Abstract
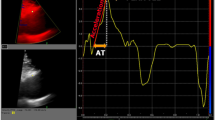
This study investigated the impact of bicuspid aortic valve (BAV) on valve morphology and motion as well as proximal and aortic hemodynamics using a same-day echocardiography and cardiac MRI. Transthoracic echocardiography, two-dimensional cine MRI of the aortic valve, and aortic 4D flow MRI were performed on the same day in 9 normofunctional BAV patients (age = 41 ± 12, 3 female), 4 BAV with moderate to severe aortic stenosis (AS) (age = 63 ± 5, 1 female), and 36 healthy tricuspid aortic valve controls (age = 52 ± 10, 21 female). Valve opening and closing timings and transvalvular peak velocity were measured using B-mode and Doppler echocardiogram, respectively. Valve orifice morphology at a fully-opened state was characterized using cine MRI. Ascending aortic (AAo) wall shear stress (WSS) was measured using 4D flow MRI data. Valve motion timings were similar between BAV and controls. BAV was associated with an increased orifice aspect ratio (1.44 ± 0.11 vs. 1.10 ± 0.13, P < 0.001), transvalvular peak velocity (1.5 ± 0.3 vs. 1.2 ± 0.2 m/s, P < 0.001) and maximum AAo WSS (1.62 ± 0.31 vs. 0.91 ± 0.24 Pa, P < 0.001). The increased orifice aspect ratio was associated with the increase in transvalvular peak velocity (r = 0.80, P < 0.0001) and maximum AAo WSS (r = 0.83, P < 0.0001). Transvalvular peak velocity was also positively correlated with maximum AAo WSS (r = 0.83, P < 0.0001). A same-day echo and MRI imaging allows for a comprehensive assessment of the impact of aortic valve disease on valve function and hemodynamics. In this pilot application to BAV, we found increased orifice aspect ratio may be responsible for increased transvalvular peak velocity and maximum AAo WSS.





Similar content being viewed by others
References
Virani SS, Alonso A, Aparicio HJ et al (2021) Heart disease and stroke statistics—2021 update: a report from the American Heart Association. Circulation 143(8):e254–e743
Fedak PW, Verma S, David TE et al (2002) Clinical and pathophysiological implications of a bicuspid aortic valve. Circulation 106(8):900–904
Michelena HI, Khanna AD, Mahoney D et al (2011) Incidence of aortic complications in patients with bicuspid aortic valves. JAMA 306(10):1104–1112
Girdauskas E, Borger MA, Secknus M-A et al (2011) Is aortopathy in bicuspid aortic valve disease a congenital defect or a result of abnormal hemodynamics? A critical reappraisal of a one-sided argument. Circulation 39(6):809–814
Bissell MM, Hess AT, Biasiolli L et al (2013) Aortic dilation in bicuspid aortic valve disease: flow pattern is a major contributor and differs with valve fusion type. Circulation 6(4):499–507
Mahadevia R, Barker AJ, Schnell S et al (2014) Bicuspid aortic cusp fusion morphology alters aortic three-dimensional outflow patterns, wall shear stress, and expression of aortopathy. Circulation 129(6):673–682
Mirabella L, Barker AJ, Saikrishnan N et al (2015) MRI-based protocol to characterize the relationship between bicuspid aortic valve morphology and hemodynamics. Ann Biomed Eng 43(8):1815–1827
Raghav V, Barker AJ, Mangiameli D et al (2018) Valve mediated hemodynamics and their association with distal ascending aortic diameter in bicuspid aortic valve subjects. J Magn Reson Imaging 47(1):246–254
Hope MD, Hope TA, Meadows AK et al (2010) Bicuspid aortic valve: four-dimensional MR evaluation of ascending aortic systolic flow patterns. Radiology 255(1):53–61
Dolan JM, Kolega J, Meng H (2013) High wall shear stress and spatial gradients in vascular pathology: a review. Ann Biomed Eng 41(7):1411–1427
Bollache E, Guzzardi DG, Sattari S et al (2018) Aortic valve-mediated wall shear stress is heterogeneous and predicts regional aortic elastic fiber thinning in bicuspid aortic valve-associated aortopathy. J Thorac Cardiovasc Surg 156(6):2112–2120
Meierhofer C, Schneider EP, Lyko C et al (2013) Wall shear stress and flow patterns in the ascending aorta in patients with bicuspid aortic valves differ significantly from tricuspid aortic valves: a prospective study. Eur Heart J 14(8):797–804
Rodríguez-Palomares JF, Dux-Santoy L, Guala A et al (2018) Aortic flow patterns and wall shear stress maps by 4D-flow cardiovascular magnetic resonance in the assessment of aortic dilatation in bicuspid aortic valve disease. J Cardiovasc Magn Reson 20(1):1–15
Guzzardi DG, Barker AJ, Van Ooij P et al (2015) Valve-related hemodynamics mediate human bicuspid aortopathy: insights from wall shear stress mapping. J Am Coll Cardiol 66(8):892–900
Baumgartner H, Hung J, Bermejo J et al (2016) Recommendations on the echocardiographic assessment of aortic valve stenosis: a focused update from the European Association of Cardiovascular Imaging and the American Society of Echocardiography. Eur Heart J 18(3):254–275
