Abstract
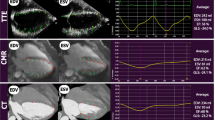
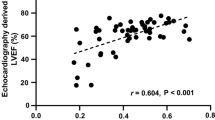
Automated function imaging (AFI, GE Healthcare) is a novel promising algorithm of speckle-tracking echocardiography that combines two-dimensional strain and AI technology. It shortens the analysis time, saves the cost associated with streamlining of image acquisition, rapid analysis, and reporting, and has greater accuracy and reproducibility of measurements. This study aimed to evaluate the reliability and feasibility of AFI for the quantification of left ventricular (LV) volumes and function in patients with LV dilation by comparison with CMR. We retrospectively studied 50 patients with LV dilation on echocardiography whom both underwent CMR and coronary angiography within three days. LV volumes, ejection fraction (EF), and global longitudinal strain (GLS) were measured from 3 long-axis cine-views via the AFI technique in two modes: without editing (auto-AFI) and with partial border editing (semi-auto-AFI). The LV volumes and EF were also measured with 2D Simpson’s biplane method, and CMR, as the standard method, was used for comparison. The AFI method still had significantly underestimated the LV volumes compared with CMR (P<0.01), but there were no significant differences between the AFI method and the conventional Simpson’s biplane method. There were no significant differences in EF between CMR and the AFI method with good correlations (auto-AFI: r = 0.81, semi-auto-AFI: r = 0.86). The auto-AFI method provided the most rapid analysis and excellent reproducibility, while the semi-auto-AFI method further improved measurement accuracy. However, there were no significant differences in LV volumes and EF between these two AFI methods. The accuracy of AFI seems to be more affected by the image quality than the left ventricular morphology. AFI enables accurate, efficient, and rapid evaluation of LV volumes and EF in patients with dilated LV, with good reproducibility and correlations with CMR.






Similar content being viewed by others
Data availability
The datasets supporting the results of this article are included within the article.
References
Virani SS, Alonso A, Benjamin EJ, Bittencourt MS, Callaway CW, Carson AP et al (2020) Heart disease and stroke statistics-2020 update: a report from the American heart association. Circulation 141:e139–e596. https://doi.org/10.1161/cir.0000000000000757
Hao G, Wang X, Chen Z, Zhang L, Zhang Y, Wei B et al (2019) Prevalence of heart failure and left ventricular dysfunction in China: the China Hypertension Survey, 2012-2015. Eur J Heart Fail 21:1329–1337. https://doi.org/10.1002/ejhf.1629
Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JG, Coats AJ et al (2016) [2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure]. Kardiol Pol 74:1037–1147. https://doi.org/10.5603/kp.2016.0141
Wang HB, Yang J, Shuai W, Yang J, Liu LB, Xu M et al (2020) Deletion of microfibrillar-associated protein 4 attenuates left ventricular remodeling and dysfunction in heart failure. J Am Heart Assoc 9:e015307. https://doi.org/10.1161/jaha.119.015307
Han LN, Guo SL, Lin XM, Shi XM, Zang CB, Yang LM et al (2014) Torasemide reduces dilated cardiomyopathy, complication of arrhythmia, and progression to heart failure. Genet Mol Res 13:7262–7274. https://doi.org/10.4238/2014.September.5.11
Arnold JR, Cann MC (2020) Cardiovascular magnetic resonance: applications and practical considerations for the general cardiologist. Heart 106:174–181. https://doi.org/10.1136/heartjnl-2019-314856
Su X, Yang W, Zhu Z, Zhang R, Fang Y (2021) Heartech® left ventricular partitioning device improves left ventricular systolic function of patients with chronic heart failure post-myocardial infarction at 1-year follow-up. Catheter Cardiovasc Interv. https://doi.org/10.1002/ccd.29489
Lilli A, Tessa C, Diciotti S, Croisille P, Clarysse P, Del Meglio J et al (2017) Simultaneous strain-volume analysis by three-dimensional echocardiography: validation in normal subjects with tagging cardiac magnetic resonance. J Cardiovasc Med (Hagerstown) 18:223–229. https://doi.org/10.2459/jcm.0000000000000336
Hua W, Yang W, Gu J, Wu J, Wang W, Liu Y et al (2021) Risk factors for right ventricular dysfunction in patients with lymphangioleiomyomatosis. Int J Cardiovasc Imaging 37:439–448. https://doi.org/10.1007/s10554-020-02009-x
Barbier P, Mirea O, Cefalù C, Maltagliati A, Savioli G, Guglielmo M (2015) Reliability and feasibility of longitudinal AFI global and segmental strain compared with 2D left ventricular volumes and ejection fraction: intra- and inter-operator, test-retest, and inter-cycle reproducibility. Eur Heart J Cardiovasc Imaging 16:642–652. https://doi.org/10.1093/ehjci/jeu274
Zito C, Longobardo L, Citro R, Galderisi M, Oreto L, Carerj ML et al (2018) Ten years of 2D longitudinal strain for early myocardial dysfunction detection: a clinical overview. Biomed Res Int 2018:8979407. https://doi.org/10.1155/2018/8979407
