Abstract
Purpose
It is unknown whether cancer treatment contributes more to long-term disease risk than lifestyle factors and comorbidities among B-cell non-Hodgkin lymphoma (B-NHL) survivors.
Methods
B-NHL survivors were identified in the Utah Cancer Registry from 1997 to 2015. Population attributable fractions (PAF) were calculated to assess the role of clinical and lifestyle factors for six cardiovascular, pulmonary, and renal diseases.
Results
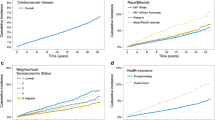
Cancer treatment contributed to 11% of heart and pulmonary conditions and 14.1% of chronic kidney disease. Charlson Comorbidity Index (CCI) at baseline contributed to all six diseases with a range of 9.9% of heart disease to 26.5% of chronic kidney disease. High BMI at baseline contributed to 18.4% of congestive heart failure and 7.9% of pneumonia, while smoking contributed to 4.8% of COPD risk.
Conclusion
Cancer treatment contributed more to heart disease, COPD, and chronic kidney disease than lifestyle factors and comorbidities among B-NHL survivors. High BMI at baseline contributed more to congestive heart failure and pneumonia than cancer treatment, whereas smoking at baseline was not a major contributor in this B-NHL survivor cohort. Baseline comorbidities consistently demonstrated high attributable risks for these diseases, demonstrating a strong association between preexisting comorbidities and aging-related disease risks.

Similar content being viewed by others
Data availability
The data that support the findings of this study are available with approval by the oversight committee for the Utah Population Database and IRB.
References
American Cancer Society (2019) Cancer treatment & survivorship facts & figures 2019–2021. American Cancer Society, Atlanta
Cohen JB, Kurtz DM, Staton AD, Flowers CR (2015) Next-generation surveillance strategies for patients with lymphoma. Future Oncol 11(13):1977–1991. https://doi.org/10.2217/fon.15.92
Salz T, Zabor EC, de Nully BP et al (2017) Pre-existing cardiovascular risk and subsequent heart failure among non-Hodgkin lymphoma survivors. J Clin Oncol 35(34):3837–3843. https://doi.org/10.1200/JCO.2017.72.4211
Moser EC, Noordijk EM, van Leeuwen FE et al (2006) Long-term risk of cardiovascular disease after treatment for aggressive non-Hodgkin lymphoma. Blood 107(7):2912–2919. https://doi.org/10.1182/blood-2005-08-3392
Ocier K, Abdelaziz S, Kim S et al (2021) Cardiovascular disease risks in younger versus older adult B-cell non-Hodgkin’s lymphoma survivors. Cancer Med 10(12):4117–4126. https://doi.org/10.1002/cam4.3934
Keefer K, Bender R, Liao J et al (2018) Characteristics of pulmonary complications in non-Hodgkin’s lymphoma patients treated with rituximab-containing chemotherapy and impact on survival. Ann Hematol 97(12):2373–2380. https://doi.org/10.1007/s00277-018-3448-9
Tichelli A, Rovó A, Gratwohl A (2008) Late pulmonary, cardiovascular, and renal complications after hematopoietic stem cell transplantation and recommended screening practices. Hematology Am Soc Hematol Educ Program 1:125–133. https://doi.org/10.1182/asheducation-2008.1.125
Afessa B, Litzow MR, Tefferi A (2001) Bronchiolitis obliterans and other late onset non-infectious pulmonary complications in hematopoietic stem cell transplantation. Bone Marrow Transplant 28:425–434
Yousem SA (1995) The histological spectrum of pulmonary graft-versus-host disease in bone marrow transplant recipients. Hum Pathol 26:668–675
Santo Tomas LH, Loberiza FR Jr, Klein JP et al (2005) Risk factors for bronchiolitis obliterans in allogeneic hematopoietic stem-cell transplantation for leukemia. Chest 128:153–161
Kersting S, Hene RJ, Koomans HA et al (2007) Chronic kidney disease after myeloablative allogeneic hematopoietic stem cell transplantation. Biol Blood Marrow Transplant 1:1169–1175
