Abstract
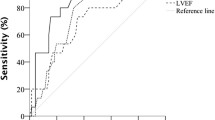
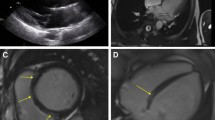
Etiology of sudden cardiac arrest (SCA) is identified in less than 30% of survivors without coronary artery disease. We sought to assess the diagnostic role of myocardial parametric mapping using cardiovascular magnetic resonance (CMR) in identifying SCA etiology. Consecutive SCA survivors undergoing CMR with myocardial parametric mapping were included in the study. The determination if CMR was decisive or contributory in identifying SCA etiology was made if the diagnosis was unclear prior to CMR, and the discharge diagnosis was consistent with the CMR result. Parametric mapping was considered essential for establishing probable SCA etiology by CMR if the SCA cause could not have been determined without its utilization. If the CMR diagnosis could have been potentially based on the combination of cine and LGE imaging, parametric mapping was considered contributory. Of the 35 patients (mean age 46.9 ± 14.1 years; 57% males) included, SCA diagnosis was based on CMR in 23 (66%) patients. Of those, parametric mapping was essential for the diagnosis of myocarditis and tako-tsubo cardiomyopathy (11/48%) and contributed to the diagnosis in 10 (43%) additional cases. Inclusion of quantitative T1 and T2 parametric mapping in the SCA CMR protocol has the potential to increase diagnostic yield of CMR and further specify SCA etiology, especially myocarditis.


Similar content being viewed by others
References
Carter-Monroe N, Virmani R (2011) Current trends in the classification of sudden cardiac death based on autopsy derived data: a review of investigations into the etiology of sudden cardiac death. Revista Española de Cardiología (English Edition) 64(1):10–12. https://doi.org/10.1016/j.recesp.2010.09.004
Zareba W, Zareba KM (2017) Cardiac magnetic resonance in sudden cardiac arrest survivors. Circ Cardiovasc Imaging. https://doi.org/10.1161/CIRCIMAGING.117.007290
Zorzi A, Susana A, de Lazzari M, Migliore F, Vescovo G, Scarpa D et al (2018) Diagnostic value and prognostic implications of early cardiac magnetic resonance in survivors of out-of-hospital cardiac arrest. Heart Rhythm 15(7):1031–1041. https://doi.org/10.1016/j.hrthm.2018.02.033
Ojrzyńska-Witek N, Marczak M, Mazurkiewicz Ł, Petryka-Mazurkiewicz J, Miłosz-Wieczorek B, Grzybowski J et al (2022) Sudden cardiac arrest: focus on cardiac magnetic resonance. Kardiol Pol 80(1):87–89. https://doi.org/10.33963/KP.a2021.0151
Zaremba T, Brøndberg AK, Jensen HK, Kim WY (2018) Cardiac magnetic resonance characteristics in young survivors of aborted sudden cardiac death. Eur J Radiol 105:141–147. https://doi.org/10.1016/j.ejrad.2018.06.004
Swoboda P, Kidambi A, Uddin A, McDiarmid A, Ripley D, Greenwood J et al (2014) Cardiovascular magnetic resonance is valuable in the investigation of aborted sudden cardiac death. Heart 100(Suppl 3):A71.2-A72. https://doi.org/10.1136/heartjnl-2014-306118.125
Rodrigues P, Joshi A, Williams H, Westwood M, Petersen SE, Zemrak F et al (2017) Diagnosis and prognosis in sudden cardiac arrest survivors without coronary artery disease: utility of a clinical approach using cardiac magnetic resonance imaging. Circ Cardiovasc Imaging 10(12):e006709. https://doi.org/10.1161/CIRCIMAGING.117.006709
