Abstract
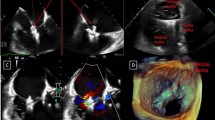
In the pediatric and congenital heart disease (CHD) population, tricuspid valve (TV) disorders are complex due to the variable TV morphology, its sophisticated interaction with the right ventricle as well as associated congenital and acquired lesions. While surgery is the standard of care for TV dysfunction in this patient population, transcatheter treatment for bioprosthetic TV dysfunction has been performed successfully. Detailed and accurate anatomic assessment of the abnormal TV is essential in the preoperative/preprocedural planning. Three-dimensional transthoracic and 3D transesophageal echocardiography (3DTEE) provides added value to 2-dimensional imaging in the characterization of the TV to guide therapy and 3DTEE serves as an excellent tool for intraoperative assessment and procedural guidance of transcatheter treatment. Notwithstanding advances in imaging and therapy, the timing and indication for intervention for TV disorders in this population are not well defined. In this manuscript, we aim to review the available literature, provide our institutional experience with 3DTEE, and briefly discuss the perceived challenges and future directions in the assessment, surgical planning, and procedural guidance of (1) congenital TV malformations, (2) acquired TV dysfunction from transvenous pacing leads, or following cardiac surgeries, and (3) bioprosthetic TV dysfunction.




Similar content being viewed by others
Abbreviations
- ACHD:
-
Adult congenital heart disease
- CHD:
-
Congenital heart disease
- RV:
-
Right ventricle
- TV:
-
Tricuspid valve
- TR:
-
Tricuspid regurgitation
- 3DTEE:
-
3-Dimensional transesophageal echocardiography
- 3DE:
-
3-Dimensional echocardiography
- 2DE:
-
2-Dimensional echocardiography
References
Hahn RT, Weckbach LT, Noack T et al (2021) Proposal for a standard echocardiographic tricuspid valve nomenclature. JACC Cardiovasc Imaging 14(7):1299–1305. https://doi.org/10.1016/j.jcmg.2021.01.012
Qureshi MY, Sommer RJ, Cabalka AK (2019) Tricuspid valve imaging and intervention in Pediatric and adult patients with congenital heart disease. JACC Cardiovasc Imaging 12(4):637–651. https://doi.org/10.1016/j.jcmg.2018.10.036
Alsaied T, Christopher AB, Da Silva J et al (2022) Multimodality imaging in Ebstein Anomaly. Pediatr Cardiol. https://doi.org/10.1007/s00246-022-03011-x
Karagodin I, Yamat M, Addetia K, Lang RM (2021) Visualization of number of tricuspid valve leaflets using three-dimensional transthoracic echocardiography. J Am Soc Echocardiogr 34(4):449–450. https://doi.org/10.1016/j.echo.2020.12.015
Tretter JT, Sarwark AE, Anderson RH, Spicer DE (2016) Assessment of the anatomical variation to be found in the normal tricuspid valve. Clin Anat 29(3):399–407. https://doi.org/10.1002/ca.22591
Wafae N, Hayashi H, Gerola LR, Vieira MC (1990) Anatomical study of the human tricuspid valve. Surg Radiol Anat 12(1):37–41. https://doi.org/10.1007/BF02094123
Hahn RT (2016) State-of-the-art review of echocardiographic imaging in the evaluation and treatment of functional tricuspid regurgitation. Circ Cardiovasc Imaging 9(12):1–15. https://doi.org/10.1161/CIRCIMAGING.116.005332
Cesna S, Eicken A (2021) Percutaneous techniques for treatment of tricuspid valve dysfunction in congenital heart disease–an emerging therapy. Expert Rev Cardiovasc Ther 19(9):817–824. https://doi.org/10.1080/14779072.2021.1865154
