Abstract
Purpose
Thyroid cancer incidence has increased over recent decades with considerable geographic variations in incidence patterns. Here, we analyzed temporal trends in the incidence and mortality rates of thyroid cancer in Taiwan.
Methods
We obtained age-standardized rates at a national level using data from the Taiwan Cancer Registry annual reports from 1995 to 2019. Trends in age-standardized rates were characterized by joinpoint regression analysis.
Results
The age-standardized incidence rate of thyroid cancer increased from 3.00 per 100,000 person-years in 1995 to 15.46 per 100,000 person-years in 2019 (p < 0.001). Significant upward trends were observed in virtually all age groups, including adolescents and the geriatric population. The average annual percent changes were 7.97%, 2.60%, 2.77%, and 1.43% for papillary, follicular, medullary, and anaplastic thyroid cancers, respectively. The mortality rate from thyroid cancer decreased over time in women but remained stable in men.
Conclusion
The incidence rates of thyroid cancer have steadily increased across gender, age groups, and tumor types over the past two decades. Future studies are needed to investigate potential etiological factors other than overdiagnosis that may drive these trends.
Similar content being viewed by others
Introduction
Thyroid cancer is the most common endocrine malignancy worldwide. The majority of thyroid cancer is follicular-derived differentiated thyroid cancer, which includes papillary and follicular types of tumors. Differentiated thyroid cancer affects younger populations than most malignancies and has an excellent prognosis, while patients with undifferentiated (anaplastic) thyroid cancer have dismal outcomes with a mean survival of 6 months [1]. Additionally, medullary thyroid cancer is a neuroendocrine C-cell derived thyroid cancer, and some patients are associated with an inherited multiple endocrine neoplasia syndrome. Given the indolent clinical course of differentiated thyroid cancer, a substantial reservoir of incidental thyroid cancer has been shown in autopsy studies [2]. It has been argued that increased detection of latent incidental diseases leads to overdiagnosis of thyroid cancer.
Globally, thyroid cancer has increased in incidence rates in recent decades, largely as a result of new cases of papillary thyroid cancer [3]. Improvement in the resolution of diagnostic imaging and its increased use has driven an increase in the identification of thyroid nodules and small, low-risk cancers. Nonetheless, there are considerable geographic variations in the incidence rates and the impact of overdiagnosis [4]. Numerous factors, such as a country's social and economic development, insurance system, iodine supplementation, and environmental exposure to radiation and endocrine disruptors, may contribute to vast differences among countries. Studies have shown that counties with a high Human Development Index generally have higher incidence rates, whereas mortality rates were relatively similar across different settings [5, 6].
In Taiwan, universal National Health Insurance has been associated with a reduction in deaths considered amenable to health care [7]. Since Taiwan is currently excluded from the World Health Organization, there is a paucity of data from Taiwan on the epidemiological burden and trends. The aim of the present study was to assess the temporal trends in thyroid cancer incidence and mortality in Taiwan over a period of 25 years. We also investigated the incidence trends stratified by age group and tumor type.
Methods
Data source
The data used for the current analysis were obtained from the Taiwan Cancer Registry annual reports of the Health Promotion Administration, Ministry of Health and Welfare, Taiwan [8]. The Taiwan Cancer Registry is a nationwide population-based cancer registry system that was established by the Taiwan government in 1979 and annually publishes the incidence and mortality of all cancers [9]. Hospitals with 50 or more beds are required to report cases of newly diagnosed cancer to the central registry office. Multiple verification procedures have been applied to ensure completeness and accuracy, including duplicate checks, logic and consistency assessments, and trace-back linkage to profiles of death certificates, National Health Insurance catastrophic illnesses, and four cancer screening programs [10]. The crude rates were adjusted to the 2000 World Health Organization population standard to generate the age-standardized rates. All rates were reported per 100,000 person-years.
