Abstract
Purpose
Recently developed handheld ultrasound devices (HHUD) represent a promising method to evaluate the cardiovascular abnormalities at the point of care. However, this technology has not been rigorously evaluated. The aim of this study was to explore the correlation and the agreement between the LVEF (Left Ventricular Ejection Fraction) visually assessed by a moderately experienced sonographer using an HHUD compared to the routine LVEF assessment performed at the Echocardiography Laboratory.
Methods
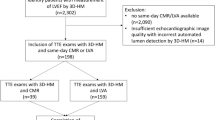
This was a prospective single center study which enrolled 120 adult inpatients and outpatients referred for a comprehensive Echocardiography (EC).
Results
The mean age of the patients was 69.9 ± 12.5 years. There were 47 females (39.2%). The R-squared was r 0.94 (p < 0.0001) and the ICC was 0.93 (IC 95% 0.91–0.95, p ≤ 0.0001). The Bland-Altman plot showed limits of agreement (LOA): Upper LOA 10.61 and Lower LOA − 8.95. The overall agreement on the LVEF assessment when it was stratified as “normal” or “reduced” was 89.1%, with a kappa of 0.77 (p < 0.0001). When the LVEF was classified as “normal”, “mildly reduced”, “moderately reduced”, or “severely reduced,” the kappa was 0.77 (p < 0.0001). The kappa between the HHUD EC and the comprehensive EC for the detection of RWMAs in the territories supplied by the LAD, LCX and RCA was 0.85, 0.73 and 0.85, respectively.
Conclusion
With current HHUD, an averagely experienced operator can accurately bedside visual estimate the LVEF. This may facilitate the incorporation of this technology in daily clinical practice improving the management of patients.





Similar content being viewed by others
References
Otto CM, Nishimura RA, Bonow RO et al (2021) 2020 ACC/AHA Guideline for the management of patients with Valvular Heart Disease: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation 143(5):E72–E227. https://doi.org/10.1161/CIR.0000000000000923
Mor-Avi V, Lang RM, Badano LP et al (2011) Current and evolving echocardiographic techniques for the quantitative evaluation of Cardiac mechanics: ASE/EAE Consensus Statement on Methodology and indications. J Am Soc Echocardiogr 24(3):277–313. https://doi.org/10.1016/j.echo.2011.01.015
Bruce CJ, Montgomery SC, Bailey KR, Tajik J, Seward JB (2002) Utility of hand-carried ultrasound devices used by cardiologists with and without significant echocardiographic experience in the cardiology inpatient and outpatient settings. Am J Cardiol 90(11):1273–1275. https://doi.org/10.1016/S0002-9149(02)02853-9
Kimura BJ, Bocchicchio M, Willis CL, DeMaria AN (2001) Screening cardiac ultrasonographic examination in patients with suspected cardiac disease in the emergency department. Am Heart J 142(2):324–330. https://doi.org/10.1067/mhj.2001.116475
Vignon P, Frank MBJ, Lesage J et al (2004) Hand-held echocardiography with doppler capability for the assessment of critically-ill patients: is it reliable? Intensive Care Med 30(4):718–723. https://doi.org/10.1007/s00134-003-2128-x
Amiel JB, Grümann A, Lhéritier G et al (2012) Assessment of left ventricular ejection fraction using an ultrasonic stethoscope in critically ill patients. Crit Care 16(1). https://doi.org/10.1186/cc11198
Lafon T, Appert A, Hadj M et al (2020) Comparative early hemodynamic profiles in patients presenting to the emergency department with septic and nonseptic acute circulatory failure using focused echocardiography. Shock 53(6):695–700. https://doi.org/10.1097/SHK.0000000000001449
Vourvouri EC, Schinkel AFL, Roelandt JRTC et al (2003) Screening for left ventricular dysfunction using a hand-carried Cardiac Ultrasound device. Vol 5.;
Fedson S, Neithardt G, Thomas P et al (2003) Unsuspected clinically important findings detected with a small portable Ultrasound device in patients admitted to a General Medicine Service. J Am Soc Echocardiogr 16(9):901–905. https://doi.org/10.1016/S0894-7317(03)00426-7
DeCara JM, Lang RM, Koch R, Bala R, Penzotti J, Spencer KT (2003) The use of small personal ultrasound devices by internists without formal training in echocardiography. Eur J Echocardiography 4(2):141–147. https://doi.org/10.1053/euje.2002.0617
