Abstract
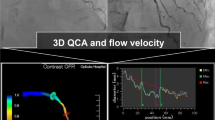
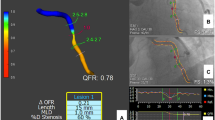
To assess a novel approach for automatic flow velocity computation in deriving quantitative flow ratio (QFR) from coronary angiography. QFR is a novel approach for assessment of functional significance of coronary artery stenosis without using pressure wire and induced hyperemia. Patient-specific coronary flow is estimated semi-automatically by frame count method, which is subjective and inconvenient in the workflow of QFR analysis. The vascular structures were automatically delineated from coronary angiogram. Subsequently, the centerline of the interrogated vessel was extracted from the delineated lumen on each image frame and the change in the length of centerline was used to compute the flow velocity, which provided patient-specific flow for computation of QFR (QFRauto). A parameter derived from the increase in centerline length was used to automatically quantify the stability of contrast flow. From the two angiographic image runs used for three-dimensional angiographic reconstruction, the one with better stability was used to compute QFRauto. QFRauto was assessed in all patients enrolled in the FAVOR II China study, and compared with the commercialized QFR computational method based on frame count (QFRcount), using pressure wire-based fractional flow reserve (FFR) as the reference standard. Out of 328 vessels with paired FFR data, QFRauto was successfully computed on 325 (99%) vessels with acceptable stability in filling of contrast flow. The flow velocity computed by the proposed approach had a weak to moderate correlation with the frame count method (r = 0.37, p < 0.001), with mean differences of − 0.02 ± 0.07 m/s (p < 0.001). QFRauto had good correlation (r = 0.96, p < 0.001) and agreement (mean difference: − 0.01 ± 0.04, p < 0.001) with QFRcount. Good correlation (r = 0.83, p < 0.001) and agreement (mean difference: 0.01 ± 0.06, p = 0.016) were also observed between QFRauto and FFR. Using FFR ≤ 0.80 to define functional significance of coronary stenosis, the overall diagnostic accuracy for QFRauto was 93.2% (95% CI 90.5–96.0%). The area under the receiver-operating characteristic curve did not differ significantly between QFRcount and QFRauto (difference: 0.00; 95% CI − 0.01 to 0.01; p = 0.529). Sensitivity, specificity, positive likelihood ratio, and negative likelihood ratio for QFRauto were 92.4% (95% CI 86.0–96.5%), 93.7% (95% CI 89.5–96.6%), 14.7 (95% CI 8.7–25.0), and 0.1 (95% CI 0.0–0.2), respectively. Automatic computation of patient-specific coronary flow velocity based on coronary angiography is feasible. Assessment of QFR based on this novel approach had good diagnostic accuracy in determining the functional significance of coronary stenosis.






Similar content being viewed by others
Abbreviations
- AUC:
-
Areas under the receiver-operator characteristics curve
- CI:
-
Confidence interval
- FFR:
-
Fractional flow reserve
- LAD:
-
Left anterior descending
- QFR:
-
Quantitative flow velocity
- QFRauto :
-
QFR computed by Vauto
- QFRcount :
-
QFR computed by Vcount
- RCA:
-
Right coronary artery
- Vauto :
-
Automatically calculated flow velocity
- Vcount :
-
Frame count-based flow velocity
References
De Bruyne B, Pijls NHJ, Kalesan B et al (2012) Fractional flow reserve–guided PCI versus medical therapy in stable coronary disease. N Engl J Med 367(11):991–1001
Tonino PAL, De Bruyne B, Pijls NHJ et al (2009) Fractional flow reserve versus angiography for guiding percutaneous coronary intervention. N Engl J Med 360(3):213–224
Johnson NP, Tóth GG, Lai D et al (2014) Prognostic value of fractional flow reserve: linking physiologic severity to clinical outcomes. J Am Coll Cardiol 64(16):1641–1654
Berry C, Corcoran D, Hennigan B et al (2015) Fractional flow reserve-guided management in stable coronary disease and acute myocardial infarction: recent developments. Eur Heart J 36(45):3155–3164
Fearon WF (2014) Percutaneous coronary intervention should be guided by fractional flow reserve measurement response to Fearon. Circulation 129(18):1860–1870
