Abstract
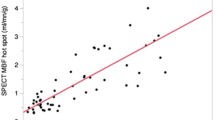
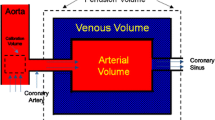
The purpose of this study was to develop a method for automatic and stable determination of the optimal time range for fitting with a Patlak plot model in order to measure myocardial perfusion using coronary X-ray angiography images. A conventional two-compartment model is used to measure perfusion, and the slope of the Patlak plot is calculated to obtain a perfusion image. The model holds for only a few seconds while the contrast agent flows from artery to myocardium. Therefore, a specific time range should be determined for fitting with the model. To determine this time range, automation is needed for routine examinations. The optimal time range was determined to minimize the standard error between data points and their least-squares regression straight line in the Patlak plot. A total of 28 datasets were tested in seven porcine models. The new method successfully detected the time range when contrast agent flowed from artery to myocardium. The mean cross correlation in the linear regression analysis (R2) was 0.996 ± 0.004. The mean length of the optimal time range was 3.61 ± 1.29 frames (2.18 ± 1.40 s). This newly developed method can automatically determine the optimal time range for fitting with the model.








Similar content being viewed by others
References
van’t Hof AWJ, Liem A, Suryapranata H et al (1998) Angiographic assessment of myocardial reperfusion in patients treated with primary angioplasty for acute myocardial infarction myocardial blush grade. Circulation 97:2302–2306. doi:10.1161/01.CIR.97.23.2302
Henriques JPS, Zijlstra F, van’t Hof AWJ et al (2003) Angiographic assessment of reperfusion in acute myocardial infarction by myocardial blush grade. Circulation 107:2115–2119. doi:10.1161/01.CIR.0000065221.06430.ED
Gibson CM, Cannon CP, Murphy SA et al (2000) Relationship of TIMI myocardial perfusion grade to mortality after administration of thrombolytic drugs. Circulation 101:125–130. doi:10.1161/01.CIR.101.2.125
Gibson CM, Schömig A (2004) Coronary and myocardial angiography: angiographic assessment of both epicardial and myocardial perfusion. Circulation 109:3096–3105. doi:10.1161/01.CIR.0000134278.50359.CB
Vogelzang M, Vlaar PJ, Svilaas T et al (2009) Computer-assisted myocardial blush quantification after percutaneous coronary angioplasty for acute myocardial infarction: a substudy from the TAPAS trial. Eur Heart J 30:594–599. doi:10.1093/eurheartj/ehn542
Cusma JT, Toggart EJ, Folts JD et al (1987) Digital subtraction angiographic imaging of coronary flow reserve. Circulation 75:461–472. doi:10.1161/01.CIR.75.2.461
Solzbach U, Liao J, Whiting JS, Eigler NL (1995) Digital angiographic impulse response analysis of myocardial perfusion: influence of heart rate and blood pressure changes on microcirculatory transit time measurement in the normal canine coronary circulation. Comput Biomed Res 28:371–392. doi:10.1006/cbmr.1995.1025
Schuhlen H, Eigler NL, Zeiher AM et al (1994) Digital angiographic assessment of the physiological changes to the regional microcirculation induced by successful coronary angioplasty. Circulation 90:163–171. doi:10.1161/01.CIR.90.1.163
Schühlen H, Eigler NL, Whiting JS (1994) Digital angiographic impulse response analysis of regional myocardial perfusion. Detection of autoregulatory changes in nonstenotic coronary arteries induced by collateral flow to adjacent stenotic arteries. Circulation 89:1004–1012. doi:10.1161/01.CIR.89.3.1004
Eigler NL, Schuhlen H, Whiting JS et al (1991) Digital angiographic impulse response analysis of regional myocardial perfusion. Estimation of coronary flow, flow reserve, and distribution volume by compartmental transit time measurement in a canine model. Circ Res 68:870–880. doi:10.1161/01.RES.68.3.870
