial Infarction using native T1 mapping in a swine model: a validation study. Sci Rep 8(1):739
Kramer CM, Barkhausen J, Bucciarelli-Ducci C, Flamm SD, Kim RJ, Nagel E (2020) Standardized cardiovascular magnetic resonance imaging (CMR) protocols: 2020 update. J Cardiovasc Magn Reson 22:17
Manisty C, Ripley DP, Herrey AS et al (2015) Splenic Switch-off: a Tool to assess stress adequacy in Adenosine Perfusion Cardiac MR Imaging. Radiology 276(3):732–740
Zhuang Baiyan C, Chen S, Arlene H, Jian W, Xin Y, Guangxin et al (2020) Detection of myocardial fibrosis and left ventricular dysfunction with Cardiac MRI in a Hypertensive Swine Model. Radiol Cardiothorac Imaging, 2(4), e190214
Zhang F, Wang J, Shao X et al (2021) Incremental value of myocardial wall motion and thickening to perfusion alone by gated SPECT myocardial perfusion imaging for viability assessment in patients with ischemic Heart Failure. J Nucl Cardiol 28(6):2545–2556
Cerqueira MD, Weissman NJ, Dilsizian V et al (2002) Standardized myocardial segmentation and nomenclature for tomographic imaging of the heart. A statement for healthcare professionals from the Cardiac Imaging Committee of the Council on Clinical Cardiology of the American Heart Association. Circulation 105(4):539–542
Gallik DM, Obermueller SD, Swarna US et al (1995) Simultaneous assessment of myocardial perfusion and left ventricular function during transient Coronary Occlusion. J Am Coll Cardiol 25:1529–1538
Ma P, Liu J, Hu Y, Zhou X, Shang Y, Wang J (2022) Histologic validation of stress cardiac magnetic resonance T1-mapping techniques for detection of coronary microvascular dysfunction in rabbits. Int J Cardiol 347:76–82
Everaars H, van Diemen PA, Bom MJ et al (2020) Comparison between quantitative cardiac magnetic resonance perfusion imaging and [15O]H2O positron emission tomography. Eur J Nucl Med Mol Imaging 47(7):1688–1697
Erbel C, Mukhammadaminova N, Gleissner CA et al (2016) Myocardial Perfusion Reserve and strain-encoded CMR for evaluation of Cardiac Allograft Microvasculopathy. JACC Cardiovasc Imaging 9(3):255–266
van Assen M, van Dijk R, Kuijpers D, Vliegenthart R, Oudkerk M (2019) T1 reactivity as an imaging biomarker in myocardial tissue characterization discriminating normal, ischemic and infarcted myocardium. Int J Cardiovasc Imaging 35:1319–1325
Heusch G (2021) Myocardial stunning and hibernation revisited. Nat Reviews Cardiol 18:522–536
Yang MX, Xu HY, Zhang L, Chen L, Xu R, Fu H, Liu H, Li XS, Fu C, Liu KL et al (2021) Myocardial perfusion assessment in the infarct core and penumbra zones in an in-vivo porcine model of the acute, sub-acute, and chronic infarction. Eur Radiol 31:2798–2808
Fishbein MC, Meerbaum S, Rit J et al (1981) Early phase acute myocardial infarct size quantification: validation of the triphenyl tetrazolium chloride tissue enzyme staining technique. Am Heart J 101:593–600
Child N, Suna G, Dabir D et al (2018) Comparison of MOLLI, shMOLLLI, and SASHA in discrimination between health and Disease and relationship with histologically derived collagen volume fraction. Eur Heart J Cardiovasc Imaging 19:768–776
Martínez-Milla J, Galán-Arriola C, Carnero M et al (2020) Translational large animal model of hibernating myocardium: characterization by serial multimodal imaging. Basic Res Cardiol 115(3):33
Ishikawa K, Ladage D, Takewa Y et al (2011) Development of a preclinical model of ischemic cardiomyopathy in swine. Am J Physiol Heart Circ Physiol 301(2):H530–H537