O’Brien AT, Gil KE, Varghese J, Simonetti OP, Zareba KM (2022) T2 mapping in myocardial disease: a comprehensive review. J Cardiovasc Magn Reson 24:33. https://doi.org/10.1186/s12968-022-00866-0
Giri S, Chung YC, Merchant A, Mihai G, Rajagopalan S, Raman Sv et al (2009) T2 quantification for improved detection of myocardial edema. J Cardiovasc Magn Reson 11(1):56. https://doi.org/10.1186/1532-429X-11-56
Wong TC, Piehler KM, Kang IA, Kadakkal A, Kellman P, Schwartzman DS et al (2014) Myocardial extracellular volume fraction quantified by cardiovascular magnetic resonance is increased in diabetes and associated with mortality and incident heart failure admission. Eur Heart J 35(10):657–664. https://doi.org/10.1093/eurheartj/eht193
Schelbert EB, Piehler KM, Zareba KM, Moon JC, Ugander M, Messroghli DR et al (2015) Myocardial fibrosis quantified by extracellular volume is associated with subsequent hospitalization for heart failure, death, or both across the spectrum of ejection fraction and heart failure stage. J Am Heart Assoc. https://doi.org/10.1161/JAHA.115.002613
Cheng RK, Masri SC (2019) Extracellular volume as an imaging biomarker for incident heart failure. Circ Cardiovasc Imaging 12(12):10152. https://doi.org/10.1161/CIRCIMAGING.119.010152
Laohabut I, Songsangjinda T, Kaolawanich Y, Yindeengam A, Krittayaphong R (2021) Myocardial extracellular volume fraction and T1 mapping by cardiac magnetic resonance compared between patients with and without type 2 diabetes, and the effect of ECV and T2D on cardiovascular outcomes. Front Cardiovasc Med 7:1725. https://doi.org/10.3389/fcvm.2021.771363
Youn JC, Hong YJ, Lee HJ, Han K, Shim CY, Hong GR et al (2017) Contrast-enhanced T1 mapping-based extracellular volume fraction independently predicts clinical outcome in patients with non-ischemic dilated cardiomyopathy: a prospective cohort study. Eur Radiol 27(9):3924–3933. https://doi.org/10.1007/s00330-017-4817-9
Schelbert EB, Fridman Y, Wong TC, Abu Daya H, Piehler KM, Kadakkal A et al (2017) Temporal relation between myocardial fibrosis and heart failure with preserved ejection fraction: association with baseline disease severity and subsequent outcome. JAMA Cardiol 2(9):995–1006. https://doi.org/10.1001/jamacardio.2017.2511
Kramer CM, Barkhausen J, Bucciarelli-Ducci C, Flamm SD, Kim RJ, Nagel E (2020) Standardized cardiovascular magnetic resonance imaging (CMR) protocols: 2020 update. J Cardiovasc Magn 22(1):1–18. https://doi.org/10.1186/s12968-020-00607-1
Haaf P, Garg P, Messroghli DR, Broadbent DA, Greenwood JP, Plein S (2016) Cardiac T1 mapping and extracellular volume (ECV) in clinical practice: a comprehensive review. J Cardiovasc Magn Reson 18(1):1–12. https://doi.org/10.1186/s12968-016-0308-4
Cerqueira MD, Weissman NJ, Dilsizian V, Jacobs AK, Kaul S, Laskey WK et al (2002) Standardized myocardial segmentation and nomenclature for tomographic imaging of the heart. Circulation 105(4):539–542. https://doi.org/10.1161/hc0402.102975
Aquaro GD, Perfetti M, Camastra G, Monti L, Dellegrottaglie S, Moro C et al (2017) Cardiac MR with late gadolinium enhancement in acute myocarditis with preserved systolic function: ITAMY study. J Am Coll 70(16):1977–1987. https://doi.org/10.1016/j.jacc.2017.08.044
Maron BJ, Maron MS (2016) LGE means better selection of HCM patients for primary prevention implantable defibrillators. JACC: Cardiovasc Imaging 9(12):1403–1406. https://doi.org/10.1016/j.jcmg.2016.01.032