Simpson J, Lopez L, Acar P et al (2017) Three-dimensional echocardiography in congenital heart disease: an expert consensus document from the european association of cardiovascular imaging and the american society of echocardiography. J Am Soc Echocardiogr 30(1):1–27. https://doi.org/10.1016/j.echo.2016.08.022
Hahn RT, Saric M, Faletra FF et al (2022) Recommended standards for the performance of transesophageal echocardiographic screening for structural heart intervention: from the American Society of Echocardiography. J Am Soc Echocardiogr 35(1):1–76. https://doi.org/10.1016/j.echo.2021.07.006
Vegas A (2016) Three-dimensional transesophageal echocardiography: principles and clinical applications. Ann Card Anaesth 19(5):S35–S43. https://doi.org/10.4103/0971-9784.192622
Lang RM, Badano LP, Tsang W et al (2012) EAE/ASE recommendations for image acquisition and display using three-dimensional echocardiography. J Am Soc Echocardiogr 25(1):3–46. https://doi.org/10.1016/j.echo.2011.11.010
Jone PN (2020) Applications of three-dimensional transesophageal echocardiography in congenital heart disease. Echocardiography 37(10):1665–1672. https://doi.org/10.1111/echo.14780
Jone PN, Haak A, Ross M et al (2019) Congenital and structural heart disease interventions using echocardiography-fluoroscopy fusion imaging. J Am Soc Echocardiogr 32(12):1495–1504. https://doi.org/10.1016/j.echo.2019.07.023
Cai AW, Constantine A, Bartolacelli Y, Krieger EV (2022) Training to care for adults with congenital heart disease in the USA and Europe. Heart 108(18):1498–1499. https://doi.org/10.1136/heartjnl-2022-321156
Takahashi K, Mackie AS, Rebeyka IM et al (2010) Two-dimensional versus transthoracic real-time three-dimensional echocardiography in the evaluation of the mechanisms and sites of atrioventricular valve regurgitation in a congenital heart disease population. J Am Soc Echocardiogr 23(7):726–734. https://doi.org/10.1016/j.echo.2010.04.017
Abudiab MM, Chao CJ, Liu S, Naqvi TZ (2017) Quantitation of valve regurgitation severity by three-dimensional vena contracta area is superior to flow convergence method of quantitation on transesophageal echocardiography. Echocardiography 34(7):992–1001. https://doi.org/10.1111/echo.13549
Chen TE, Kwon SH, Enriquez-Sarano M, Wong BF, Mankad SV (2013) Three-dimensional color doppler echocardiographic quantification of tricuspid regurgitation orifice area: comparison with conventional two-dimensional measures. J Am Soc Echocardiogr 26(10):1143–1152. https://doi.org/10.1016/j.echo.2013.07.020
Mah K, Khoo NS, Tham E et al (2021) Tricuspid regurgitation in hypoplastic left heart syndrome: three-dimensional echocardiography provides additional information in describing jet location. J Am Soc Echocardiogr 34(5):529–536. https://doi.org/10.1016/j.echo.2020.12.010
Utsunomiya H, Harada Y, Susawa H et al (2019) Comprehensive evaluation of tricuspid regurgitation location and severity using vena contracta analysis: a color doppler three-dimensional transesophageal echocardiographic study. J Am Soc Echocardiogr 32(12):1526-1537e2. https://doi.org/10.1016/j.echo.2019.07.022
Li L, Colen TM, Jani V et al (2021) Dynamic systolic changes in tricuspid regurgitation vena contracta size and proximal isovelocity surface area in hypoplastic left heart syndrome: a three-dimensional color doppler echocardiographic study. J Am Soc Echocardiogr 34(8):877–886. https://doi.org/10.1016/j.echo.2021.03.004