Galasko GIW, Lahiri A, Senior R (2003) Portable echocardiography: an innovative tool in screening for cardiac abnormalities in the community. Eur J Echocardiography 4(2):119–127. https://doi.org/10.1053/euje.2002.0627
Wu EB, Brilakis ES, Mashayekhi K et al (2021) Global chronic total occlusion crossing algorithm. J Am Coll Cardiol 78(8):840–853. https://doi.org/10.1016/j.jacc.2021.05.055
Bustam A, Azhar MN, Veriah RS, Arumugam K, Loch A (2014) Performance of emergency physicians in point-of-care echocardiography following limited training. Emerg Med J 31(5):369–373. https://doi.org/10.1136/emermed-2012-201789
Alexander JH, Peterson ED, Chen AY, Harding TM, Adams DB, Kisslo JA (2004) Feasibility of point-of-care echocardiography by internal medicine house staff. Am Heart J 147(3):476–481. https://doi.org/10.1016/j.ahj.2003.10.010
Xie T, Chamoun AJ, Mcculloch M, Tsiouris N, Birnbaum Y, Ahmad M Rapid Screening of Cardiac patients with a miniaturized hand-held Ultrasound Imager-Comparisons with physical examination and conventional Two-Dimensional Echocardiography
Hannan MM, Xie R, Cowger J et al (2019) Epidemiology of infection in mechanical circulatory support: a global analysis from the ISHLT mechanically assisted Circulatory Support Registry. J Heart Lung Transplantation 38(4):364–373. https://doi.org/10.1016/j.healun.2019.01.007
Kobal SL, Trento L, Baharami S et al (2005) Comparison of effectiveness of hand-carried ultrasound to bedside cardiovascular physical examination. Am J Cardiol 96(7):1002–1006. https://doi.org/10.1016/j.amjcard.2005.05.060
Perez-Avraham G, Kobal SL, Etzion O et al (2010) Left ventricular geometric abnormality screening in hypertensive patients using a hand-carried ultrasound device. J Clin Hypertens 12(3):181–186. https://doi.org/10.1111/j.1751-7176.2009.00247.x
Kirkpatrick JN, Ghani SN, Spencer KT (2008) Hand carried echocardiography screening for LV systolic dysfunction in a pulmonary function laboratory. Eur J Echocardiography 9(3):381–383. https://doi.org/10.1016/j.euje.2007.06.013
Ghani SN, Kirkpatrick JN, Spencer KT et al (2006) Rapid assessment of left ventricular systolic function in a pacemaker clinic using a hand-carried ultrasound device. J Interventional Cardiac Electrophysiol 16(1):39–43. https://doi.org/10.1007/s10840-006-9011-y
López-Palmero S, Bolivar-Herrera N, López-Lloret G, Merchán-Ortega G, Macancela-Quiñones JJ, López-Martínez G (2015) Diagnostic utility of handheld ultrasonography as an extension of the physical examination of patients with heart failure. Revista Clínica Española (English Edition) 215(4):204–210. https://doi.org/10.1016/j.rceng.2015.01.002
Martin LD, Howell EE, Ziegelstein RC et al (2009) Hand-carried Ultrasound performed by Hospitalists: does it improve the Cardiac Physical examination? Am J Med 122(1):35–41. https://doi.org/10.1016/j.amjmed.2008.07.022
Lucas BP, Candotti C, Margeta B et al (2011) Hand-carried echocardiography by hospitalists: a randomized trial. Am J Med 124(8):766–774. https://doi.org/10.1016/j.amjmed.2011.03.029
Lucas BP, Candotti C, Margeta B et al (2009) Diagnostic accuracy of hospitalist-performed hand-carried ultrasound echocardiography after a brief training program. J Hosp Med 4(6):340–349. https://doi.org/10.1002/jhm.438
Melamed R, Sprenkle MD, Ulstad VK, Herzog CA, Leatherman JW (2009) Assessment of left ventricular function by intensivists using hand-held echocardiography. Chest 135(6):1416–1420. https://doi.org/10.1378/chest.08-2440
Liebo MJ, Israel RL, Lillie EO, Smith MR, Rubenson DS, Topol EJ (2011) Is pocket mobile echocardiography the next-generation stethoscope? A cross-sectional comparison of rapidly acquired images with standard transthoracic echocardiography. Ann Intern Med 155(1):33–39. https://doi.org/10.7326/0003-4819-155-1-201107050-00005
Razi R, Estrada JR, Doll J, Spencer KT (2011) Bedside hand-carried ultrasound by internal medicine residents versus traditional clinical assessment for the identification of systolic dysfunction in patients admitted with decompensated heart failure. J Am Soc Echocardiogr 24(12):1319–1324. https://doi.org/10.1016/j.echo.2011.07.013