Bozkurt B, Colvin M, Cook J, Cooper LT, Deswal A, Fonarow GC et al (2016) Current diagnostic and treatment strategies for specific dilated cardiomyopathies: a scientific statement from the American Heart Association. Circulation 134:e579–e646. https://doi.org/10.1161/CIR.0000000000000455
Maron BJ, Towbin JA, Thiene G, Antzelevitch C, Corrado D, Arnett D et al (2006) Contemporary definitions and classification of the cardiomyopathies: an American Heart Association Scientific statement from the council on clinical cardiology, heart failure and transplantation committee; quality of care and outcomes research and functional genomics and translational biology interdisciplinary working groups; and council on epidemiology and prevention. Circulation 113(14):1807–1816. https://doi.org/10.1161/CIRCULATIONAHA.106.174287
Singh T, Khan H, Gamble DT, Scally C, Newby DE, Dawson D (2022) Takotsubo syndrome: pathophysiology, emerging concepts, and clinical implications. Circulation 145(13):1002–1019. https://doi.org/10.1161/CIRCULATIONAHA.121.055854
Thavendiranathan P, Walls M, Giri S, Verhaert D, Rajagopalan S, Moore S et al (2012) Improved detection of myocardial involvement in acute inflammatory cardiomyopathies using T2 mapping. Circ Cardiovasc Imaging 5(1):102–110. https://doi.org/10.1161/CIRCIMAGING.111.967836
Wu KC (2017) Sudden cardiac death substrate imaged by magnetic resonance imaging: from investigational tool to clinical applications. Circ Cardiovasc Imaging 10(7):e005461. https://doi.org/10.1161/CIRCIMAGING.116.005461
Baritussio A, Zorzi A, Ghosh Dastidar A, Susana A, Mattesi G, Rodrigues JCL et al (2017) Out of hospital cardiac arrest survivors with inconclusive coronary angiogram: impact of cardiovascular magnetic resonance on clinical management and decision-making. Resuscitation 116:91–97. https://doi.org/10.1016/j.resuscitation.2017.03.039
Tschöpe C, Ammirati E, Bozkurt B, Caforio ALP, Cooper LT, Felix SB et al (2021) Myocarditis and inflammatory cardiomyopathy: current evidence and future directions. Nat Rev Cardiol 18(3):169–193. https://doi.org/10.1038/s41569-020-00435-x
von Knobelsdorff-Brenkenhoff F, Schüler J, Dogangüzel S, Dieringer MA, Rudolph A, Greiser A et al (2017) Detection and monitoring of acute myocarditis applying quantitative cardiovascular magnetic resonance. Circ Cardiovasc Imaging 10(2):1–10. https://doi.org/10.1161/CIRCIMAGING.116.005242
Grun S, Schumm J, Greulich S, Wagner A, Schneider S, Bruder O et al (2012) Long-term follow-up of biopsy-proven viral myocarditis: predictors of mortality and incomplete recovery. J Am Coll Cardiol 59(18):1604–1615. https://doi.org/10.1016/j.jacc.2012.01.007
Spieker M, Katsianos E, Gastl M, Behm P, Horn P, Jacoby C et al (2018) T2 mapping cardiovascular magnetic resonance identifies the presence of myocardial inflammation in patients with dilated cardiomyopathy as compared to endomyocardial biopsy. Eur Heart J Cardiovasc Imaging 19(5):574–582. https://doi.org/10.1093/ehjci/jex230
Løgstrup BB, Nielsen JM, Kim WY, Poulsen SH (2016) Myocardial oedema in acutemyocarditis detected by echocardiographic 2Dmyocardial deformation analysis. Eur Heart J Cardiovasc Imaging 17(9):1018–1026. https://doi.org/10.1093/ehjci/jev302