Kutty S, Colen T, Thompson RB et al (2014) Tricuspid regurgitation in hypoplastic left heart syndrome mechanistic insights from 3-dimensional echocardiography and relationship with outcomes. Circ Cardiovasc Imaging 7(5):765–772. https://doi.org/10.1161/CIRCIMAGING.113.001161
Colen T, Kutty S, Thompson RB et al (2018) Tricuspid valve adaptation during the first interstage period in hypoplastic left heart syndrome. J Am Soc Echocardiogr 31(5):624–633. https://doi.org/10.1016/j.echo.2017.11.020
Nguyen AV, Lasso A, Nam HH et al (2019) Dynamic three-dimensional geometry of the tricuspid valve annulus in hypoplastic left heart syndrome with a fontan circulation. J Am Soc Echocardiogr 32(5):655-666e13. https://doi.org/10.1016/j.echo.2019.01.002
O’Leary PW, Dearani JA, Anderson RH, Spicer DE, Srivastava D (2019) Diseases of the tricuspid valve. In: Wernovsky G, Anderson RH, Kumar K et al (eds) Anderson’s Pediatric Cardiology, 4th edn. Elsevier Ltd, Amsterdam, pp 585–605
Kouchoukos NT, Blackstone EH, Hanley FL, Kirklin JK (2012) Tricuspid valve disease. In: Kouchoukos NT, Blackstone EH, Hanley FL, Kirklin JK (eds) Kirklin/Barratt-Boyes cardiac surgery, 4th edn. Elsevier Saunders, Philadelphia, pp 656–671
Barron DJ, Stumper O, Brawn WJ, Spicer DE, Anderson RH (2022) Chapter 38 - congenitally corrected transposition. In: Anderson’s Pediatric Cardiology. Fourth Edition Elsevier Ltd. pp. 697–714 https://doi.org/10.1016/B978-0-7020-7608-4.00044-3
Cetta F, Dearani JA, O’Leary PW, Driscoll DJ (2016) Ebstein Anomaly. In: Alen HD (ed) Moss and Adams’ heart disease in infants, children, and adolescents, including the fetus and young adult. Wolters Kluwer Health, London, pp 288–294
Cetta F, Eidem BW (2016) Chapter 13. Ebstein Anomaly, tricuspid valve dysplasia, and right atrial anomalies. In: Lai WW, Mertens L, Cohen S, Geva M (eds) Echocardiography in pediatric and congenital heart disease: from fetus to adult, 2nd edn. Wiley, Hoboken, pp 231–242
Vettukattil JJ, Bharucha T, Anderson RH (2007) Defining Ebstein’s malformation using three-dimensional echocardiography. Interact Cardiovasc Thorac Surg 6(6):685–690. https://doi.org/10.1510/icvts.2007.156612
Bharucha T, Anderson RH, Lim ZS, Vettukattil JJ (2010) Multiplanar review of three-dimensional echocardiography gives new insights into the morphology of Ebsteins malformation. Cardiol Young 20(1):49–53. https://doi.org/10.1017/S1047951109991971
Pacifico AD (2003) Transesophageal three-dimensional echocardiographic demonstration of Ebstein ’ s Anomaly. Echocardiography 20(2):305–307
Acar P, Abadir S, Roux D et al (2006) Ebstein’s anomaly assessed by real-time 3-D echocardiography. Ann Thorac Surg 82(2):731–733. https://doi.org/10.1016/j.athoracsur.2005.09.012
van Noord PT, Scohy TV, McGhie J, Bogers AJJC (2010) Three-dimensional transesophageal echocardiography in Ebstein’s anomaly. Interact Cardiovasc Thorac Surg 10(5):836–837. https://doi.org/10.1510/icvts.2009.229476
Pigula FA, Mettler B (2017) Management of tricuspid regurgitation in patients with hypoplastic left heart syndrome. Semin Thorac Cardiovasc Surg 29(1):64–69. https://doi.org/10.1053/j.semtcvs.2017.02.004
Ono M, Mayr B, Burri M et al (2020) Tricuspid valve repair in children with hypoplastic left heart syndrome: impact of timing and mechanism on outcome. Eur J Cardio-thoracic Surg 57(6):1083–1090. https://doi.org/10.1093/ejcts/ezaa004
Mah K, Khoo NS, Martin BJ et al (2022) Insights from 3D Echocardiography in Hypoplastic Left Heart Syndrome Patients undergoing TV repair. Pediatr Cardiol 43(4):735–743. https://doi.org/10.1007/s00246-021-02780-1