Delgado J, Cooper N, Thomson K et al (2006) The importance of age, fludarabine, and total body irradiation in the incidence and severity of chronic renal failure after allogeneic hematopoietic cell transplantation. Biol Blood Marrow Transplant 12:75–83
Hajder JMD, Stanisavljevic N, Mihaljevic B et al (2012) Biological and clinical features of non-Hodgkin’s lymphoma in the elderly. J BUON 17(4):753–760 (PubMed PMID: 23335537)
Whiteman DCWL (2016) The fractions of cancer attributable to modifiable factors: a global review. Cancer Epidemiol 44:203–221. https://doi.org/10.1016/j.canep.2016.06.013
Nicolaides CDS, Pavlidis N (1998) Prognostic factors in aggressive non-hodgkin’s lymphomas. Oncologist 3(3):189–197
Lees C, Keane C, Gandhi MK, Gunawardana J (2019) Biology and therapy of primary mediastinal B-cell lymphoma: current status and future directions. Br J Haematol 185(1):25–41. https://doi.org/10.1111/bjh.15778
Camicia R, Winkler HC, Hassa PO (2015) Novel drug targets for personalized precision medicine in relapsed/refractory diffuse large B-cell lymphoma: a comprehensive review. Mol Cancer 14:207. https://doi.org/10.1186/s12943-015-0474-2
Armitage JOGR, Lunning MA, Cavalli F (2017) Non-Hodgkin lymphoma. Lancet 390(10091):15–21. https://doi.org/10.1016/S0140-6736(16)32407-2
Madanat YF, Smith MR, Almasan A, Hill BT (2016) Idelalisib therapy of indolent B-cell malignancies: chronic lymphocytic leukemia and small lymphocytic or follicular lymphomas. Blood Lymphat Cancer 6:1–6. https://doi.org/10.2147/BLCTT.S73530
Gopal AK, Kahl BS, de Vos S et al (2014) PI3Kδ inhibition by idelalisib in patients with relapsed indolent lymphoma. N Engl J Med 370(11):1008–1018. https://doi.org/10.1056/NEJMoa1314583
Inamdar A, Goy A, Ayoub N et al (2016) Mantle cell lymphoma in the era of precision medicine-diagnosis, biomarkers and therapeutic agents. Oncotarget. https://doi.org/10.18632/oncotarget.8961
Ciobanu A, Stanca O, Triantafyllidis I, Lupu A (2013) Indolent lymphoma: diagnosis and prognosis in medical practice. Maedica (Buchar) 8(4):338–342
Thieblemont C, Molina T, Davi F (2016) Optimizing therapy for nodal marginal zone lymphoma. Blood 127(17):2064–2071. https://doi.org/10.1182/blood-2015-12-624296
The National Association of Health Data Organizations. Next Steps for the InterState Exchange of Nonresident Data Between State Health Data Organizations. Salt Lake City, Utah: The National Association of Health Data Organizations; 2009. https://www.nahdo.org/node/167
US Census Bureau. State-to-state migration flows. (2017). Retrieved from https://www.census.gov/data/tables/time-series/demo/geographic-mobility/ state-to-state-migration.html. Accessed Dec 2017.
Jaul E, Barron J (2017) Age-Related diseases and clinical and public health implications for the 85 years old and over population. Front Pub Health 5:335. https://doi.org/10.3389/fpubh.2017.00335
Liguori I, Russo G, Curcio F et al (2018) Oxidative stress, aging, and diseases. Clin Interv Aging 13:757–772. https://doi.org/10.2147/CIA.S158513
Shurin MR, Shurin GV, Chatta GS (2007) Aging and the dendritic cell system: implications for cancer. Crit Rev Oncol Hematol 64(2):90–105. https://doi.org/10.1016/j.critrevonc.2007.03.002
Armenian SH, Gibson CJ, Rockne RC et al (2019) Premature aging in young cancer survivors. J Natl Cancer Inst 111(3):226–232. https://doi.org/10.1093/jnci/djy229
Ocier K, Abdelaziz S, Kim S et al (2021) Age-Related Disease Risks in Younger versus Older B-Cell Non-Hodgkin's Lymphoma Survivors. Cancer Epidemiol Biomarkers Prev 30(12):2268–2277. https://doi.org/10.1158/1055-9965.EPI-21-0190
American Academy of Family Physicians. (2017). Tobacco: preventing and treating nicotine dependence and tobacco use. https://www.aafp.org/patient‐care/public‐health/tobacco‐nicotine/codingreference.html.