Lu JK, Zhu C, Jing H, Wang YJ, Qing EM (2012) Application of intraoperative arterial pressure-based cardiac output monitoring for patients undergoing coronary artery bypass grafting Surgery. Chin Med J (Engl) 125(12):2099–2103
Cwajg JM, Cwajg E, Nagueh SF et al (2000) End-diastolic wall thickness as a predictor of recovery of function in myocardial hibernation: relation to rest-redistribution Tl-201 tomography and dobutamine stress echocardiography. J Am Coll Cardiol 35:1152–1161
Caillaud D, Calderon J, Reant P, Lafitte S, Dos Santos P, Couffinhal T, Roques X, Barandon L (2010) Echocardiographic analysis with a two-dimensional strain of chronic myocardial ischemia induced with ameroid constrictor in the pig. Interact Cardiovasc Thorac Surg 10:689–693
Sánchez-González J, Fernandez-Jiménez R, Nothnagel ND, LópezMartín G, Fuster V, Ibañez B (2015) Optimization of dual-saturation single bolus acquisition for quantitative cardiac perfusion and myocardial blood flow maps. J Cardiovasc Magn Reson 17(1):21
Schuster A, Zarinabad N, Ishida M et al (2014) Quantitative assessment of magnetic resonance derived myocardial perfusion measurements using advanced techniques: microsphere validation in an explanted pig heart system. J Cardiovasc Magn Reson 16(1):82
Van Houten M, Yang Y, Hauser A et al (2019) Adenosine stress CMR perfusion imaging of the temporal evolution of perfusion defects in a porcine model of Progressive obstructive coronary artery occlusion. NMR Biomed 32(11):e4136
Lindsey ML, Bolli R, Canty JM Jr et al (2018) Guidelines for experimental models of myocardial ischemia and infarction. Am J Physiol Heart Circ Physiol 314(4):H812–H838
Anagnostopoulos C, Georgakopoulos A, Pianou N, Nekolla SG (2013) Assessment of myocardial perfusion and viability by positron emission tomography. Int J Cardiol 167(5):1737–1749
Wang L, Lu MJ, Feng L et al (2019) Relationship of myocardial hibernation, scar, and angiographic collateral flow in ischemic cardiomyopathy with coronary chronic total occlusion. J Nucl Cardiol 26(5):1720–1730
Löffler AI, Kramer CM (2018) Myocardial viability testing to Guide Coronary revascularization. Interv Cardiol Clin 7(3):355–365
Funding
This study was supported in part by research grants from the National Natural Science Foundation of China (No. 81971588), the Construction Research Project of Key Laboratory (Cultivation) of the Chinese Academy of Medical Sciences (No. 2019PT310025), the Clinical and Translational Fund of the Chinese Academy of Medical Sciences (No. 2019XK320063), Capital’s Funds for Health Improvement and Research (CFH 2020-2-4034) and the Clinically Characteristic Applied Research Fund (No. Z191100006619021).
Author information
Authors and Affiliations
Contributions
Guarantors of integrity of entire study, B.Z., C.C., J.H., J.X., XS., X.D., L.L., S.L., X.W., M.L.; study concepts/study design or data acquisition or data analysis/interpretation, J.H., S.Z., W.Y., L.Z. D.Z., M.L.; experimental studies, B.Z., C.C., J.X., W.W., X.W., M.L.; statistical analysis, B.Z.; and manuscript editing, B.Z., X.D., A.S., M.L.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Consent to participate
The informed consent wasn’t available because this research is an animal study.
Consent to publish
The data and photographs are available.
Conflict of interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhuang, B., Cui, C., He, J. et al. Developing and evaluating a chronic ischemic cardiomyopathy in swine model by rest and stress CMR. Int J Cardiovasc Imaging 40, 249–260 (2024). https://doi.org/10.1007/s10554-023-02999-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-023-02999-4