Shigemitsu S, Mah K, Thompson RB et al (2021) Tricuspid valve tethering is Associated with residual regurgitation after Valve Repair in Hypoplastic Left Heart Syndrome: A three-dimensional echocardiographic study. J Am Soc Echocardiogr 34(11):1199–1210. https://doi.org/10.1016/j.echo.2021.06.007
Herz C, Pace DF, Nam HH et al (2021) Segmentation of tricuspid valve leaflets from transthoracic 3D echocardiograms of children with hypoplastic Left Heart Syndrome using deep learning. Front Cardiovasc Med 8(December):1–19. https://doi.org/10.3389/fcvm.2021.735587
Pouch AM, Aly AH, Lasso A et al (2017) Image segmentation and modeling of the Pediatric Tricuspid Valve in Hypoplastic Left Heart Syndrome. Funct imaging Model Hear Int Work FIMH proceedings FIMH 10263(1):95–105. https://doi.org/10.1007/978-3-319-59448-4_10
Carozza A, Renzulli A, De Feo M et al (2001) Tricuspid repair for infective endocarditis: clinical and echocardiographic results. Tex Hear Inst J 28(2):96–101
Dawood MY, Cheema FH, Ghoreishi M et al (2015) Contemporary outcomes of operations for tricuspid valve infective endocarditis. Ann Thorac Surg 99(2):539–546. https://doi.org/10.1016/j.athoracsur.2014.08.069
Yousof AM, Shafei MZ, Endrys G, Khan N, Simo M, Cherian G (1985) Tricuspid stenosis and regurgitation in rheumatic heart disease: a prospective cardiac catheterization study in 525 patients. Am Heart J 110(1 PART 1):60–64. https://doi.org/10.1016/0002-8703(85)90515-0
Lewis MJ, Ginns JN, Ye S et al (2016) Postoperative tricuspid regurgitation after adult congenital heart surgery is associated with adverse clinical outcomes. J Thorac Cardiovasc Surg 151(2):460–465. https://doi.org/10.1016/j.jtcvs.2015.09.028
Messika-Zeitoun D, Thomson H, Bellamy M et al (2004) Medical and surgical outcome of tricuspid regurgitation caused by flail leaflets. J Thorac Cardiovasc Surg 128(2):296–302. https://doi.org/10.1016/j.jtcvs.2004.01.035
Huang Y, Dearani JA, Lahr BD et al (2022) Surgical management of transvenous lead-induced tricuspid regurgitation in adult and pediatric patients with congenital heart disease. J Thorac Cardiovasc Surg 163(6):2185–2193e4. https://doi.org/10.1016/j.jtcvs.2021.10.006
Taira K, Suzuki A, Fujino A, Watanabe T, Ogyu A, Ashikawa K (2006) Tricuspid valve stenosis related to subvalvular adhesion of pacemaker lead: a case report. J Cardiol 47(6):301–306. http://www.ncbi.nlm.nih.gov/pubmed/16800373
Gelves-Meza J, Lang RM, Valderrama-Achury MD et al (2022) Tricuspid regurgitation related to cardiac implantable electronic devices: an integrative review. J Am Soc Echocardiogr. https://doi.org/10.1016/j.echo.2022.08.004
Fukuda S, Saracino G, Matsumura Y et al (2006) Three-dimensional geometry of the tricuspid annulus in healthy subjects and in patients with functional tricuspid regurgitation: a real-time, 3-dimensional echocardiographic study. Circulation 114(SUPPL 1):492–498. https://doi.org/10.1161/CIRCULATIONAHA.105.000257
Puchalski MD, Lui GK, Miller-Hance WC et al (2019) Guidelines for performing a comprehensive transesophageal echocardiographic: examination in children and all patients with congenital heart disease: recommendations from the American Society of Echocardiography. J Am Soc Echocardiogr 32(2):173–215. https://doi.org/10.1016/j.echo.2018.08.016
Tei C, Pilgrim JP, Shah PM, Ormiston JA, Wong M (1982) The tricuspid valve annulus: study of size and motion in normal subjects and in patients with tricuspid regurgitation. Circulation 66(3):665–671. https://doi.org/10.1161/01.cir.66.3.665
