Abstract
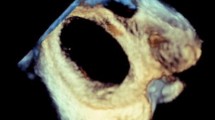
In patients undergoing percutaneous closure of secundum atrial septal defect, the device selection is decided based on three-dimensional transesophageal echocardiography (3D TEE) measurements and two-dimensional balloon stretched diameter measurements; more importantly balloon sizing. The purpose of the study was to assess whether in patients with “halo-sign”, defined as increased tissue thickness at the edge of the ASD rims, there is an agreement between 3D TEE and 2D balloon stretched diameter aiming to avoidance of balloon sizing. Forty consecutive patients who underwent closure of a single, without complex anatomy ASD were included. 3D and 2D TEE datasets were acquired and analyzed offline. Planimetry was used to calculate circumference derived diameter of ASD from 3D datasets. Patients were classified according to the presence of the “halo sign” and the agreement between circumference derived diameter and balloon stretched diameter was examined. Forty consecutive patients who underwent closure of a single, without complex anatomy ASD were included. 3D and 2D TEE datasets were acquired and analyzed offline. Planimetry was used to calculate circumference derived diameter of ASD from 3D datasets. Patients were classified according to the presence of the “halo sign” and the agreement between circumference derived diameter and balloon stretched diameter was examined. Higher correlation and lower median absolute difference between 3D TEE measurements and 2D stretched balloon diameter was found in patients with “halo sign”. In patients with the “halo sign” mean diameter difference was non-significant. On the contrary statistically significant difference was found in patients without the “halo sign”. Significant difference was also found when comparing mean difference in the two patient groups. ASD sizing by 3D echocardiography, is accurate in patients with halo sign and it correlates well with the balloon sizing method. This study justifies further investigation concerning the reliability of 3D imaging for the selection of the ASD device size with a view to avoid balloon sizing, decrease procedural time and thus simplify the procedure.






Similar content being viewed by others
References
Hoffman JI, Kaplan S (2002) The incidence of congenital heart disease. J Am Coll Cardiol 39:1890–1900
Fraisse A, Latchman M, Sharma S et al (2018) Atrial septal defect closure: indications and contra-indications. J Thorac Dis 10(Suppl 24):S2874–S2881
Cowley CG, Lloyd TR, Bove EL et al (2001) Comparison of results of closure of secundum atrial septal defect by surgery versus Amplatzer septal occluder. Am J Cardiol 88:589–591
Du ZD, Hijazi ZM, Kleinman CS et al (2002) Comparison between transcatheter and surgical closure of secundum atrial septal defect in children and adults: results of a multicenter nonrandomized trial. J Am Coll Cardiol 39:1836–1844
Vaidyanathan B, Simpson JM, Kumar RK (2009) Transesophageal echocardiography for device closure of atrial septal defects case selection. JACC Cardiovasc Imaging 10:1238–1427
Faletra FF, Ho SY, Auricchio A (2010) Anatomy of right atrial structures by real time 3D transesophageal echocardiography. JACC Cardiovasc Imaging 3:966–975
Roberson DA, Cui VW (2014) Three-dimensional transesophageal echocardiography of atrial septal defect device closure. Curr Cardiol Rep 16(2):453
Karsenty C, Hadeed K, Acar P (2018) Interventional catheterization and echocardiography: an indefectible link illustrated by atrial septal defect closure. Arch Cardiovasc Dis 111(6–7):392–394
Savis A, Simpson J (2018) Echocardiographic approach to catheter closure of atrial septal defects: patient selection, procedural guidance and post-procedural checks. Echo Res Pract 5(2):R49–R64
Seo JS, Song JM, Kim YH et al (2012) Effect of atrial septal defect shape evaluated using three-dimensional transesophageal echocardiography on size measurements for percutaneous closure. J Am Soc Echocardiogr 25(10):1031–1040
