Abstract
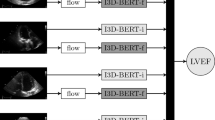
We sought to determine the cardiac ultrasound view of greatest quality using a machine learning (ML) approach on a cohort of transthoracic echocardiograms (TTE) with abnormal left ventricular (LV) systolic function. We utilize an ML model to determine the TTE view of highest quality when scanned by sonographers. A random sample of TTEs with reported LV dysfunction from 09/25/2017-01/15/2019 were downloaded from the regional database. Component video files were analyzed using ML models that jointly classified view and image quality. The model consisted of convolutional layers for extracting spatial features and Long Short-term Memory units to temporally aggregate the frame-wise spatial embeddings. We report the view-specific quality scores for each TTE. Pair-wise comparisons amongst views were performed with Wilcoxon signed-rank test. Of 1,145 TTEs analyzed by the ML model, 74.5% were from males and mean LV ejection fraction was 43.1 ± 9.9%. Maximum quality score was best for the apical 4 chamber (AP4) view (70.6 ± 13.9%, p<0.001 compared to all other views) and worst for the apical 2 chamber (AP2) view (60.4 ± 15.4%, p<0.001 for all views except parasternal short-axis view at mitral/papillary muscle level, PSAX M/PM). In TTEs scanned by professional sonographers, the view with greatest ML-derived quality was the AP4 view.




Similar content being viewed by others
Availability of data and material
The data that support the findings of this study are available on request from the corresponding author, CL. The data is available subject to approval by the University of British Columbia Clinical Research Ethics Board.
Abbreviations
- AP2:
-
apical 2 chamber view
- AP3:
-
apical 3 chamber view
- AP4:
-
apical 4 chamber view
- CPACS:
-
Cardiology Picture Archiving and Communications System
- LSTM:
-
long short-term memory model
- PLAX:
-
parasternal long-axis view
- PSAX M/PM:
-
parasternal short-axis view at the level of the mitral valve or papillary muscle
- POCUS:
-
point of care ultrasound
- RWMA:
-
regional wall motion abnormality
- TTE:
-
transthoracic echocardiogram
References
Johri AM, Durbin J, Newbigging J, Tanzola R, Chow R, De S, Tam J (2018) Committee CSoECPoCU: Cardiac Point-of-care Ultrasound: state of the art in Medical School Education.J Am Soc Echocardiogr
Haskins SC, Bronshteyn Y, Perlas A, El-Boghdadly K, Zimmerman J, Silva M, Boretsky K, Chan V, Kruisselbrink R, Byrne M et al (2021) : American Society of Regional Anesthesia and Pain Medicine expert panel recommendations on point-of-care ultrasound education and training for regional anesthesiologists and pain physicians-part I: clinical indications.Reg Anesth Pain Med
Haskins SC, Bronshteyn Y, Perlas A, El-Boghdadly K, Zimmerman J, Silva M, Boretsky K, Chan V, Kruisselbrink R, Byrne M et al American Society of Regional Anesthesia and Pain Medicine expert panel recommendations on point-of-care ultrasound education and training for regional anesthesiologists and pain physicians—part II: recommendations.Regional Anesthesia & Pain Medicine2021:rapm-2021-10256
Lambrecht JE, Zhang K, Tierney DM, Millner P, Giovannini D, Barron K, Novak W, Patel SA, Dversdal R, Cox EJ, Lopresti CM (2021) : Integration of point of Care Ultrasound Education into the Internal Medicine Core Clerkship Experience.Journal of Ultrasound in Medicine
Olszynski P, Kim D, Chenkin J, Rang L (2018) The core emergency ultrasound curriculum project: a report from the curriculum Working Group of the CAEP Emergency Ultrasound Committee. CJEM 20:176–182
Lopresti CM, Jensen TP, Dversdal RK, Astiz DJ (2019) Point-of-care Ultrasound for Internal Medicine Residency Training: A position Statement from the Alliance of Academic Internal Medicine. Am J Med 132:1356–1360
Arntfield R, Millington S, Ainsworth C, Arora R, Boyd J, Finlayson G, Gallagher W, Gebhardt C, Goffi A, Hockman E et al (2014) Canadian recommendations for critical care ultrasound training and competency. Can Respir J 21:341–345
Hanson MG, Chan B (2021) : The role of point-of-care ultrasound in the diagnosis of pericardial effusion: a single academic center retrospective study.The Ultrasound Journal13
Sheth A, Dabo-Trubelja A (2021) Perioperative focused cardiac ultrasound: a brief report. J Anesth Crit Care 13:55–60
Fitzgibbon JB, Lovallo E, Escajeda J, Radomski MA, Martin-Gill C (2019) Feasibility of out-of-hospital cardiac arrest Ultrasound by EMS Physicians. Prehospital Emerg Care 23:297–303
Moulson N, Jaff Z, Wiltshire V, Taylor T, O’Connor HM, Hopman WM, Johri AM (2019) Feasibility and reliability of Nonexpert POCUS for Cardiovascular Preparticipation Screening of Varsity athletes: the SHARP Protocol. Can J Cardiol 35:35–41