Friedberg MK (2018) Imaging right-left ventricular interactions. JACC Cardiovasc Imaging 11(5):755–771. https://doi.org/10.1016/j.jcmg.2018.01.028
Volpato V, Badano LP, Figliozzi S, Florescu DR, Parati G, Muraru D (2021) Multimodality cardiac imaging and new display options to broaden our understanding of the tricuspid valve. Curr Opin Cardiol 36(5):513–524. https://doi.org/10.1097/HCO.0000000000000890
Karhausen J, Dudaryk R, Phillips-Bute B et al (2012) Three-dimensional transesophageal echocardiography for perioperative right ventricular assessment. Ann Thorac Surg 94(2):468–474. https://doi.org/10.1016/j.athoracsur.2012.03.073
Kawase T, Takahashi Y, Ito A et al (2022) Three-dimensional transesophageal echocardiographic morphological evaluation of the tricuspid valve. Interact Cardiovasc Thorac Surg. https://doi.org/10.1093/icvts/ivac145
Magunia H, Schmid E, Hilberath JN et al (2017) 2D echocardiographic evaluation of right ventricular function correlates with 3D volumetric models in cardiac surgery patients. J Cardiothorac Vasc Anesth 31(2):595–601. https://doi.org/10.1053/j.jvca.2016.11.020
Stephens EH, Dearani JA, Qureshi MY, Ammash N, Maleszewski JJ (2020) The congenital tricuspid valve spectrum: from Ebstein to Dysplasia. World J Pediatr Congenit Hear Surg 11(6):783–791. https://doi.org/10.1177/2150135120949235
Hahn RT (2022) The right heart and outcomes of tricuspid valve surgery. Eur J Cardiothorac Surg 62(2):7–8. https://doi.org/10.1093/ejcts/ezac352
Bharucha T, Honjo O, Seller N et al (2013) Mechanisms of tricuspid valve regurgitation in hypoplastic left heart syndrome: a case-matched echocardiographic-surgical comparison study. Eur Heart J Cardiovasc Imaging 14(2):135–141. https://doi.org/10.1093/ehjci/jes123
Garatti A, Nano G, Bruschi G et al (2012) Twenty-five year outcomes of tricuspid valve replacement comparing mechanical and biologic prostheses. Ann Thorac Surg 93(4):1146–1153. https://doi.org/10.1016/j.athoracsur.2011.12.031
Guenther T, Noebauer C, Mazzitelli D, Busch R, Tassani-Prell P, Lange R (2008) Tricuspid valve surgery: a thirty-year assessment of early and late outcome. Eur J Cardio-thoracic Surg 34(2):402–409. https://doi.org/10.1016/j.ejcts.2008.05.006
McElhinney DB, Cabalka AK, Aboulhosn JA et al (2016) Transcatheter tricuspid valve-in-valve implantation for the treatment of dysfunctional surgical bioprosthetic valves: an international, multicenter registry study. Circulation 133(16):1582–1593. https://doi.org/10.1161/CIRCULATIONAHA.115.019353
Zaidi A, Oxborough D, Augustine DX et al (2020) Echocardiographic assessment of the tricuspid and pulmonary valves: a practical guideline from the british Society of Echocardiography. Echo Res Pract 7(4):G95–G122. https://doi.org/10.1530/ERP-20-0033
Vahanian A, Beyersdorf F, Praz F et al (2022) 2021 ESC/EACTS guidelines for the management of valvular heart disease: developed by the task force for the management of valvular heart disease of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic surgery (EACTS). Rev Esp Cardiol (Engl Ed) 75(6):524. https://doi.org/10.1016/j.rec.2022.05.006
Friedberg MK, Reddy S (2019) Right ventricular failure in congenital heart disease. Curr Opin Pediatr 31(5):604–610. https://doi.org/10.1097/MOP.0000000000000804
Reddy S, Bernstein D (2015) The vulnerable right ventricle. Curr Opin Pediatr 27(5):563–568. https://doi.org/10.1097/MOP.0000000000000268