Godart F, Houeijeh A, Recher M et al (2015) Transcatheter closure of atrial septal defect with the Figulla(®) ASD Occluder: a comparative study with the Amplatzer(®) Septal Occluder. Arch Cardiovasc Dis 108(1):57–63
Butera G, Biondi-Zoccai G, Sangiorgi G et al (2011) Percutaneous versus surgical closure of secundum atrial septal defects: a systematic review and meta-analysis of currently available clinical evidence. EuroIntervention 7:377–385
Du ZD, Hijazi ZM, Kleinman CS, Silverman NH, Larntz K (2002) Comparison between transcatheter and surgical closure of secundum atrial septal defect in children and adults: results of a multicenter nonrandomized trial. J Am Coll Cardiol 39:1836–1844
Papachristidis A, Papitsas M, Roper D et al (2017) Three-dimensional measurement of aortic annulus dimensions using area or circumference for transcatheter aortic valve replacement valve sizing: does it make a difference? J Am Soc Echocardiogr 30(9):871–878
Abdel-Massih T, Dulac Y, Taktak A et al (2005) Assessment of atrial septal defect size with 3D-transesophageal echocardiography: comparison with balloon method. Echocardiography 22:121–127
Hascoet S, Hadeed K, Marchal P et al (2015) The relation between atrial septal defect shape, diameter, and area using three-dimensional transesophageal echocardiography and balloon sizing during percutaneous closure in children. Eur Hear J Cardiovasc Imaging 16(7):747–755
Barueau AE, Petit J, Lambert V et al (2014) Trancatheter closure of large atrial septal defects: feasibility and safety in a large adult and pediatric population. Circ Cardiovasc Interv 7(6):837–843
Turner DR, Owada CY, Sang CJ, Khan M, Lim DS (2017) Closure of secundum atrial septal defects with the AMPLATZER septal occluder: a prospective multicenter, post-approval study. Circ Cardiovasc Interv 10(8):e004212
Suda K, Raboisson MJ, Piette E, Dahdah NS, Miro J (2004) Reversible atrioventricular block associated with closure of atrial septal defects using the Amplatzer device. J Am Coll Cardiol 43:1677–1682
Schoen SP, Boscheri A, Lange SA et al (2008) Incidence of aortic valve regurgitation and outcome after percutaneous closure of atrial septal defects and patent foramen ovale. Heart 94:844–847
Amin Z, Hijazi ZM, Bass JL, Cheatham JP, Hellenbrand WE, Kleinman CS (2004) Erosion of Amplatzer septal occluder device after closure of secundum atrial septal defects: review of registry of complications and recommendations to minimize future risk. Catheter Cardiovasc Interv 63:496–502
Kannan BR, Francis E, Sivakumar K, Anil SR, Kumar RK (2003) Transcatheter closure of very large (≥ 25 mm) atrial septal defects using the Amplatzer septal occluder. Catheter Cardiovasc Interv 59:522–527
Berger F, Vogel M, Alexi-Meskishvili V, Lange PE (1999) Comparison of results and complications of surgical and Amplatzer device closure of atrial septal defects. J Thorac Cardiovasc Surg 118:674–678
McElhinney DB, Quertermain MD, Kenny D, Alboliras E, Amin Z (2016) Relative risk factors for cardiac erosion following transcatheter closure of atrial septal defects: a case-control study. Circulation 133(18):1738–1746
Aggeli C, Verveniotis A, Andrikopoulou E, Vavuranakis E, Toutouzas K, Tousoulis D (2018) Echocardiographic features of PFOs and paradoxical embolism: a complicated puzzle. Int J Cardiovasc Imaging 34:1849–1861
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary material 1 (AVI 2863 kb)
Supplementary material 2 (AVI 2595 kb)
Supplementary material 3 (MP4 33552 kb)
Rights and permissions
About this article
Cite this article
Aggeli, C., Apostolou, I., Dimitroglou, Y. et al. The role of ‘halo sign’ for the accurate quantification of atrial septal defect size with 3D TEE. Int J Cardiovasc Imaging 36, 873–881 (2020). https://doi.org/10.1007/s10554-020-01786-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-020-01786-9