Bøtker MT, Jacobsen L, Rudolph SS, Knudsen L (2018) : The role of point of care ultrasound in prehospital critical care: a systematic review.Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine26
Razi R, Estrada JR, Doll J, Spencer KT (2011) Bedside hand-carried ultrasound by internal medicine residents versus traditional clinical assessment for the identification of systolic dysfunction in patients admitted with decompensated heart failure. J Am Soc Echocardiogr 24:1319–1324
Cullen MW, Blauwet LA, Vatury OM, Mulvagh SL, Behrenbeck TR, Scott CG, Pellikka PA (2014) Diagnostic capability of comprehensive handheld vs transthoracic echocardiography. Mayo Clin Proc 89:790–798
Johnson BK, Tierney DM, Rosborough TK, Harris KM, Newell MC (2016) Internal medicine point-of-care ultrasound assessment of left ventricular function correlates with formal echocardiography. J Clin Ultrasound 44:92–99
Perera P, Mailhot T, Riley D, Mandavia D (2010) The RUSH exam: Rapid Ultrasound in SHock in the evaluation of the critically lll. Emerg Med Clin North Am 28:29–56
Jensen MB, Sloth E, Larsen KM, Schmidt MB (2004) Transthoracic echocardiography for cardiopulmonary monitoring in intensive care. Eur J Anaesthesiol 21:700–707
Kirkpatrick JN, Grimm R, Johri AM, Kimura BJ, Kort S, Labovitz AJ, Lanspa M, Phillip S, Raza S, Thorson K, Turner J (2020) Recommendations for Echocardiography Laboratories participating in Cardiac Point of Care Cardiac Ultrasound (POCUS) and critical Care Echocardiography Training: Report from the American Society of Echocardiography. J Am Soc Echocardiogr 33:409–422e404
Johri AM, Galen B, Kirkpatrick JN, Lanspa M, Mulvagh S, Thamman R (2020) ASE Statement on Point-of-care Ultrasound during the 2019 Novel Coronavirus Pandemic. J Am Soc Echocardiogr 33:670–673
Emergency Ultrasound Imaging Criteria Compendium (2016) Ann Emerg Med 68:e11–48
Mayo PH, Beaulieu Y, Doelken P, Feller-Kopman D, Harrod C, Kaplan A, Oropello J, Vieillard-Baron A, Axler O, Lichtenstein D et al (2009) American college of chest Physicians/La Societe de Reanimation de Langue Francaise statement on competence in critical care ultrasonography. Chest 135:1050–1060
Mitchell C, Rahko PS, Blauwet LA, Canaday B, Finstuen JA, Foster MC, Horton K, Ogunyankin KO, Palma RA, Velazquez EJ (2019) Guidelines for performing a comprehensive transthoracic echocardiographic examination in adults: recommendations from the American Society of Echocardiography. J Am Soc Echocardiogr 32:1–64
Luong C, Saboktakin Rizi S, Gin K, Jue J, Yeung DF, Tsang MYC, Sayre EC, Tsang TSM (2021) : Prevalence of left ventricular systolic dysfunction by single echocardiographic view: towards an evidence-based point of care cardiac ultrasound scanning protocol.The International Journal of Cardiovascular Imaging
Abdi A, Luong C, Tsang T, Jue J, Gin K, Yeung D, Hawley D, Rohling R, Abolmaesumi P (2017) Quality Assessment of echocardiographic cine using recurrent neural networks: feasibility on five Standard View Planes. In: Descoteaux M, Maier-Hein L, Franz A, Jannin P, Collins D, Duchesne S (eds) Medical Image Computing and Computer-Assisted intervention – MICCAI 2017. Lecture Notes in Computer Science
Luong C, Liao Z, Abdi A, Girgis H, Rohling R, Gin K, Jue J, Yeung D, Szefer E, Thompson D et al (2020) : Automated estimation of echocardiogram image quality in hospitalized patients.The International Journal of Cardiovascular Imaging
Van Woudenberg N, Liao Z, Abdi AH, Girgis H, Luong C, Vaseli H, Behnami D, Zhang H, Gin K, Rohling R et al (2018) Quantitative Echocardiography: Real-Time Quality Estimation and View classification implemented on a Mobile Android device. In; Cham. Springer International Publishing, pp 74–81
Tighe DA, Rosetti M, Vinch CS, Chandok D, Muldoon D, Wiggin B, Dahlberg ST, Aurigemma GP (2007) Influence of image quality on the accuracy of real time three-dimensional echocardiography to measure left ventricular volumes in unselected patients: a comparison with gated-SPECT imaging. Echocardiography 24:1073–1080
Hoffmann R, Lethen H, Marwick T, Arnese M, Fioretti P, Pingitore A, Picano E, Buck T, Erbel R, Flachskampf FA, Hanrath P (1996) Analysis of interinstitutional observer agreement in interpretation of dobutamine stress echocardiograms. J Am Coll Cardiol 27:330–336
Kusunose K, Shibayama K, Iwano H, Izumo M, Kagiyama N, Kurosawa K, Mihara H, Oe H, Onishi T, Ota M et al (2018) : Reduced variability of visual left ventricular ejection fraction assessment with reference images: the Japanese Association of Young Echocardiography Fellows multicenter study.J Cardiol