De Paulis R, De Matteis GM, Nardi P et al (2001) Opening and closing characteristics of the aortic valve after valve-sparing procedures using a new aortic root conduit. Ann Thorac Surg 72(2):487–494
Leyh RG, Schmidtke C, Sievers H-H et al (1999) Opening and closing characteristics of the aortic valve after different types of valve-preserving surgery. Circulation 100(21):2153–2160
Bazett HCJH (1920) An analysis of the time relations of electrocardiograms. Heart 7:353–370
Walker PG, Cranney GB, Scheidegger MB et al (1993) Semiautomated method for noise reduction and background phase error correction in MR phase velocity data. J Magn Reson Imaging 3(3):521–530
Berhane H, Scott M, Elbaz M et al (2020) Fully automated 3D aortic segmentation of 4D flow MRI for hemodynamic analysis using deep learning. Magn Reson Med 84:2204
Potters WV, van Ooij P, Marquering H et al (2015) Volumetric arterial wall shear stress calculation based on cine phase contrast MRI. J Magn Reson Imaging 41(2):505–516
Gordon DZ, Abbasi MA, Lee J et al (2020) Four-dimensional flow magnetic resonance imaging quantification of blood flow in bicuspid aortic valve. J Thorac Imaging 35(6):383–388
Rahman O, Scott M, Bollache E et al (2019) Interval changes in aortic peak velocity and wall shear stress in patients with bicuspid aortic valve disease. Int J Cardiovasc Imaging 35(10):1925–1934
Athar M, Ansari M, Khan M (2003) Flow characteristics of elliptical orifice plates. ISH J Hydraul Eng 9(2):22–35
Flachskampf FA, Weyman AE, Guerrero JL et al (1990) Influence of orifice geometry and flow rate on effective valve area: an in vitro study. J Am Coll Cardiol 15(5):1173–1180
Kamimura D, Hans S, Suzuki T et al (2016) Delayed time to peak velocity is useful for detecting severe aortic stenosis. J Am Heart Assoc 5(10):e003907
Kim SH, Kim JS, Kim BS et al (2014) Time to peak velocity of aortic flow is useful in predicting severe aortic stenosis. Int J Cardiol 172(3):e443–e446
van Ooij P, Markl M, Collins JD et al (2017) Aortic valve stenosis alters expression of regional aortic wall shear stress: new insights from a 4-dimensional flow magnetic resonance imaging study of 571 subjects. J Am Heart Assoc 6(9):e005959
Fries R, Graeter T, Aicher D et al (2006) In vitro comparison of aortic valve movement after valve-preserving aortic replacement. J Thorac Cardiovasc Surg 132(1):32–37
Higashidate M, Tamiya K, Beppu T et al (1995) Regulation of the aortic valve opening: in vivo dynamic measurement of aortic valve orifice area. J Thorac Cardiovasc Surg 110(2):496–503
Thubrikar M, Bosher LP, Nolan SP (1979) The mechanism of opening of the aortic valve. J Thorac Cardiovasc Surg 77(6):863–870
Bellhouse B, Bellhouse F (1968) Mechanism of closure of the aortic valve. Nature 217(5123):86–87
Soulat G, Scott MB, Allen BD et al (2022) Association of regional wall shear stress and progressive ascending aorta dilation in bicuspid aortic valve. Cardiovasc Imaging 15(1):33–42
Acknowledgements
This study was supported by NIH R01HL115828 and R01HL133504. We would also like to thank General Electric, Inc., and the Irene D. Pritzker foundation for their financial and equipment support for this study.
Funding
This study was supported by NIH R01HL115828 and R01HL133504. We would also like to thank General Electric, Inc., and the Irene D. Pritzker foundation for their financial and equipment support for this study.
Author information
Authors and Affiliations
Contributions
All authors have made significant contributions to this work and read and commented on previous manuscript versions. JL performed echocardiography and MRI image-processing, statistical data analysis and drafted the first version of the manuscript. NEH, AP, and GS participated in image processing and clinical data interpretation. AB was a senior investigator instrumental in study conceptualization and data acquisition management. JT and MM were principal investigators who conceived this study and provided clinical and technical guidance of echocardiography and MRI data interpretation.
Corresponding author
Ethics declarations
Conflict of interest
All authors have no relevant financial or non-financial competing interests to report.
Ethical approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Internal Review Board of Northwestern University (STU00204434).
Consent to participate
Informed consent was obtained from all individuals who participated in the study.
Consent to publish
The authors affirm that human research participants provided informed consent to publish the study results.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lee, J., El Hangouche, N., Pathrose, A. et al. Bicuspid aortic valve morphology and hemodynamics by same-day echocardiography and cardiac MRI. Int J Cardiovasc Imaging 38, 2047–2056 (2022). https://doi.org/10.1007/s10554-022-02593-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-022-02593-0