Rothman KJ, Lash TL (2020) Modern epidemiology, 4th edn. Lippincott Williams & Wilkins, Philadelphia, pp 263–286
Rockhill B, Newman B, Weinberg C (1998) Use and misuse of population attributable fractions. Am J Pub Health 88(1):15–19
Altman D, Machin D, Bryant T et al (2013) Statistics with confidence: confidence intervals and statistical guidelines, 2nd edn. Wiley, New York
Abid SH, Malhotra V, Perry MC (2001) Radiation-induced and chemotherapy-induced pulmonary injury. Curr Opin Oncol 13(4):242–248. https://doi.org/10.1097/00001622-200107000-00006
Wong R, Ofstedal MB, Yount K et al (2008) Unhealthy lifestyles among older adults: exploring transitions in Mexico and the US. Eur J Ageing 5(4):311–326. https://doi.org/10.1007/s10433-008-0098-0.PMID:25419206;PMCID:PMC4239542
Geyer SM, Morton LM, Habermann TM et al (2010) Smoking, alcohol use, obesity, and overall survival from non-hodgkin lymphoma: a population-based study. Cancer 116(12):2993–3000. https://doi.org/10.1002/cncr.25114
Kobayashi Y, Miura K, Hojo A et al (2011) Charlson comorbidity Index is an independent prognostic factor among elderly patients with diffuse large B-cell lymphoma. J Cancer Res Clin Oncol 137(7):1079–1084. https://doi.org/10.1007/s00432-010-0973-x
Lin T-L, Kuo M-C, Shih L-Y et al (2012) The impact of age, charlson comorbidity index, and performance status on treatment of elderly patients with diffuse large B cell lymphoma. Ann Hematol 91(9):1383–1391. https://doi.org/10.1007/s00277-012-1463-9
Drozd-Sokolowska J, Zaucha JM, Biecek P et al (2020) Type 2 diabetes mellitus compromises the survival of diffuse large B-cell lymphoma patients treated with (R)-CHOP—the PLRG report. Sci Rep 10(1):3517. https://doi.org/10.1038/s41598-020-60565-7
Acknowledgments
We also acknowledge partial support for the UPDB through grant P30 CA2014 from the National Cancer Institute, University of Utah, and from the University of Utah’s Program in Personalized Health and Center for Clinical and Translational Science. We thank the University of Utah Center for Clinical and Translational Science (CCTS) (funded by NIH Clinical and Translational Science Awards), the Pedigree and Population Resource, University of Utah Information Technology Services, and Biomedical Informatics Core for establishing the Master Subject Index between the Utah Population Database, the University of Utah Health Sciences Center and Intermountain Healthcare. The Utah Cancer Registry is funded by the National Cancer Institute’s SEER Program, Contract No. HHSN261201800016I, the US Centers for Disease Control and Prevention’s National Program of Cancer Registries, Cooperative Agreement No. NU58DP0063200, with additional support from the University of Utah and Huntsman Cancer Foundation. Partial support for all datasets within the Utah Population Database was provided by the University of Utah Huntsman Cancer Institute and the Huntsman Cancer Institute Cancer Center Support grant, P30 CA2014 from the National Cancer Institute
Funding
This work was supported by grants from the National Institutes of Health (NIH) (R21 CA185811, R03 CA159357, M. Hashibe, PI) and a National Center for Research Resources (NCRR) Grant (R01 RR021746, G. Mineau, PI) with additional support from the Utah Department of Health and the University of Utah. We thank the Pedigree and Population Resource of the Huntsman Cancer Institute, University of Utah (funded in part by the Huntsman Cancer Foundation) for its role in the ongoing collection, maintenance, and support of the Utah Population Database (UPDB).
Author information
Authors and Affiliations
Contributions
KO and MH conceived and designed the study. KO, CP, KS, JS, CL, and MH developed the methodology. KR, JS, VD, MN, AF, KS, and MH acquired the data. KO, SA, SK, and MH conducted data analysis and interpretation. KO, CP, KS, JS, CL, and MH drafted, reviewed, and revised the article. MN, AF, and MH constructed and organized the databases. MH supervised the entire study.
Corresponding author
Ethics declarations
Conflict of interest
No potential conflicts of interest were disclosed.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ocier, K., Abdelaziz, S., Kim, S. et al. Contributions of cancer treatment, comorbidities, and obesity to aging-related disease risks among non-Hodgkin lymphoma survivors. Cancer Causes Control 34, 171–180 (2023). https://doi.org/10.1007/s10552-022-01652-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-022-01652-0