Abstract
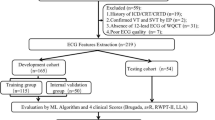
Up to one-third of patients selected by current guidelines do not respond to cardiac resynchronization therapy (CRT), the aim of this study was to find out novel analytical approaches to improve pre-implantation CRT response prediction. Among 31 pre-implantation features of clinical, laboratory, electrocardiography (ECG), and echocardiography variables in a consecutive cohort of patients receiving a first-time CRT device (CRT-pacemaker or CRT-defibrillator), we developed a machine learning (ML) model with three classification algorithms (support vector machines (SVM), K nearest neighbors, and random subspaces) with the best features combination to predict CRT response. Three categorical variables, left bundle branch block (LBBB), nonischemic cardiomyopathy, and female gender, were independently associated with CRT responses. Among continuous variables, including septal wall thickness, posterior wall thickness, and relative wall thickness (RWT), could regularize ECG QRS duration (QRSd) and significantly enhance the correlation between QRSd and CRT response. The 3 ML algorithms in a total of 38 features combinations constantly recognized that the features combined with QRSd/RWT outperformed the combinations without it. For each of three algorithms, the triplet feature combination of QRSd/RWT, LBBB, and nonischemic cardiomyopathy repeatedly increased the classification rate more than 8%. The best performance for CRT response prediction occurred with SVM model, which proposed actual QRSd/RWT values that favored CRT responses in patients both with and without LBBB. Lower QRSd/RWT values were required for CRT responses in patients with ischemic cardiomyopathy compared to those with non-ischemic cardiomyopathy. ML from ventricular remodeling characteristics–regularized QRSd improves CRT response prediction.



Similar content being viewed by others
References
Goldenberg I, Kutyifa V, Klein HU et al (2014) Survival with cardiac-resynchronization therapy in mild heart failure. N Engl J Med 370:1694–1701. https://doi.org/10.1056/NEJMoa1401426
Hunt SA, (2005) ACC/AHA 2005 guideline update for the diagnosis and management of chronic heart failure in the adult: a report of the American College of Cardiology/American Heart Association task force on practice guidelines (writing committee to update the 2001 guidelines for the evaluation and management of heart failure). J Am Coll Cardiol 46:e1–e82. https://doi.org/10.1016/j.jacc.2005.08.022
Cleland JG, Freemantle N, Erdmann E et al (2012) Long-term mortality with cardiac resynchronization therapy in the cardiac resynchronization-heart failure (CARE-HF) trial. Eur J Heart Fail 14:628–634. https://doi.org/10.1093/eurjhf/hfs055
Manlucu J, Tang AS (2014) Whom should I refer in 2014 for cardiac resynchronization? Can J Cardiol 30:675–678. https://doi.org/10.1016/j.cjca.2014.03.019
Yancy CW, Jessup M, Bozkurt B et al (2013) 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association task force on practice guidelines. Circulation 128:1810–1852. https://doi.org/10.1161/CIR.0b013e31829e8807
Ponikowski P, Voors AA, Anker SD, et al (2016) 2016 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure: the task force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J 37:2129–2200. https://doi.org/10.1093/eurheartj/ehw128
Varma N, Manne M, Nguyen D et al (2014) Probability and magnitude of response to cardiac resynchronization therapy according to QRS duration and gender in nonischemic cardiomyopathy and LBBB. Heart Rhythm 11:1139–1147. https://doi.org/10.1016/j.hrthm.2014.04.001
Yancy CW, McMurray JJ (2013) ECG—still the best for selecting patients for CRT. N Engl J Med 369:1463–1464. https://doi.org/10.1056/NEJMe1310406
Bleeker GB, Schalij MJ, Molhoek SG et al (2004) Relationship between QRS duration and left ventricular dyssynchrony in patients with end-stage heart failure. J Cardiovasc Electrophysiol 15:544–549. https://doi.org/10.1046/j.1540-8167.2004.03604.x