Hendriks T, Ali A, Maagdenberg L, van Melle CG, Hummel JP, Oudkerk YM et al (2019) Agreement of 2D transthoracic echocardiography with cardiovascular magnetic resonance imaging after ST-elevation myocardial infarction. Eur J Radiol 114:6–13. https://doi.org/10.1016/j.ejrad.2019.02.039
Voigt JU, Cvijic M (2019) 2- and 3-dimensional myocardial strain in cardiac health and disease. JACC Cardiovasc Imaging 12:1849–1863. https://doi.org/10.1016/j.jcmg.2019.01.044
Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L et al (2015) Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American society of echocardiography and the european association of cardiovascular imaging. J Am Soc Echocardiogr 28:1–39e14. https://doi.org/10.1016/j.echo.2014.10.003
Vahanian A, Beyersdorf F, Praz F, Milojevic M, Baldus S, Bauersachs J et al (2021) 2021 ESC/EACTS Guidelines for the management of valvular heart disease. Eur Heart J. https://doi.org/10.1093/eurheartj/ehab395
Lang RM et al (2016) Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the american society of echocardiography and the european association of, cardiovascular imaging. Eur Heart J Cardiovasc Imaging 17:412. https://doi.org/10.1093/ehjci/jew041
Medvedofsky D, Mor-Avi V, Byku I, Singh A, Weinert L, Yamat M et al (2017) Three-dimensional echocardiographic automated quantification of left heart chamber volumes using an adaptive analytics algorithm: feasibility and impact of image quality in nonselected patients. J Am Soc Echocardiogr 30:879–885. https://doi.org/10.1016/j.echo.2017.05.018
Knackstedt C, Bekkers SCAM, Schummers G, Schreckenberg M, Muraru D, Badano LP et al (2015) Fully automated versus standard tracking of left ventricular ejection fraction and longitudinal strain. J Am Coll Cardiol 66:1456–1466. https://doi.org/10.1016/j.jacc.2015.07.052
O’Grady H, Mostafa K, Zafar H, Lohan D, Morris L, Sharif F (2019) Changes in left ventricular shape and morphology in the presence of heart failure: a four-dimensional quantitative and qualitative analysis. Int J Comput Assist Radiol Surg 14:1415–1430. https://doi.org/10.1007/s11548-019-01985-3
Cohn JN, Ferrari R, Sharpe N (2000) Cardiac remodeling--concepts and clinical implications: a consensus paper from an international forum on cardiac remodeling. Behalf of an International Forum on Cardiac Remodeling. J Am Coll Cardiol 35:569–582. https://doi.org/10.1016/s0735-1097(99)00630-0
Knackstedt C, Bekkers SC, Schummers G, Schreckenberg M, Muraru D, Badano LP et al (2015) automated versus standard tracking of left ventricular ejection fraction and longitudinal strain: the FAST-EFs multicenter study. J Am Coll Cardiol 66:1456–1466. https://doi.org/10.1016/j.jacc.2015.07.052
Nolan MT, Thavendiranathan P (2019) Automated quantification in echocardiography. JACC Cardiovasc Imaging 12:1073–1092. https://doi.org/10.1016/j.jcmg.2018.11.038
Medvedofsky D, Maffessanti F, Weinert L, Tehrani DM, Narang A, Addetia K et al (2018) 2D and 3D echocardiography-derived indices of left ventricular function and shape: relationship with mortality. JACC Cardiovasc Imaging 11:1569–1579. https://doi.org/10.1016/j.jcmg.2017.08.023
Volpato V, Mor-Avi V, Narang A, Prater D, Gonçalves A, Tamborini G et al (2019) Automated, machine learning-based, 3D echocardiographic quantification of left ventricular mass. Echocardiography 36:312–319. https://doi.org/10.1111/echo.14234
Potter E, Marwick TH (2018) Assessment of left ventricular function by echocardiography: the case for routinely adding global longitudinal strain to ejection fraction. JACC Cardiovasc Imaging 11:260–274. https://doi.org/10.1016/j.jcmg.2017.11.017
Myhr KA, Pedersen FHG, Kristensen CB, Visby L, Hassager C, Mogelvang R (2018) Semi-automated estimation of left ventricular ejection fraction by two-dimensional and three-dimensional echocardiography is feasible, time-efficient, and reproducible. Echocardiography 35:1795–1805. https://doi.org/10.1111/echo.14112
Kalam K, Otahal P, Marwick TH (2014) Prognostic implications of global LV dysfunction: a systematic review and meta-analysis of global longitudinal strain and ejection fraction. Heart 100:1673–1680. https://doi.org/10.1136/heartjnl-2014-305538
Funding
None.
Author information
Authors and Affiliations
Contributions
YF and ZS conceived and designed the study. YC, WY, and WH collected the data and performed analysis. YC drafted the manuscript. All authors critically reviewed data analysis and the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study was approved by the Ethics Committee of Ruijin Hospital Affiliated with Shanghai Jiaotong University School of Medicine.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chen, Y., Hua, W., Yang, W. et al. Reliability and feasibility of automated function imaging for quantification in patients with left ventricular dilation: comparison with cardiac magnetic resonance. Int J Cardiovasc Imaging 38, 1267–1276 (2022). https://doi.org/10.1007/s10554-021-02510-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-021-02510-x