Abstract
Purpose
Obesity and smoking have been associated with poor prostate cancer (PC) outcomes. We investigated associations between obesity and biochemical recurrence (BCR), metastasis, castrate resistant-PC (CRPC), PC-specific mortality (PCSM), and all-cause mortality (ACM) and examined if smoking modified these associations.
Methods
We analyzed SEARCH Cohort data from men undergoing RP between 1990 and 2020. Cox regression models were used to estimate hazard ratios (HRs) and 95% confidence intervals (CIs) for associations between body mass index (BMI) as a continuous variable and weight status classifications (normal: 18.5 ≤ 25 kg/m2; overweight: 25–29.9 kg/m2; obese: ≥ 30 kg/m2) and PC outcomes.
Results
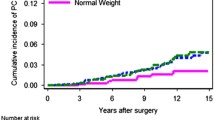
Among 6,241 men, 1,326 (21%) were normal weight, 2,756 (44%) overweight and 2159 (35%) obese; 1,841 (30%) were never-smokers, 2,768 (44%) former and 1,632 (26%) current-smokers. Among all men, obesity was associated with non-significant increased risk of PCSM, adj-HR = 1.71; 0.98–2.98, P = 0.057, while overweight and obesity were inversely associated with ACM, adj-HR = 0.75; 0.66–0.84, P < 0.001 and adj-HR = 0.86; 0.75–0.99, P = 0.033, respectively. Other associations were null. BCR and ACM were stratified for smoking status given evidence for interactions (P = 0.048 and P = 0.054, respectively). Among current-smokers, overweight was associated with an increase in BCR (adj-HR = 1.30; 1.07–1.60, P = 0.011) and a decrease in ACM (adj-HR = 0.70; 0.58–0.84, P < 0.001). Among never-smokers, BMI (continuous) was associated with an increase in ACM (adj-HR = 1.03; 1.00–1.06, P = 0.033).
Conclusions
While our results are consistent with obesity as a risk factor for PCSM, we present evidence of effect modification by smoking for BCR and ACM highlighting the importance of stratifying by smoking status to better understand associations with body weight.

Similar content being viewed by others
Data availability
Data are available upon request within VA rules and policy requirements.
References
American Cancer Society (2022) https://www.cancer.org/cancer/prostate-cancer/about/key-statistics.html/. Accessed 3 Aug, 2022
Siegel RL, Miller KD, Wagle NS, Jemal A (2023) Cancer statistics, 2023. CA Cancer J Clinic 73:17–48. https://doi.org/10.3322/caac.21763.
Pernar CH, Ebot EM, Wilson KM, Mucci LA (2018) The epidemiology of prostate cancer. Cold Spring Harbor Perspect Med 8:a030361. https://doi.org/10.1101/cshperspect.a030361
Peisch SF, Van Blarigan EL, Chan JM, Stampfer MJ, Kenfield SA (2017) Prostate cancer progression and mortality: a review of diet and lifestyle factors. World J Urol 35:867–874. https://doi.org/10.1007/s00345-016-1914-3
American Institute for Cancer Research (2020) The continuous update project—prostate cancer. https://www.aicr.org/research/the-continuous-update-project/prostate-cancer/. Accessed 31 May 2023
World Health Organization (2021) Obesity and overweight. https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight. Accessed 31 May 2023
Ward ZJ, Bleich SN, Cradock AL et al (2019) Projected U.S. state-level prevalence of adult obesity and severe obesity. N Engl J Med 381:2440–2450. https://doi.org/10.1056/nejmsa1909301
Centers for Disease Control and Prevention (2020) Current cigarette smoking among adults in the United States. https://www.cdc.gov/tobacco/data_statistics/fact_sheets/adult_data/cig_smoking/index.htm. Accessed 31 May 2023
Centers for Disease Control and Prevention (2020) Smoking & tobacco use. https://www.cdc.gov/tobacco/data_statistics/fact_sheets/fast_facts/index.htm. Accessed 31 May 2023
Langlais CS, Graff RE, Van Blarigan EL et al (2021) Post-diagnostic dietary and lifestyle factors and prostate cancer recurrence, progression, and mortality. Curr Oncol Rep. https://doi.org/10.1007/s11912-021-01017-x
Zhang X, Zhou G, Sun B et al (2015) Impact of obesity upon prostate cancer-associated mortality: a meta-analysis of 17 cohort studies. Oncol Lett 9:1307–1312. https://doi.org/10.3892/ol.2014.2841
Luo R, Chen Y, Ran K, Jiang Q (2020) Effect of obesity on the prognosis and recurrence of prostate cancer after radical prostatectomy: a meta-analysis. Transl Androl Urol 9:2713–22. https://doi.org/10.21037/tau-20-1352
Vidal AC, Oyekunle T, Howard LE et al (2020) Obesity, race, and long-term prostate cancer outcomes. Cancer 126:3733–3741. https://doi.org/10.1002/cncr.32906