Bishop CM (2006) Pattern recognition and machine learning (information science and statistics). Springer, New York
Obermeyer Z, Emanuel EJ (2016) Predicting the future—big data, machine learning, and clinical medicine. N Engl J Med 375:1216–1219. https://doi.org/10.1056/NEJMp1606181
Sengupta PP, Huang YM, Bansal M et al (2016) Cognitive machine-learning algorithm for cardiac imaging: a pilot study for differentiating constrictive pericarditis from restrictive cardiomyopathy. Circ Cardiovasc Imaging 9:e004330. https://doi.org/10.1161/CIRCIMAGING.115.004330
Ellenbogen KA, Huizar JF (2012) Foreseeing super-response to cardiac resynchronization therapy: a perspective for clinicians. J Am Coll Cardiol 59:2374–2377. https://doi.org/10.1016/j.jacc.2011.11.074
Felker GM, Shaw LK, O’Connor CM (2002) A standardized definition of ischemic cardiomyopathy for use in clinical research. J Am Coll Cardiol 39:210–218. https://doi.org/10.1016/S0735-1097(01)01738-7
Gold MR, Thebault C, Linde C et al (2012) The effect of QRS duration and morphology on cardiac resynchronization therapy outcomes in mild heart failure: results from the resynchronization Reverses remodeling in systolic left ventricular dysfunction (REVERSE) study. Circulation 126:822–829. https://doi.org/10.1161/CIRCULATIONAHA.112.097709
Wang YG, Wu HT, Daubechies I et al (2015) Automated J wave detection from digital 12-lead electrocardiogram. J Electrocardiol 48:21–28. https://doi.org/10.1016/j.jelectrocard.2014.10.006
Surawicz B, Childers R, Deal BJ et al (2009) AHA/ACCF/HRS recommendations for the standardization and interpretation of the electrocardiogram, part III: intraventricular conduction disturbances a scientific statement from the American Heart Association Electrocardiography and Arrhythmias Committee, Council on Clinical Cardiology; the American College of Cardiology Foundation; and the Heart Rhythm Society endorsed by the International Society for Computerized Electrocardiology. J Am Coll Cardiol 53:976–981. https://doi.org/10.1016/j.jacc.2008.12.013
Lang RM, Bierig M, Devereux RB et al (2005) Recommendations for chamber quantification: a report from the American Society of Echocardiography’s Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr 18:1440–1463. https://doi.org/10.1016/j.echo.2005.10.005
Biton Y, Goldenberg I, Kutyifa V et al (2016) Relative wall thickness and the risk for ventricular tachyarrhythmias in patients with left ventricular dysfunction. J Am Coll Cardiol 67:303–312. https://doi.org/10.1016/j.jacc.2015.10.076
Devereux RB, Alonso DR, Lutas EM et al (1986) Echocardiographic assessment of left ventricular hypertrophy: comparison to necropsy findings. Am J Cardiol 57:450–458. https://doi.org/10.1016/0002-9149(86)90771-X
Nagueh SF, Appleton CP, Gillebert TC et al (2009) Recommendations for the evaluation of left ventricular diastolic function by echocardiography. J Am Soc Echocardiogr 22:107–133. https://doi.org/10.1016/j.echo.2008.11.023
Lei J, Dhamoon AS, Wang JF et al (2016) Walking the tightrope: using quantitative Doppler echocardiography to optimize ventricular filling pressures in patients hospitalized for acute heart failure. Eur Heart J Acute Cardiovasc Care 5:130–140. https://doi.org/10.1177/2048872615573517
Lei J, Wang JF, Voelker R et al (2014) Developing integrated echocardiographic protocol to optimize cardiac resynchronization therapy with quadripolar lead. J Am Coll Cardiol 64 (16 Supplement): C159. https://doi.org/10.1016/j.jacc.2014.06.732
Jansen AH, Bracke FA, van Dantzig JM et al (2006) Correlation of echo-Doppler optimization of atrioventricular delay in cardiac resynchronization therapy with invasive hemodynamics in patients with heart failure secondary to ischemic or idiopathic dilated cardiomyopathy. Am J Cardiol 97:552–557. https://doi.org/10.1016/j.amjcard.2005.08.076