Cases of thyroid cancer were identified using the topography codes of the International Classification of Diseases for Oncology, Field Trial Edition (ICD-O-FT: T-193) or the International Classification of Diseases for Oncology, Third Edition (ICD-O-3: C73). Tumor type was classified according to ICD-O-3 morphology codes: papillary (8260/3, 8340/3, 8341/3, 8342/3, 8343/3, 8344/3, and 8350/3), follicular (8290/3, 8330/3, 8331/3, 8332/3, 8333/3, 8335/3, and 8339/3), medullary (8345/3, 8347/3, and 8510/3), and anaplastic (8020/3 and 8021/3). We analyzed the data up to 2019 to avoid the potential effects of the 2019 coronavirus disease (COVID-19) pandemic [11].
Statistical analysis
A joinpoint piecewise linear regression analysis was performed to identify the time points corresponding to significant changes and identify temporal trends in the age-standardized incidence and mortality rates [12]. The National Cancer Institute Joinpoint regression software version 4.9.1.0 was used for all analyses with default parameters. Average annual percent change (AAPC) was calculated as a summary measure of the trends for the overall period. A 95% confidence interval (95% CI) was obtained from the parametric method with 4499 permutations. The rate was deemed to have been increased if the AAPC estimation and the lower boundary of its 95% CI were both positive. In contrast, the rate was deemed to be in a downward trend if the AAPC estimation and the upper boundary of its 95% CI were both negative. Otherwise, the rate was deemed to be stable over time. For visual clarity, adaptive splines were used to demonstrate the continuous relationship between the calendar year and statistical data.
Results
Demographic characteristics
From 1995 to 2019, a total of 55,372 cases of newly diagnosed thyroid cancer were recorded in the Taiwan Cancer Registry, comprising 13,240 (24%) men and 42,132 (76%) women (Table 1). As shown in Fig. 1a, the age-standardized incidence rate of thyroid cancer increased from 3.00 per 100,000 person-years in 1995 to 15.46 per 100,000 person-years in 2019 (AAPC = 7.10%, 95% CI 6.13 to 8.07, p < 0.001). The upward trends were observed in both men (AAPC = 7.35%, 95% CI 6.92 to 7.79) and women (AAPC = 6.81%, 95% CI 5.80 to 7.83). The mean age at diagnosis of thyroid cancer was 48.7 years for men and 42.7 years for women in 1995, and the mean age at diagnosis rose to 50.7 years for men and 49.6 years for women in 2019. The median age of diagnosis increased over time (Fig. 1b). The AAPC for median age at diagnosis for thyroid cancer was 0.32% (95% CI 0.23 to 0.42) for men and 0.97% (95% CI 0.78 to 1.15) for women.
Temporal trends in a age-standardized incidence rates, b median age at diagnosis, c age-standardized mortality rates, and d mortality-to-incidence ratios of thyroid cancer in Taiwan, from 1995 to 2019. Solid lines represent restricted cubic splines (smoothed fits). AAPC average annual percent change
Incidence trends for thyroid cancer by age
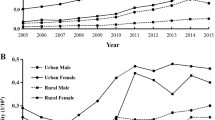
The age-standardized incidence rates of thyroid cancer by age group and sex are presented in Fig. 2. Those aged between 30 and 64 years accounted for the majority of thyroid cancer cases (74%). About 2% of thyroid cancers were diagnosed before 20 years of age, and 14% were diagnosed in those aged 65 years or older. In general, trends of increased thyroid cancer incidence were observed across all age groups, with the highest AAPCs occurring at ages between 30 and 64 years. It is noteworthy that the thyroid cancer incidence has also been increased in adolescents. The AAPC for age-standardized incidence rates was 2.70% (95% CI 0.85 to 4.59) for males aged 15 to 19 years and 4.16% (95% CI 2.57 to 5.78) for females. In addition, the incidence of thyroid cancer significantly increased in the 10–14 age group of females (AAPC = 2.98%, 95% CI 1.24 to 4.74).