Ruppert V, Meyer T, Pankuweit S, Möller E, Funck RC, Grimm W et al (2008) Gene expression profiling from endomyocardial biopsy tissue allows distinction between subentities of dilated cardiomyopathy. J Thorac Cardiovasc Surg 136(2):360-369.e1. https://doi.org/10.1016/j.jtcvs.2008.03.016
Ammirati E, Frigerio M, Adler ED, Basso C, Birnie DH, Brambatti M et al (2020) Management of acute myocarditis and chronic inflammatory cardiomyopathy: an expert consensus document. Circ Heart Fail 13(11):e007405. https://doi.org/10.1161/CIRCHEARTFAILURE.120.007405
Spieker M, Haberkorn S, Gastl M, Behm P, Katsianos S, Horn P et al (2017) Abnormal T2 mapping cardiovascular magnetic resonance correlates with adverse clinical outcome in patients with suspected acute myocarditis. J Cardiovasc Magn Reson 19(1):38. https://doi.org/10.1186/s12968-017-0350-x
Caforio ALP, Pankuweit S, Arbustini E, Basso C, Gimeno-Blanes J, Felix SB et al (2013) Current state of knowledge on aetiology, diagnosis, management, and therapy of myocarditis: a position statement of the European Society of Cardiology Working Group on myocardial and pericardial diseases. Eur Heart J 34(33):2636–2648. https://doi.org/10.1093/eurheartj/eht210
Dass S, Suttie JJ, Piechnik SK, Ferreira VM, Holloway CJ, Banerjee R et al (2012) Myocardial tissue characterization using magnetic resonance noncontrast T1 mapping in hypertrophic and dilated cardiomyopathy. Circ Cardiovasc Imaging 5(6):726–733. https://doi.org/10.1161/CIRCIMAGING.112.976738
Ferreira VM, Schulz-Menger J, Holmvang G, Kramer CM, Carbone I, Sechtem U et al (2018) Cardiovascular magnetic resonance in nonischemic myocardial inflammation: expert recommendations. J Am Coll Cardiol 72(24):3158–3176. https://doi.org/10.1016/j.jacc.2018.09.072
Rodrigues P, Joshi A, Williams H, Westwood M, Petersen SE, Zemrak F et al (2017) Diagnosis and prognosis in sudden cardiac arrest survivors without coronary artery disease: utility of a clinical approach using cardiac magnetic resonance imaging. Circ Cardiovasc Imaging 10(12):006709. https://doi.org/10.1161/CIRCIMAGING.117.006709
Baig M, Galazka P, Dakwar O, Syed SA, Sawlani R, Shahir K et al (2021) Prevalence of myocardial edema with T2 mapping in hypertrophic cardiomyopathy. J Am Coll Cardiol 77:1303. https://doi.org/10.1016/S0735-1097(21)02661-9
Bönner F, Spieker M, Haberkorn S, Jacoby C, Flögel U, Schnackenburg B et al (2016) Myocardial T2 mapping increases noninvasive diagnostic accuracy for biopsy-proven myocarditis. JACC: Cardiovasc Imaging 9:1467–1469. https://doi.org/10.1016/j.jcmg.2015.11.014
Lurz P, Luecke C, Eitel I, Föhrenbach F, Frank C, Grothoff M et al (2016) Comprehensive cardiac magnetic resonance imaging in patients with suspected myocarditis the myoracer-trial. J Am Coll Cardiol 67(15):1800–1811. https://doi.org/10.1016/j.jacc.2016.02.013
Funding
The authors have not disclosed any funding.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by KEG, VTT, KMZ and SR. The first draft of the manuscript was written by KEG and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gil, K.E., Truong, V.T., Zareba, K.M. et al. Parametric mapping by cardiovascular magnetic resonance imaging in sudden cardiac arrest survivors. Int J Cardiovasc Imaging 39, 1547–1555 (2023). https://doi.org/10.1007/s10554-023-02864-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-023-02864-4