Cortes C, Vapnik V (1995) Support-vector networks. Mach Learn 20:273–297. https://doi.org/10.1007/BF00994018
Cover T, Hart P (1967) Nearest neighbor pattern classification. IEEE Trans Inf Theory 13:21–27. https://doi.org/10.1109/tit.1967.1053964
Ho TK (1998) The random subspace method for constructing decision forests. IEEE Trans Pattern Anal Mach Intell 20:832–844. https://doi.org/10.1109/34.709601
Gaasch WH, Zile MR (2011) Left ventricular structural remodeling in health and disease: with special emphasis on volume, mass, and geometry. J Am Coll Cardiol 58:1733–1740. https://doi.org/10.1016/j.jacc.2011.07.022
Zhang Q, Fung JW, Auricchio A et al (2006) Differential change in left ventricular mass and regional wall thickness after cardiac resynchronization therapy for heart failure. Eur Heart J 27:1423–1430. https://doi.org/10.1093/eurheartj/ehi885
Chan DD, Wu KC, Loring Z et al (2014) Comparison of the relation between left ventricular anatomy and QRS duration in patients with cardiomyopathy with versus without left bundle branch block. Am J Cardiol 113:1717–1722. https://doi.org/10.1016/j.amjcard.2014.02.026
Draper TS Jr, Silver JS, Gaasch WH (2015) Adverse structural remodeling of the left ventricle and ventricular arrhythmias in patients with depressed ejection fraction. J Card Fail 21:97–102. https://doi.org/10.1016/j.cardfail.2014.10.018
Gasparini M, Galimberti P (2013) Device therapy in heart failure: has CRT changed “the sickest benefit the most” to “the healthiest benefit the most?”. J Am Coll Cardiol 61:945–947. https://doi.org/10.1016/j.jacc.2012.11.048
Adelstein EC, Saba S (2007) Scar burden by myocardial perfusion imaging predicts echocardiographic response to cardiac resynchronization therapy in ischemic cardiomyopathy. Am Heart J 153:105–112. https://doi.org/10.1016/j.ahj.2006.10.015
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors report no conflicts of interest in this study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
Supplemental methods
For SVM, radial kernel was used. Mahalanobis distance was used in KNN. For all of the three methods, cross-validation was applied to choose appropriate values of the parameters.
Cross-validation, a well-known model/parameter selection technique, was performed to select appropriate parameters and estimate the test classification error. More specifically, we randomly split the whole data into ten subsets. For each experiment, nine of subsets were used as training data and the remaining one was used as test data. In other words, the features and the corresponding labels of training data were used to learn the model and then this model was applied to the features of test data to predict the response. The predicted labels were then compared with the ground truth to compute the test classification rate. The subset for testing is then permuted and ten experiments are carried out. The report classification rate is the average over ten experiments.
The advantage of cross-validation is twofold. First, the best model and parameter can be determined using the training data. Second, there was no overlap between the training and test data, and the ground-truth labels of the test data were not used for predicting the labels. Therefore, the test classification rate computed through the above procedure was a good measure about how well the model performs on further unseen data. Furthermore, the data are split at random and the subset for testing is permuted. It is well known that the variation in the averaged test classification rate is small.
Rights and permissions
About this article
Cite this article
Lei, J., Wang, Y.G., Bhatta, L. et al. Ventricular geometry–regularized QRSd predicts cardiac resynchronization therapy response: machine learning from crosstalk between electrocardiography and echocardiography. Int J Cardiovasc Imaging 35, 1221–1229 (2019). https://doi.org/10.1007/s10554-019-01545-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-019-01545-5