Similar trends were observed in the geriatric population. For men, the incidence of thyroid cancer significantly increased in the 65–84 age group. The incidence rate was stable in men with a chronological age of 85 years or older (AAPC = − 1.25%, 95% CI − 3.98 to 1.55). For women, increased incidence rates were noted in subjects aged 65 years or older, with the exception of a marginal increase seen in those aged 80 to 84 years (AAPC = 1.01%, 95% CI − 0.17 to 2.19).
Incidence trends for thyroid cancer by tumor type
The incidence rates of different tumor types were further evaluated (Table 2). As shown in Fig. 3, papillary thyroid cancer showed the most drastic increase in incidence rates (AAPC = 7.97%, 95% CI 6.83 to 9.13). The AAPC for age-standardized incidence rates was 2.60% (95% CI 2.16 to 3.04) for follicular thyroid cancer and 2.77% (95% CI 1.33 to 4.24) for medullary thyroid cancer. Notably, the incidence rate of anaplastic thyroid cancer was 0.06 per 100,000 person-years in 1995 and rose to 0.11 per 100,000 person-years in 2019 with an AAPC of 1.43% (95% CI 0.30 to 2.57, p = 0.015).
Temporal trends in mortality
Overall, the mortality rates of thyroid cancer decreased over time (AAPC = − 1.28%, 95% CI − 1.88 to − 0.69, p < 0.001). In women, the mortality rate was 0.74 per 100,000 person-years in 1995 and dropped to 0.46 per 100,000 person-years in 2019 with an AAPC of − 1.73% (95% CI − 2.39 to − 1.06). However, the annual mortality rates of thyroid cancer did not change significantly in men (Fig. 1c). The mortality rate was 0.26 per 100,000 person-years in 1995 and became 0.36 per 100,000 person-years in 2019 with an AAPC of 0.39% (95% CI − 0.55 to 1.33).
We also calculated the mortality-to-incidence ratio (MIR), which has previously been employed as a proxy for survival [13]. Men generally had higher MIR values than women (Fig. 1d). The MIR of both sexes was 0.15 in 1995 and gradually decreased to 0.04 in 2019 with an AAPC of -5.43% (95% CI − 6.00 to − 4.85, p < 0.001).
Discussion
Consistent with global trends, we noted that the incidence rates of thyroid cancer have increased across gender, age groups, and tumor types over the past two decades. A previous analysis using the Taiwan Cancer Registry and the National Death Registry databases revealed that the age-standardized incidence of thyroid cancer increased from 5.66 per 100,000 person-years in 1997 to 12.30 per 100,000 person-years in 2012, with an AAPC of 5.1% (6.9% in males and 4.6% in females) [14]. The increase in incidence rates was most marked in papillary tumors and among middle-aged individuals. These findings suggest that Taiwan is no exception to the worldwide challenge of overdiagnosis of thyroid cancer.
Based on autopsy studies, the prevalence of subclinical papillary thyroid cancer is stable across the lifespan, and middle age does not confer a higher prevalence of subclinical disease compared to younger or older age groups [15]. Additionally, the prevalence of subclinical thyroid cancer has not increased over time [2]. Researchers from the Mayo Clinic reported that incidence rates of clinically relevant thyroid cancers, defined by histology, size, invasion, and metastasis, have not changed significantly in 80 years [16]. These observations indicate that increased incidence rates of thyroid cancer likely result from more diagnostic detection than a true population-level increase in tumorigenesis.
In the present study, it is noteworthy that increases in thyroid cancer incidence were observed in the pediatric as well as geriatric groups. Increased incidence rates of thyroid cancer in the pediatric population have been reported in other countries [17, 18]. Although one may argue that children and adolescents are less likely to have overdetection effects, the pattern of thyroid cancer incidence in children and adolescents mirrors the pattern seen in adults [19]. It is therefore postulated that overdiagnosis is also evident in the pediatric group. Nonetheless, in the United States, the incidence rates of large pediatric thyroid cancers (> 20 mm) increased from 1973 to 2013 [17]. It remains possible that a biologically real increase in incidence in the pediatric population exists and may stem from various factors, such as excess adiposity and exposure to medical radiation. Multiple or repeated exposures to dental X-rays were shown to be associated with an increased risk of thyroid cancer [20]. Warningly, its use in orthodontic practice has increased, especially in children and adolescents.