Olesen LL, Andersen A, Thaulow S (2015) Hand-held echocardiography is useful for diagnosis of left systolic dysfunction in an elderly population. Dan Med J 62:7
Andersen GN, Haugen BO, Graven T, Salvesen Ø, Mjølstad OC, Dalen H (2011) Feasibility and reliability of point-of-care pocket-sized echocardiography. Eur J Echocardiography 12(9):665–670. https://doi.org/10.1093/ejechocard/jer108
Mjølstad OC, Andersen GN, Dalen H et al (2013) Feasibility and reliability of point-of-care pocket-size echocardiography performed by medical residents. Eur Heart J Cardiovasc Imaging 14(12):1195–1202. https://doi.org/10.1093/ehjci/jet062
Biais M, Carrié C, Delaunay F, Morel N, Revel P, Janvier G (2012) Evaluation of a new pocket echoscopic device for focused cardiac ultrasonography in an emergency setting. Crit Care 16(3). https://doi.org/10.1186/cc11340
Panoulas VF, Daigeler AL, Malaweera ASN et al (2013) Pocket-size hand-held cardiac ultrasound as an adjunct to clinical examination in the hands of medical students and junior doctors. Eur Heart J Cardiovasc Imaging 14(4):323–330. https://doi.org/10.1093/ehjci/jes140
Filipiak-Strzecka D, John B, Kasprzak J, Michalski B, Lipiec P (2013) Pocket-size echocardiograph-a valuable tool for nonexperts or just a portable device for echocardiographers. Adv Med Sci 58(1):67–72. https://doi.org/10.2478/v10039-012-0054-2
Cullen MW, Blauwet LA, Vatury OM et al (2014) Diagnostic capability of comprehensive handheld vs transthoracic echocardiography. Mayo Clin Proc 89(6):790–798. https://doi.org/10.1016/j.mayocp.2013.12.016
Stokke TM, Ruddox V, Sarvari SI, Otterstad JE, Aune E, Edvardsen T (2014) Brief group training of medical students in focused cardiac ultrasound may improve diagnostic accuracy of physical examination. J Am Soc Echocardiogr 27(11):1238–1246. https://doi.org/10.1016/j.echo.2014.08.001
Ruddox V, Stokke TM, Edvardsen T et al (2013) The diagnostic accuracy of pocket-size cardiac ultrasound performed by unselected residents with minimal training. Int J Cardiovasc Imaging 29(8):1749–1757. https://doi.org/10.1007/s10554-013-0278-7
Mehta M, Jacobson T, Peters D et al (2014) Handheld Ultrasound Versus Physical examination in patients referred for Transthoracic Echocardiography. for a Suspected Cardiac Condition.
Mancuso FJN, Siqueira VN, Moisés VA et al (2014) Focused cardiac ultrasound using a Pocket-Size device in the emergency room. Arq Bras Cardiol 103(6):530–537. https://doi.org/10.5935/abc.20140158
Ünlüer EE, Karagöz A, Akoǧlu H, Bayata S (2014) Visual estimation of bedside echocardiographic ejection fraction by emergency physicians. Western J Emerg Med 15(2):221–226. https://doi.org/10.5811/westjem.2013.9.16185
Khan HA, Wineinger NE, Uddin PQ, Mehta HS, Rubenson DS, Topol EJ (2014) Can hospital rounds with pocket ultrasound by cardiologists reduce standard echocardiography? Am J Med 127(7):669e. 1-669.e7
Johnson BK, Tierney DM, Rosborough TK, Harris KM, Newell MC (2016) Internal medicine point-of-care ultrasound assessment of left ventricular function correlates with formal echocardiography. J Clin Ultrasound 44(2):92–99. https://doi.org/10.1002/jcu.22272
Bhavnani SP, Sola S, Adams D et al (2018) A Randomized Trial of Pocket-Echocardiography Integrated Mobile Health device assessments in Modern Structural Heart Disease clinics. JACC Cardiovasc Imaging 11(4):546–557. https://doi.org/10.1016/j.jcmg.2017.06.019
Moulson N, Jaff Z, Wiltshire V et al (2019) Feasibility and reliability of Nonexpert POCUS for Cardiovascular Preparticipation Screening of Varsity athletes: the SHARP Protocol. Can J Cardiol 35(1):35–41. https://doi.org/10.1016/j.cjca.2018.11.003
Nilsson G, Söderström L, Alverlind K, Samuelsson E, Mooe T (2019) Hand-held cardiac ultrasound examinations performed in primary care patients by nonexperts to identify reduced ejection fraction. BMC Med Educ 19(1). https://doi.org/10.1186/s12909-019-1713-9
Wejner-Mik P, Kasprzak JD, Filipiak-Strzecka D, Miśkowiec D, Lorens A, Lipiec P (2019) Personal mobile device-based pocket echocardiograph—the diagnostic value and clinical utility. Adv Med Sci 64(1):157–161. https://doi.org/10.1016/j.advms.2018.11.003