Tu S, Westra J, Yang J et al (2016) Diagnostic accuracy of fast computational approaches to derive fractional flow reserve from diagnostic coronary angiography: the international multicenter FAVOR pilot study. JACC Cardiovasc Interv 9(19):2024–2035
Tu S, Barbato E, Köszegi Z et al (2014) Fractional flow reserve calculation from 3-dimensional quantitative coronary angiography and TIMI frame count: a fast computer model to quantify the functional significance of moderately obstructed coronary arteries. JACC Cardiovasc Interv 7(7):768
Xu B, Tu S, Qiao S et al (2017) Diagnostic accuracy of angiography-based quantitative flow ratio measurements for online assessment of coronary stenosis. J Am Coll Cardiol 70(25):3077–3087
Westra J, Tu S, Winther S et al (2018) Evaluation of coronary artery stenosis by quantitative flow ratio during invasive coronary angiography: the WIFI II study (wire-free functional imaging II). Circ Cardiovasc Imaging 11(3):e007107
Westra J, Andersen BK, Campo G et al (2018) Diagnostic performance of in-procedure angiography-derived quantitative flow reserve compared to pressure-derived fractional flow reserve: the FAVOR II Europe-Japan Study. J Am Heart Assoc Cardiovas Cerebrovasc Dis 7(14):e009603
Perona P, Malik J (2002) Scale-space and edge detection using anisotropic diffusion. IEEE Trans Pattern Anal Mach Intell 12(7):629–639
Jin Y, Fayad LM, Laine AF (2001) Contrast enhancement by multiscale adaptive histogram equalization. In: International symposium on optical science and technology. International society for optics and photonics
Prasad VSN, Domke J (2005) Gabor filter visualization. J Atmos Sci 13
Osher S, Sethian JA (1988) Fronts propagating with curvature-dependent speed: algorithms based on Hamilton-Jacobi formulations. J Comput Phys 79:12–49
Hassouna MS, Farag AA (2007) Multistencils fast marching methods: a highly accurate solution to the Eikonal equation on Cartesian domains. IEEE Trans Pattern Anal Mach Intell 29(9):1563–1574
Godunov SK (1959) A finite difference method for the numerical computation of discontinuous solutions of the equations of fluid dynamics. Matematicheskii Sbornik 47:357–393
Van Uitert R, Bitter I (2007) Subvoxel precise skeletons of volumetric data based on fast marching methods. Med Phys 34(2):627
Tu S, Hao P, Koning G et al (2011) In vivo assessment of optimal viewing angles from X-ray coronary angiography. Eurointervention 7(1):112
Toth G, Hamilos M, Pyxaras S et al (2014) Evolving concepts of angiogram: fractional flow reserve discordances in 4000 coronary stenoses. Eur Heart J 35(40):2831–2838
Tu S, Echavarria-Pinto M, Birgelen CV et al (2015) Fractional flow reserve and coronary bifurcation anatomy: a novel quantitative model to assess and report the stenosis severity of bifurcation lesions. JACC Cardiovasc Interv 8(4):564–574
Götberg M, Fröbert O (2017) Instantaneous wave-free ratio versus fractional flow reserve. N Engl J Med 377(16):1813–1823
Gould KL (1978) Pressure-flow characteristics of coronary stenoses in unsedated dogs at rest and during coronary vasodilation. Circ Res 43(2):242–253
Mejía-Rentería H, Lee JM, Lauri F et al (2018) Influence of microcirculatory dysfunction on angiography-based functional assessment of coronary stenoses. JACC Cardiovasc Interv 11(8):741–753
Funding
This study was supported by the National Key Research and Development Program of China (Grant No. 2016YFC0100500), the Natural Science Foundation of China (Grant No. 81871460 and 31500797), Shanghai ShenKang Hospital Development Center (16CR3034A), and Shanghai Jiao Tong University (Grant No. YG2015ZD04 and YG2016ZD09).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the Authors have declared a conflict of interest in relation to this study, with the exception that S Tu received research support from Medis medical imaging and Pulse medical imaging. Other authors report no conflicts of interest regarding this manuscript.
Rights and permissions
About this article
Cite this article
Zhang, Y., Zhang, S., Westra, J. et al. Automatic coronary blood flow computation: validation in quantitative flow ratio from coronary angiography. Int J Cardiovasc Imaging 35, 587–595 (2019). https://doi.org/10.1007/s10554-018-1506-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-018-1506-y