In line with trends in other countries [21], the rate of upsurge was lower in the geriatric group compared to the middle-aged population. Older patients, however, may be more vulnerable to treatment-related morbidities. Studies have indicated that thyroid cancer survivors have an increased risk of cerebrovascular disease and atrial fibrillation [22]. In Taiwan, cardiovascular disease is the third leading cause of mortality in thyroid cancer patients [23]. We recently demonstrated that, compared to the general population, thyroid cancer survivors have a substantial risk of coronary heart disease [24]. Some experts have proposed that surgical management of elderly patients with thyroid cancer should be tempered when high-risk findings (aggressive tumor type and metastasis) are absent, especially for those who have comorbid illnesses [25].
We found that the median age of diagnosis increased over time. In Korea, the age at diagnosis has also increased from 37.2 years before 1984 to 49.2 years after 2005 [26]. This may reflect a demographic shift and heightened overdiagnosis within the working age population. It is possible that employees will more readily access health care and regularly undergo annual health checkups as requested by the company. While declining birth rates and increased life expectancies create an aging population, retirement age is being delayed. In this regard, Taiwan has an accelerated rate of aging that is more than twice that of European countries and the United States [27]. A steeper rise in the age at diagnosis for women may imply advances in women's economic participation during the study period.
Iodine status influences the dominant tumor type of thyroid cancer, while endemic goiter and follicular thyroid cancer are more common in iodine-deficient areas. Mandatory salt iodization began in 1967 in Taiwan, and Taiwan's iodine policy changed from mandatory to voluntary salt iodization in 2003 [28]. As in other iodine-replete countries [5], we demonstrated that papillary thyroid cancer had a steeper increase in incidence rates than follicular thyroid cancer (AAPC 7.97% and 2.60%, respectively). Strikingly, our study disclosed that the incidence rates were also increased in medullary and anaplastic thyroid cancer (AAPC 2.77% and 1.43%, respectively).
It is acknowledged that the majority of anaplastic thyroid cancers develop through dedifferentiation from a preceding differentiated thyroid cancer [29]. Therefore, it is expected that the incidence of anaplastic cancer will decrease following the successful treatment of differentiated thyroid cancer [30]. Indeed, declining trends in anaplastic thyroid cancer rates were observed in most countries [31]. Our analysis points to an alarming increase in the incidence rates of anaplastic thyroid cancer with no joinpoints in Taiwan. This finding echoes a recent study exploring the Surveillance, Epidemiology, and End Results-18 cancer registry during 2000–2018, which reported an increase in anaplastic thyroid cancer with an AAPC of 1.99% in the United States [32]. The probability of a true rise in thyroid cancer burden needs careful attention as the increasing occurrence of anaplastic thyroid cancer is unlikely accounted for by overdiagnosis of small indolent tumors.
Medullary thyroid cancer originating from parafollicular neuroendocrine cells has a distinct pathobiology from follicular-derived thyroid cancer. In general, trends in the incidence of medullary thyroid cancer are not correlated with the corresponding trends in papillary and follicular thyroid cancer incidence [31]. In agreement with our observations, slight increases in incidence rates of medullary thyroid cancer have been reported in several countries, including the United States, Norway, and France [5, 32,33,34]. Interestingly, in Korea, when concerns of overdiagnosis were raised, decrements in thyroid cancer incidence were observed in not only papillary but also medullary thyroid cancer [35]. In this respect, it remains unclear whether there is a reservoir of subclinical medullary thyroid cancer, and whether the observed small increase in medullary thyroid cancer incidence is due in part to a more sensitive detection and diagnosis.