Nagata Y, Kado Y, Onoue T, Otani K, Nakazono A, Otsuji Y, Takeuchi M (2018) Impact of image quality on reliability of the measurements of left ventricular systolic function and global longitudinal strain in 2D echocardiography. Echo Res Pract 5:27–39
Medvedofsky D, Mor-Avi V, Byku I, Singh A, Weinert L, Yamat M, Kruse E, Ciszek B, Nelson A, Otani K et al (2017) Three-dimensional echocardiographic automated quantification of Left Heart Chamber volumes using an adaptive analytics Algorithm: feasibility and impact of Image Quality in Nonselected Patients. J Am Soc Echocardiogr 30:879–885
Huang G, Liu Z, van der Maaten L, Weinberger KQ (2017) : Densely connected Convolutional Networks.Computer Vision and Pattern Recognition1(2)
Ioffe S, Szegedy C (2015) Batch normalization: accelerating deep network training by reducing internal covariate shift. ICML 37:448–456
Hochreiter S, Schmidhuber J (1997) Long short-term memory. Neural Comput 9:1735–1780
Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L, Flachskampf FA, Foster E, Goldstein SA, Kuznetsova T et al (2015) Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr 28:1–39e14
Zhang J, Gajjala S, Agrawal P, Tison GH, Hallock LA, Beussink-Nelson L, Lassen MH, Fan E, Aras MA, Jordan C et al (2018) Fully automated Echocardiogram Interpretation in Clinical Practice. Circulation 138:1623–1635
Thaden JJ, Tsang MY, Ayoub C, Padang R, Nkomo VT, Tucker SF, Cassidy CS, Bremer M, Kane GC, Pellikka PA (2017) : Association between Echocardiography Laboratory Accreditation and the quality of imaging and reporting for Valvular Heart Disease.Circ Cardiovasc Imaging10
Hensel KO, Roskopf M, Wilke L, Heusch A (2018) Intraobserver and interobserver reproducibility of M-mode and B-mode acquired mitral annular plane systolic excursion (MAPSE) and its dependency on echocardiographic image quality in children. PLoS ONE 13:e0196614
Lee KC, Liu S, Callahan P, Green T, Jarrett T, Cochran JD, Mei Y, Mobasseri S, Sayegh H, Rangarajan V et al (2021) : Routine use of contrast on Admission Transthoracic Echocardiography for Heart failure reduces the rate of repeat Echocardiography during Index Admission.J Am Soc Echocardiogr
Ellenberger K, Jeyaprakash P, Sivapathan S, Sangha S, Kitley J, Darshni A, Chen D, Negishi K, Pathan F (2021) The effect of obesity on echocardiographic image quality. Heart Lung Circ
Spencer KT, Kimura BJ, Korcarz CE, Pellikka PA, Rahko PS, Siegel RJ (2013) Focused cardiac ultrasound: recommendations from the American Society of Echocardiography. J Am Soc Echocardiogr 26:567–581
Levitov A, Frankel HL, Blaivas M, Kirkpatrick AW, Su E, Evans D, Summerfield DT, Slonim A, Breitkreutz R, Price S et al (2016) Guidelines for the appropriate use of Bedside General and Cardiac Ultrasonography in the evaluation of critically Ill Patients-Part II: Cardiac Ultrasonography. Crit Care Med 44:1206–1227
Atkinson P, Bowra J, Lambert M, Lamprecht H, Noble V, Jarman B (2015) International Federation for Emergency Medicine point of care ultrasound curriculum. CJEM 17:161–170
International expert statement (2011) On training standards for critical care ultrasonography. Intensive Care Med 37:1077–1083
Behnami D, Luong C, Vaseli H, Abdi A, Girgis H, Hawley D, Rohling R, Gin K, Abolmaesumi P, Tsang T (2018) Automatic detection of patients with a high risk of systolic cardiac failure in Echocardiography. In; Cham. Springer International Publishing, pp 65–73
Funding
This work was supported by the Vancouver Coastal Health Research Institute and Canadian Institutes of Health Research.
Author information
Authors and Affiliations
Contributions
C. Luong and D. Behnami contributed equally to this manuscript as co-first authors. T. Tsang and P. Abolmaesumi contributed equally to this manuscript as co-senior authors.
Corresponding author
Ethics declarations
Disclosures
No disclosures.
Competing interests
The authors have no relevant financial or non-financial interests to disclose.
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of the University of British Columbia.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Co-first authors: Christina L. Luong and Delaram Behnami contributed equally to this manuscript.
Co-senior authors: Purang Abolmaesumi and Teresa S. M. Tsang
Rights and permissions
About this article
Cite this article
Luong, C.L., Behnami, D., Liao, Z. et al. Machine learning derived echocardiographic image quality in patients with left ventricular systolic dysfunction: insights on the echo views of greatest image quality. Int J Cardiovasc Imaging 39, 1313–1321 (2023). https://doi.org/10.1007/s10554-023-02802-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-023-02802-4