Vidal AC, Howard LE, Sun SX et al (2017) Obesity and prostate cancer-specific mortality after radical prostatectomy: results from the Shared Equal Access Regional Cancer Hospital (SEARCH) database. Prostate Cancer Prostatic Dis 20:72–78. https://doi.org/10.1038/pcan.2016.47
Amling CL, Riffenburgh RH, Sun L et al (2004) Pathologic variables and recurrence rates as related to obesity and race in men with prostate cancer undergoing radical prostatectomy. J Clin Oncol 22:439–445. https://doi.org/10.1200/JCO.2004.03.132
Chalfin HJ, Lee SB, Jeong BC et al (2014) Obesity and long-term survival after radical prostatectomy. J Urol 192:1100–1104. https://doi.org/10.1016/j.juro.2014.04.086
Siddiqui SA, Inman BA, Sengupta S et al (2006) Obesity and survival after radical prostatectomy: a 10-year prospective cohort study. Cancer 107:521–529. https://doi.org/10.1002/cncr.22030
Mallah KN, Diblasio CJ, Rhee AC, Scardino PT, Kattan MW (2005) Body mass index is weakly associated with, and not a helpful predictor of, disease progression in men with clinically localized prostate carcinoma treated with radical prostatectomy. Cancer 103:2030–2034. https://doi.org/10.1002/cncr.20991
Leal-García M, Canto P, Cárdenas-Cárdenas E, Feria-Bernal G, García-García E, Méndez JP (2020) Overweight and obesity in men with prostate cancer do not constitute risk factors for biochemical recurrence. Aging Male 23:1283–1288. https://doi.org/10.1080/13685538.2020.1764523
Tomaszewski JJ, Chen YF, Bertolet M, Ristau BT, Woldemichael E, Nelson JB (2013) Obesity is not associated with aggressive pathologic features or biochemical recurrence after radical prostatectomy. Urology 81:992–996. https://doi.org/10.1016/j.urology.2012.10.080
Schiffmann J, Karakiewicz PI, Rink M et al (2018) Obesity paradox in prostate cancer: increased body mass index was associated with decreased risk of metastases after surgery in 13,667 patients. World J Urol 36:1067–1072. https://doi.org/10.1007/s00345-018-2240-8
Vidal AC, Howard LE, de Hoedt A et al (2018) Obese patients with castration-resistant prostate cancer may be at a lower risk of all-cause mortality: results from the Shared Equal Access Regional Cancer Hospital (SEARCH) database. BJU Int 122:76–82. https://doi.org/10.1111/bju.14193
Lee DH, Giovannucci EL (2019) The obesity paradox in cancer: epidemiologic insights and perspectives. Curr Nutr Rep 8:175–181. https://doi.org/10.1007/s13668-019-00280-6
Darcey E, Boyle T (2018) Tobacco smoking and survival after a prostate cancer diagnosis: a systematic review and meta-analysis. Cancer Treat Rev 70:30–40. https://doi.org/10.1016/j.ctrv.2018.07.001
Noor R, Perdana CAM, Umbas R, Agus Rizal AH, Hamid (2016) The risk factors of prostate cancer and its prevention: a literature review. Indones J Internal Med 48:11
De Nunzio C, Andriole GL, Thompson IM Jr, Freedland SJ (2015) Smoking and prostate cancer: a systematic review. Eur Urol Focus 1:28–38. https://doi.org/10.1016/j.euf.2014.10.002
Islami F, Moreira DM, Boffetta P, Freedland SJ (2014) A systematic review and meta-analysis of tobacco use and prostate cancer mortality and incidence in prospective cohort studies. Eur Urol 66:1054–1064. https://doi.org/10.1016/j.eururo.2014.08.059
Moreira DM, Nickel JC, Gerber L et al (2015) Smoking is associated with acute and chronic prostatic inflammation: results from the REDUCE Study. Cancer Prev Res (Phila) 8:312–317. https://doi.org/10.1158/1940-6207.Capr-14-0260
Moreira DM, Aronson WJ, Terris MK et al (2014) Cigarette smoking is associated with an increased risk of biochemical disease recurrence, metastasis, castration-resistant prostate cancer, and mortality after radical prostatectomy: results from the SEARCH database. Cancer 120:197–204. https://doi.org/10.1002/cncr.28423
Foerster B, Pozo C, Abufaraj M et al (2018) Association of smoking status with recurrence, metastasis, and mortality among patients with localized prostate cancer undergoing prostatectomy or radiotherapy: a systematic review and meta-analysis. JAMA Oncol 4:953–961. https://doi.org/10.1001/jamaoncol.2018.1071
Rieken M, Shariat SF, Kluth LA et al (2015) Association of cigarette smoking and smoking cessation with biochemical recurrence of prostate cancer in patients treated with radical prostatectomy. Eur Urol 68:949–956. https://doi.org/10.1016/j.eururo.2015.05.038
Song M, Giovannucci E (2016) Estimating the influence of obesity on cancer risk: stratification by smoking is critical. J Clin Oncol 34:3237–3239. https://doi.org/10.1200/jco.2016.67.6916
Berrington de Gonzalez A, Hartge P, Cerhan JR et al (2010) Body-mass index and mortality among 1.46 million white adults. N Engl J Med 363:2211–2219. https://doi.org/10.1056/NEJMoa1000367