Tamborini G, Marsan NA, Gripari P et al (2010) Reference values for right ventricular volumes and ejection Fraction with Real-Time Three-Dimensional Echocardiography: evaluation in a large series of normal subjects. J Am Soc Echocardiogr 23(2):109–115. https://doi.org/10.1016/j.echo.2009.11.026
Wejner PM, Kasprzak JD, Szymczyk E et al (2022) Changes in right ventricular morphology and function in patients undergoing cardiac surgery: a 3D echocardiographic study. Kardiol Pol 80(2):156–162. https://doi.org/10.33963/KP.a2021.0195
Fusini L, Tamborini G, Gripari P et al (2011) Feasibility of intraoperative three-dimensional transesophageal echocardiography in the evaluation of right ventricular volumes and function in patients undergoing cardiac surgery. J Am Soc Echocardiogr 24(8):868–877. https://doi.org/10.1016/j.echo.2011.05.002
Grewal J, Majdalany D, Syed I, Pellikka P, Warnes CA (2010) Three-dimensional echocardiographic assessment of right ventricular volume and function in adult patients with congenital heart disease: comparison with magnetic resonance imaging. J Am Soc Echocardiogr 23(2):127–133. https://doi.org/10.1016/j.echo.2009.11.002
Jone PN, Le L, Pan Z et al (2022) Three-Dimensional Echocardiography right ventricular volumes and ejection fraction reference values in children: a north american Multicentre Study. Can J Cardiol 38(9):1426–1433. https://doi.org/10.1016/j.cjca.2022.04.026
Morcos M, Kilner PJ, Sahn DJ, Litt HI, Valsangiacomo-Buechel ER, Sheehan FH (2017) Comparison of systemic right ventricular function in transposition of the great arteries after atrial switch and congenitally corrected transposition of the great arteries. Int J Cardiovasc Imaging 33(12):1993–2001. https://doi.org/10.1007/s10554-017-1201-4
Herberg U, Smit F, Winkler C, Dalla-Pozza R, Breuer J, Laser KT (2021) Real-time 3D-echocardiography of the right ventricle-paediatric reference values for right ventricular volumes using knowledge-based reconstruction: a multicentre study. Quant Imaging Med Surg 11(7):2905–2917. https://doi.org/10.21037/qims-20-1155
Renella P, Marx GR, Zhou J, Gauvreau K, Geva T (2014) Feasibility and reproducibility of three-dimensional echocardiographic assessment of right ventricular size and function in pediatric patients. J Am Soc Echocardiogr 27(8):903–910. https://doi.org/10.1016/j.echo.2014.04.008
Zhao R, Shu F, Zhang C et al (2020) Early detection and prediction of Anthracycline-induced right ventricular cardiotoxicity by 3-dimensional echocardiography. JACC CardioOncol 2(1):13–22. https://doi.org/10.1016/j.jaccao.2020.01.007
D’Andrea A, Riegler L, Morra S et al (2012) Right ventricular morphology and function in top-level athletes: a three-dimensional echocardiographic study. J Am Soc Echocardiogr 25(12):1268–1276. https://doi.org/10.1016/j.echo.2012.07.020
Kjaergaard J, Petersen CL, Kjaer A, Schaadt BK, Oh JK, Hassager C (2006) Evaluation of right ventricular volume and function by 2D and 3D echocardiography compared to MRI. Eur J Echocardiogr 7(6):430–438. https://doi.org/10.1016/j.euje.2005.10.009
Bera D, Raghunathan SB, Chen C et al (2018) Multiline 3D beamforming using micro-beamformed datasets for pediatric transesophageal echocardiography. Phys Med Biol 63(7):075015. https://doi.org/10.1088/1361-6560/aab45e
Morgan AE, Howell K, Chen S et al (2020) Imaging and computational modeling of tricuspid regurgitation and repair. Vessel Plus 4:1–14. https://doi.org/10.20517/2574-1209.2019.32
Acknowledgements
The authors appreciate Ms. Kaitlin Doan for her assistance in editing the videos.