Thyroid cancer-specific mortality was the leading cause of death in patients with thyroid cancer in Taiwan, highlighting that cancer-related death remains a major health threat to thyroid cancer survivors [23]. International trends generally showed a decline in thyroid cancer mortality rates in both sexes [36]. Nonetheless, in the current study, we noted that the thyroid cancer mortality rate remained stable over time in male patients. In the United States, incidence-based mortality rates of thyroid cancer increased throughout 2000–2018 in both men and women, particularly for papillary and anaplastic carcinomas [32]. These reinforce the possibility that there might be actual increases in thyroid cancer burden in addition to medical scrutiny.
To date, biological causes of gender differences in thyroid cancer incidence are not yet well known. The autopsy prevalence of subclinical papillary thyroid cancer was similar between women and men [37]. The preconceived view regarding gender disparity may influence patterns in clinical thinking and health care utilization, leading to the risk of overdetection in women and the risk of underdetection in men [37]. Undoubtedly, other potential factors may contribute to the observed disparities, including hormonal and reproductive effects, obesity prevalence, smoking and dietary patterns, and occupational exposure to certain carcinogens. Male gender was independently associated with worse outcomes among patients with papillary thyroid cancer [38]. In-depth understanding of pathophysiology and continuously monitoring the trends in epidemiology of thyroid cancer are necessary to solve gender dilemmas.
The main strengths of this study are that we provided the most updated incidence and mortality rates of thyroid cancer in Taiwan based on high-quality cancer registries. The population-based design and the size of population coverage provided reliable estimates over the study period. Furthermore, we conducted joinpoint regression analyses to account for variation in trends over time rather than assuming a constant trend across all time periods. Nonetheless, several limitations need to be considered. We recognized the inherent limitations of retrospective analysis of a population-based database. Certain details, including patients' socioeconomic status and histologic characteristics, are not available. The MIR is not a useful or valid survival estimate [39]. Therefore, we were unable to calculate trends for survival, which would provide important insights into the extent of overdiagnosis. Second, the data source was from an East Asian country, which limits its generalizability to a more ethnically diverse population. Finally, given the descriptive nature of this study, the potential reasons for the observed incidence trends are largely conjectural.
Despite these limitations, our study sheds light on the clinical implications of thyroid cancer overdiagnosis in Taiwan. Accompanied with overdiagnosis, the potential harms and treatment-related adverse effects can be substantial. Diastolic dysfunction is frequently observed in asymptomatic long-term pediatric survivors of thyroid cancer [40]. Moreover, overdiagnosis turns normal subjects into patients and predisposes them to years of follow-up. Health-related quality of life is lower in young adults diagnosed with thyroid cancer, particularly when it comes to neuromuscular, concentration, and anxiety complaints [41]. In pediatric patients with differentiated thyroid cancer, disease-specific death is uncommon even in the presence of distant metastases [42]. Physical and psychological consequences associated with overdiagnosis may be more serious in children and adolescents. While the possibility of a true increase in disease burden is still debated, from a clinical perspective, physicians should avoid overutilization of medical imaging and should be discouraged from performing biopsies of low-risk nodules.
In conclusion, this large population-based study over a period of 25 years indicates that the overall incidence of thyroid cancer in Taiwan has been rising, consistently across all age groups and four major tumor types. Although the mortality rate from thyroid cancer in women has declined, death rates from thyroid cancer remain stable in men. Future etiological and molecular investigations are warranted to understand the underlying pathogenesis of the upward trend in the incidence of medullary and anaplastic thyroid cancer.
Data availability
The data that support the findings of this study were obtained from the openly available Cancer Registry System of the Health Promotion Administration, Ministry of Health and Welfare of Taiwan.