Scher HI, Morris MJ, Stadler WM et al (2016) Trial design and objectives for castration-resistant prostate cancer: updated recommendations from the prostate cancer clinical trials working group 3. J Clin Oncol 34:1402–1418. https://doi.org/10.1200/jco.2015.64.2702
Xue X, Agalliu I, Kim MY et al (2017) New methods for estimating follow-up rates in cohort studies. BMC Med Res Methodol 17:155. https://doi.org/10.1186/s12874-017-0436-z
Banez LL, Hamilton RJ, Partin AW et al (2007) Obesity-related plasma hemodilution and PSA concentration among men with prostate cancer. JAMA 298:2275–2280. https://doi.org/10.1001/jama.298.19.2275
World Cancer Research Fund/American Institute for Cancer Research: Diet, nutrition, physical activity and cancer: a Global Perspective (2018) Continuous update project expert report: diet, nutrition, physical activity and prostate cancer. www.dietandcancerreport.org. Accessed July 3, 2022
Anderson AS, Martin RM, Renehan AG et al (2021) Cancer survivorship, excess body fatness and weight-loss intervention-where are we in 2020? Br J Cancer 124:1057–1065. https://doi.org/10.1038/s41416-020-01155-2
Audrain-Mcgovern J, Benowitz NL (2011) Cigarette smoking, nicotine, and body weight. Clin Pharmacol Ther 90:164–168. https://doi.org/10.1038/clpt.2011.105
Chiolero A, Jacot-Sadowski I, Faeh D, Paccaud F, Cornuz J (2007) Association of cigarettes smoked daily with obesity in a general adult population. Obesity (Silver Spring) 15:1311–1318. https://doi.org/10.1038/oby.2007.153
Chiolero A, Faeh D, Paccaud F, Cornuz J (2008) Consequences of smoking for body weight, body fat distribution, and insulin resistance. Am J Clin Nutr 87:801–809. https://doi.org/10.1093/ajcn/87.4.801
Dickerman BA, Ahearn TU, Giovannucci E et al (2017) Weight change, obesity and risk of prostate cancer progression among men with clinically localized prostate cancer. Int J Cancer 141:933–944. https://doi.org/10.1002/ijc.30803
Kelly SP, Lennon H, Sperrin M et al (2019) Body mass index trajectories across adulthood and smoking in relation to prostate cancer risks: the NIH-AARP Diet and Health Study. Int J Epidemiol 48:464–473. https://doi.org/10.1093/ije/dyy219
Chu DI, De Nunzio C, Gerber L et al (2011) Predictive value of digital rectal examination for prostate cancer detection is modified by obesity. Prostate Cancer Prostatic Dis 14:346–353. https://doi.org/10.1038/pcan.2011.31
Langlais CS, Cowan JE, Neuhaus J et al (2019) Obesity at diagnosis and prostate cancer prognosis and recurrence risk following primary treatment by radical prostatectomy. Cancer Epidemiol Biomark Prev 28:1917–1925. https://doi.org/10.1158/1055-9965.epi-19-0488
Nik-Ahd F, Howard LE, Aronson WJ et al (2020) Obese men undergoing radical prostatectomy: is robotic or retropubic better to limit positive surgical margins? Results from SEARCH. Int J Urol 27:851–857. https://doi.org/10.1111/iju.14307
Funding
No funding was received to assist with the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
ITL contributed to the writing of the original draft, review, and editing. LG contributed to the formal data analysis, interpretation, writing of the original draft, and review. AMH contributed to the data acquisition, writing and review, and project administration of the study. MRC, CLA, CJK, ZK, MKT, LGR, and WJA contributed to the data acquisition of the study. ACV contributed to the conceptualization, writing of the original draft, and review. SJF contributed to the acquisition of data, conceptualization, investigation, interpretation, writing of the original draft, review, and editing. IC contributed to the conceptualization, interpretation, methodology, supervision, writing of the original draft, review, and editing. All authors approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no potential conflict of interest that are relevant to the content of this article.
Ethical approval
This study was approved by the Durham VA IRB with waiver of informed consent and was conducted in accordance with recognized ethical guidelines (e.g., Declaration of Helsinki, CIOMS, Belmont Report, U.S. Common Rule).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Liu, I.T., Gu, L., De Hoedt, A.M. et al. Are associations between obesity and prostate cancer outcomes following radical prostatectomy the same in smokers and non-smokers? Results from the SEARCH Cohort. Cancer Causes Control 34, 983–993 (2023). https://doi.org/10.1007/s10552-023-01747-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-023-01747-2