Aldaas OM, Igata S, Raisinghani A, Kraushaar M, DeMaria AN (2019) Accuracy of left ventricular ejection fraction determined by automated analysis of handheld echocardiograms: a comparison of experienced and novice examiners. Echocardiography 36(12):2145–2151. https://doi.org/10.1111/echo.14546
Rana S, Shrestha BK, Pant C, Adhikari S, Regmi S (2020) Left ventricle ejection fraction estimation by point of care echocardiography in patients admitted in intensive care unit. J Chitwan Med Coll 10(1):54–57. https://doi.org/10.3126/jcmc.v10i1.28072
Monsomboon A, Patarateeranon T, Tongyoo S et al (2019) Agreement between emergency physicians and a cardiologist on cardiac function evaluation after short training. Siriraj Med J 71(4):253–260. https://doi.org/10.33192/Smj.2019.39
Wiegers SE, Ryan T, Arrighi JA et al (2019) 2019 ACC/AHA/ASE Advanced Training Statement on Echocardiography (revision of the 2003 ACC/AHA clinical competence Statement on Echocardiography): a report of the ACC competency Management Committee. J Am Coll Cardiol 74(3):377–402. https://doi.org/10.1016/j.jacc.2019.02.003
Lang RM, Badano LP, Victor MA et al (2015) Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr 28(1):1–39e14. https://doi.org/10.1016/j.echo.2014.10.003
Albaroudi B, Haddad M, Albaroudi O, Abdel-Rahman ME, Jarman R, Harris T (2022) Assessing left ventricular systolic function by emergency physician using point of care echocardiography compared to expert: systematic review and meta-analysis. Eur J Emerg Med 29(1):18–32. https://doi.org/10.1097/MEJ.0000000000000866
Le MPT, Voigt L, Nathanson R et al (2022) Comparison of four handheld point-of-care ultrasound devices by expert users. Ultrasound J 14(1). https://doi.org/10.1186/s13089-022-00274-6
Sağlam C, Ünlüer EE, Yamanoğlu NGÇ et al (2021) Accuracy of Emergency Physicians for detection of Regional Wall Motion Abnormalities in patients with chest Pain without ST-Elevation myocardial infarction. J Ultrasound Med 40(7):1335–1342. https://doi.org/10.1002/jum.15513
Shiina A, Tajik AJ, Smith HC, Lengyel M, Seward JB (1986) Prognostic significance of Regional Wall Motion abnormality in patients with prior myocardial infarction: a prospective correlative study of Two-Dimensional Echocardiography and Angiography. Mayo Clin Proc 61(4):254–262. https://doi.org/10.1016/S0025-6196(12)61925-9
Cicala S, de Simone G, Roman MJ et al (2007) Prevalence and prognostic significance of wall-motion abnormalities in adults without clinically recognized Cardiovascular Disease. Circulation 116(2):143–150. https://doi.org/10.1161/CIRCULATIONAHA.106.652149
Espersen C, Modin D, Platz E et al (2022) Global and regional wall motion abnormalities and incident heart failure in the general population. Int J Cardiol 357:146–151. https://doi.org/10.1016/j.ijcard.2022.03.027
Funding
This study did not receive a grant from any funding agency in the public, commercial, or non-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Andrea Teira Calderón and Jose Antonio Vázque de Prada Tiffe contributed to the conception and design of the study, the acquisition of data, the analysis and interpretation of data and the drafting of the article. Molly Levine; Cristina Ruisánchez Villar; David Serrano González; Santiago Catoya Villa; Miguel Llano Cardenal; Piedad Lerena Saenza; José María Cuesta Cosgaya; Mónica Fernández-Valls; Francisco González Vilchez; Jose María de la Torre Hernández; Héctor M. García-García contributed revising the manuscript critically for important intellectual content. All authors approved the version to be submitted.
Corresponding author
Ethics declarations
Conflicts of interest
The authors report no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Teira Calderón, A., Levine, M., Ruisánchez, C. et al. Clinical comparison of a handheld cardiac ultrasound device for the assessment of left ventricular function. Int J Cardiovasc Imaging 40, 55–64 (2024). https://doi.org/10.1007/s10554-023-02979-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-023-02979-8