References
Cabanillas ME, McFadden DG, Durante C (2016) Thyroid cancer. Lancet 388(10061):2783–2795
Furuya-Kanamori L, Bell KJL, Clark J, Glasziou P, Doi SAR (2016) Prevalence of differentiated thyroid cancer in autopsy studies over six decades: a meta-analysis. J Clin Oncol 34(30):3672–3679
Wiltshire JJ, Drake TM, Uttley L, Balasubramanian SP (2016) Systematic review of trends in the incidence rates of thyroid cancer. Thyroid 26(11):1541–1552
Kim J, Gosnell JE, Roman SA (2020) Geographic influences in the global rise of thyroid cancer. Nat Rev Endocrinol 16(1):17–29
Kitahara CM, Sosa JA (2016) The changing incidence of thyroid cancer. Nat Rev Endocrinol 12(11):646–653
Pizzato M, Li M, Vignat J, Laversanne M, Singh D, La Vecchia C, Vaccarella S (2022) The epidemiological landscape of thyroid cancer worldwide: GLOBOCAN estimates for incidence and mortality rates in 2020. Lancet Diabetes Endocrinol 10(4):264–272
Lee YC, Huang YT, Tsai YW, Huang SM, Kuo KN, McKee M, Nolte E (2010) The impact of universal National Health Insurance on population health: the experience of Taiwan. BMC Health Serv Res 10:225
Health Promotion Administration, Ministry of Health and Welfare, Taiwan (2022) Cancer registry annual report. https://www.hpa.gov.tw/Pages/List.aspx?nodeid=269. Accessed November 2022
Chiang CJ, Wang YW, Lee WC (2019) Taiwan’s Nationwide cancer registry system of 40 years: past, present, and future. J Formos Med Assoc 118(5):856–858
Chiang CJ, You SL, Chen CJ, Yang YW, Lo WC, Lai MS (2015) Quality assessment and improvement of nationwide cancer registration system in Taiwan: a review. Jpn J Clin Oncol 45(3):291–296
Chung HP, Wu KL, Lin CY, Tang YH, Chen CH, Wu JC, Chen YT, Kuo KC, Chang WK (2022) Characteristics and outcomes of hospitalized geriatric patients with COVID-19 infection in Taiwan. Int J Gerontol 16(3):207–212
Kim HJ, Fay MP, Feuer EJ, Midthune DN (2000) Permutation tests for joinpoint regression with applications to cancer rates. Stat Med 19(3):335–351
Gajalakshmi CK, Shanta V, Rama R (1998) Registration of cancer mortality data in a developing area: Chennai (Madras, India) experience. Cancer Causes Control 9(2):131–136
Liu FC, Lin HT, Lin SF, Kuo CF, Chung TT, Yu HP (2017) Nationwide cohort study on the epidemiology and survival outcomes of thyroid cancer. Oncotarget 8(45):78429–78451
Arroyo N, Bell KJL, Hsiao V, Fernandes-Taylor S, Alagoz O, Zhang Y, Davies L, Francis DO (2022) Prevalence of subclinical papillary thyroid cancer by age: meta-analysis of autopsy studies. J Clin Endocrinol Metab 107(10):2945–2952
Genere N, El Kawkgi OM, Giblon RE, Vaccarella S, Morris JC, Hay ID, Brito JP (2021) Incidence of clinically relevant thyroid cancers remains stable for almost a century: a population-based study. Mayo Clin Proc 96(11):2823–2830
Qian ZJ, Jin MC, Meister KD, Megwalu UC (2019) Pediatric thyroid cancer incidence and mortality trends in the United States, 1973–2013. JAMA Otolaryngol Head Neck Surg 145(7):617–623
Lee YA, Yun HR, Lee J, Moon H, Shin CH, Kim SG, Park YJ (2021) Trends in pediatric thyroid cancer incidence, treatment, and clinical course in Korea during 2004–2016: a nationwide population-based study. Thyroid 31(6):902–911