Funding
The authors have not disclosed any funding.
Author information
Authors and Affiliations
Contributions
TD: wrote the main manuscript text and prepared figures and videos. All authors reviewed, edited, and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file1 Video 1. TV dysplasia with tethered septal leaflet (S) and significantly reduced motion of the leaflet edge which led to a coaptation defect with the anterior (A) and posterior leaflet (P). Patient had a successful repair with mild regurgitation and no stenosis (MP4 30673 kb)
Supplementary file2 Video 2. Ebstein anomaly with severe apical displacement of the septal leaflet and restricted motion of all 3 leaflets resulting in a large coaptation defect. The TV orifice is seen opening into the RV outflow tract. Patient had a TV replacement due to high risk condition and severely limited leaflet mobility (MP4 24397 kb)
Supplementary file3 Video 3. Ebstein anomaly with moderate apical displacement of the septal leaflet. There are 2 large anterior leaflets and good mobility of all 3 leaflets. The effective orifice is seen opening into the RV outflow tract. The patient underwent a successful Cone reconstruction of the TV (MP4 24395 kb)
Supplementary file4 Video 4. Severe TR in a patient with history of hypoplastic left heart syndrome and Fontan circulation. The anterior and posterior leaflets are fused with significant prolapse while the septal leaflet is tethered with restricted mobility, resulting in a large coaptation defect and severe TR via an eccentric jet (MP4 15866 kb)
Supplementary file5 Video 5. Transvenous dual chamber pacemaker with atrial lead curling at the TV inflow disrupting closure of the leaflets and ventricular lead crossing the TV along the septal leaflet (MP4 23724 kb)
Supplementary file6 Video 6. Ventricular pacemaker lead crossing near the posterior leaflet with significant restriction of posterior and septal leaflet resulting in a large coaptation defect (MP4 18733 kb)
Supplementary file7 Video 7. Persistent severe TR from tethered septal and posterior leaflets and densely thickened chord resulting in a very large coaptation defect (following a transvenous defibrillator lead removal) (MP4 24470 kb)
Supplementary file8 Video 8. Patient with single RV, Fontan circulation, and mechanical St Jude valve in the TV position presenting with recurrent stroke. There are significant artifacts on 2DE. The 2 discs are with normal mobility on 3DTEE, and no obvious clots noted on the valve (MP4 4028 kb)
Supplementary file9 Video 9. Konno patch dehiscence resulting in severely restricted septal leaflet, a large coaptation defect and severe regurgitation along the septal leaflet (MP4 25059 kb)
Supplementary file10 Video 10. Procedural guidance using 3DTEE during an off-label, transcatheter valve-in-valve treatment using a 29-mm Edwards valve for severe, symptomatic TR 4 years after surgical replacement of a 33-mm Epic porcine valve (MP4 95650 kb)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Doan, T.T., Pignatelli, R.H., Parekh, D.R. et al. Imaging and guiding intervention for tricuspid valve disorders using 3-dimensional transesophageal echocardiography in pediatric and congenital heart disease. Int J Cardiovasc Imaging 39, 1855–1864 (2023). https://doi.org/10.1007/s10554-023-02898-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-023-02898-8