Eigler NL, Pfaff JM, Zeiher A et al (1989) Digital angiographic impulse response analysis of regional myocardial perfusion: linearity, reproducibility, accuracy, and comparison with conventional indicator dilution curve parameters in phantom and canine models. Circ Res 64:853–866. doi:10.1161/01.RES.64.5.853
Gil D, Rodriguez-Leor O, Radeva P, Mauri J (2008) Myocardial perfusion characterization from contrast angiography spectral distribution. IEEE Trans Med Imaging 27:641–649. doi:10.1109/TMI.2007.912814
Sakaguchi T, Ichihara T, Trost JC et al (2014) Development of a theory for generating regional cardiac perfusion images during coronary angiography in the coronary angiography lab. Int J Cardiovasc Imaging 30:9–19. doi:10.1007/s10554-013-0304-9
Ichihara T, George RT, Silva C et al (2011) Quantitative analysis of first-pass contrast-enhanced myocardial perfusion multidetector CT using a Patlak plot method and extraction fraction correction during adenosine stress. IEEE Trans Nucl Sci 58:133–138. doi:10.1109/TNS.2010.2084104
Ichihara T, George RT, Lima JAC et al (2010) Evaluation of equivalence of upslope method-derived myocardial perfusion index and transfer constant based on two-compartment tracer kinetic model. IEEE Nucl Sci Symp Med Imaging Conf Rec. doi:10.1109/NSSMIC.2010.5874200
Vallée J-PM, Sostman HD, Macfall JR et al (1998) Quantification of myocardial perhsion by MRI after coronary occlusion. Magn Reson Med 40:287–297. doi:10.1002/mrm.1910400215
Ichihara T, Ishida M, Kitagawa K et al (2009) Quantitative analysis of first-pass contrast-enhanced myocardial perfusion MRI using a Patlak plot method and blood saturation correction. Magn Reson Med 62:373–383. doi:10.1002/mrm.22018
Kety SS (1951) The theory and applications of the exchange of inert gas at the lungs and tissues. Pharmacol Rev 3:1–41
Patlak CS, Blasberg RG, Fenstermacher JD (1983) Graphical evaluation of blood-to-brain transfer constants from multiple-time uptake data. J Cereb Blood Flow Metab 3:1–7. doi:10.1038/jcbfm.1983.1
Yao J, Sakaguchi T, Yousuf O et al (2012) Linear quantification correction for myocardial perfusion imaging from X-ray coronary angiography. IEEE Nucl Sci Symp Med Imaging Conf Rec. doi:10.1109/NSSMIC.2012.6551680
Hackstein N, Wiegand C, Rau WS, Langheinrich AC (2004) Glomerular filtration rate measured by using triphasic helical CT with a two-point Patlak plot technique. Radiology 230:221–226. doi:10.1148/radiol.2301021266
Jerosch-Herold M, Hu X, Murthy NS et al (2003) Magnetic resonance imaging of myocardial contrast enhancement with MS-325 and its relation to myocardial blood flow and the perfusion reserve. J Magn Reson Imaging 18:544–554. doi:10.1002/jmri.10384
Axel L (1983) Tissue mean transit time from dynamic computed tomography by a simple deconvolution technique. Invest Radiol 18:94–99. doi:10.1097/00004424-198301000-00018
Acknowledgments
The authors would like to thank Mr. Ryoichi Nagae for measuring the calculation times and Dr. Tohru Yagi for his valuable comments.
Conflict of interest
T. Sakaguchi is an employee of Toshiba Medical Systems Corporation. T. Ichihara has received research grant support from Toshiba Medical Systems Corporation. T. Natsume declares that he has no conflict of interest. J. Yao is an employee of Toshiba Medical Research Institute USA. O. Yousuf declares that he has no conflict of interest. J.C. Trost declares that he has no conflict of interest. J.A.C. Lima, has received research grant support from Toshiba Medical Systems Corporation. R.T. George has received research grant support from Toshiba Medical Systems Corporation, Astellas Pharma, and GE Healthcare, and has consulted for ICON Medical Imaging.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sakaguchi, T., Ichihara, T., Natsume, T. et al. Development of a method for automated and stable myocardial perfusion measurement using coronary X-ray angiography images. Int J Cardiovasc Imaging 31, 905–914 (2015). https://doi.org/10.1007/s10554-015-0658-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-015-0658-2