Vaccarella S, Lortet-Tieulent J, Colombet M, Davies L, Stiller CA, Schuz J, Togawa K, Bray F, Franceschi S, Dal Maso L, Steliarova-Foucher E, IICC-3 contributors (2021) Global patterns and trends in incidence and mortality of thyroid cancer in children and adolescents: a population-based study. Lancet Diabetes Endocrinol 9(3):144–152
Memon A, Rogers I, Paudyal P, Sundin J (2019) Dental X-rays and the risk of thyroid cancer and meningioma: a systematic review and meta-analysis of current epidemiological evidence. Thyroid 29(11):1572–1593
Li M, Dal Maso L, Vaccarella S (2020) Global trends in thyroid cancer incidence and the impact of overdiagnosis. Lancet Diabetes Endocrinol 8(6):468–470
Tsai WH, Zeng YH, Lee CC, Chien MN, Liu SC, Chien KL, Cheng SP, Tseng PJ, Tsai MC (2023) Association between thyroid cancer and cardiovascular disease: a meta-analysis. Front Cardiovasc Med 10:1075844
Lu YL, Lin SF, Wu MH, Lee YY, Lee PW, Chang SH, Huang YT (2021) Survival and death causes in thyroid cancer in Taiwan: a nationwide case-control cohort study. Cancers 13(16):3955
Tsai MC, Hsieh CT, Hsu HY, Yeh TL, Lee WC, Chiang CJ, Hsiao BY, Jhuang JR, Tsai WH, Cheng SP, Chou CL, Lee CC, Liu SC, Tseng PJ, Chien KL (2022) Association between thyroid cancer and cardiovascular disease risk: a nationwide observation study. Sci Rep 12(1):18438
Wang Z, Vyas CM, Van Benschoten O, Nehs MA, Moore FD Jr, Marqusee E, Krane JF, Kim MI, Heller HT, Gawande AA, Frates MC, Doubilet PM, Doherty GM, Cho NL, Cibas ES, Benson CB, Barletta JA, Zavacki AM, Larsen PR, Alexander EK, Angell TE (2018) Quantitative analysis of the benefits and risk of thyroid nodule evaluation in patients ≥70 years old. Thyroid 28(4):465–471
Cho BY, Choi HS, Park YJ, Lim JA, Ahn HY, Lee EK, Kim KW, Yi KH, Chung JK, Youn YK, Cho NH, Park DJ, Koh CS (2013) Changes in the clinicopathological characteristics and outcomes of thyroid cancer in Korea over the past four decades. Thyroid 23(7):797–804
Lin YY, Huang CS (2016) Aging in Taiwan: building a society for active aging and aging in place. Gerontologist 56(2):176–183
Tang KT, Wang FF, Pan WH, Lin JD, Won GS, Chau WK, Lin HD, Hsieh YT (2016) Iodine status of adults in Taiwan 2005–2008, 5 years after the cessation of mandatory salt iodization. J Formos Med Assoc 115(8):645–651
Baloch ZW, Asa SL, Barletta JA, Ghossein RA, Juhlin CC, Jung CK, LiVolsi VA, Papotti MG, Sobrinho-Simoes M, Tallini G, Mete O (2022) Overview of the 2022 WHO classification of Thyroid neoplasms. Endocr Pathol 33(1):27–63
Albores-Saavedra J, Henson DE, Glazer E, Schwartz AM (2007) Changing patterns in the incidence and survival of thyroid cancer with follicular phenotype–papillary, follicular, and anaplastic: a morphological and epidemiological study. Endocr Pathol 18(1):1–7
Miranda-Filho A, Lortet-Tieulent J, Bray F, Cao B, Franceschi S, Vaccarella S, Dal Maso L (2021) Thyroid cancer incidence trends by histology in 25 countries: a population-based study. Lancet Diabetes Endocrinol 9(4):225–234
Megwalu UC, Moon PK (2022) Thyroid cancer incidence and mortality trends in the United States: 2000–2018. Thyroid 32(5):560–570
Opsahl EM, Akslen LA, Schlichting E, Aas T, Brauckhoff K, Hagen AI, Rosenlund AF, Sigstad E, Groholt KK, Maehle L, Engebretsen LF, Jorgensen LH, Varhaug JE, Bjoro T (2019) Trends in diagnostics, surgical treatment, and prognostic factors for outcomes in medullary thyroid carcinoma in Norway: a nationwide population-based study. Eur Thyroid J 8(1):31–40
Li M, Delafosse P, Meheus F, Borson-Chazot F, Lifante JC, Simon R, Groclaude P, Combes JD, Dal Maso L, Polazzi S, Duclos A, Colonna M, Vaccarella S (2021) Temporal and geographical variations of thyroid cancer incidence and mortality in France during 1986–2015: the impact of overdiagnosis. Cancer Epidemiol 75:102051
Oh CM, Lim J, Jung YS, Kim Y, Jung KW, Hong S, Won YJ (2021) Decreasing trends in thyroid cancer incidence in South Korea: What happened in South Korea? Cancer Med 10(12):4087–4096
James BC, Mitchell JM, Jeon HD, Vasilottos N, Grogan RH, Aschebrook-Kilfoy B (2018) An update in international trends in incidence rates of thyroid cancer, 1973–2007. Cancer Causes Control 29(4–5):465–473
LeClair K, Bell KJL, Furuya-Kanamori L, Doi SA, Francis DO, Davies L (2021) Evaluation of gender inequity in thyroid cancer diagnosis: differences by sex in US thyroid cancer incidence compared with a meta-analysis of subclinical thyroid cancer rates at autopsy. JAMA Intern Med 181(10):1351–1358
Su DH, Chang SH, Chang TC (2015) The impact of locoregional recurrences and distant metastases on the survival of patients with papillary thyroid carcinoma. Clin Endocrinol 82(2):286–294
Ellis L, Belot A, Rachet B, Coleman MP (2019) The mortality-to-incidence ratio is not a valid proxy for cancer survival. J Glob Oncol 5:1–9
Klein Hesselink MS, Bocca G, Hummel YM, Brouwers AH, Burgerhof JGM, van Dam EWCM, Gietema JA, Havekes B, van den Heuvel-Eibrink MM, Corssmit EPM, Kremer LCM, Netea-Maier RT, van der Pal HJH, Peeters RP, Plukker JTM, Ronckers CM, van Santen HM, van der Meer P, Links TP, Tissing WJE (2017) Diastolic dysfunction is common in survivors of pediatric differentiated thyroid carcinoma. Thyroid 27(12):1481–1489
Goldfarb M, Casillas J (2016) Thyroid cancer-specific quality of life and health-related quality of life in young adult thyroid cancer survivors. Thyroid 26(7):923–932
Nies M, Vassilopoulou-Sellin R, Bassett RL, Yedururi S, Zafereo ME, Cabanillas ME, Sherman SI, Links TP, Waguespack SG (2021) Distant metastases from childhood differentiated thyroid carcinoma: clinical course and mutational landscape. J Clin Endocrinol Metab 106(4):e1683–e1697
Funding
This work was supported by research grants (NSTC-110-2314-B-195-018-MY3) from the National Science and Technology Council of Taiwan and MacKay Memorial Hospital (MMH-11212). The funders had no involvement in the design, analysis, interpretation, or publishing of this manuscript.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Data collection and analysis were performed by SYHC and SPC. The first draft of the manuscript was written by SYHC and SPC. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interest
The authors have no relevant financial or non-financial interests to disclose.
Ethical approval
The conduct of this study was reviewed and approved by the Institutional Review Board of MacKay Memorial Hospital (Approval Number 22MMHIS345e).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Cheng, S.YH., Hsu, YC. & Cheng, SP. Trends in thyroid cancer burden in Taiwan over two decades. Cancer Causes Control 34, 553–561 (2023). https://doi.org/10.1007/s10552-023-01694-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-023-01694-y