Abstract
Purpose
The reasons behind socio-economic disparities in prostate cancer incidence remain unclear. We tested the hypothesis that individual-level factors act jointly with neighborhood-level social and built environment factors to influence prostate cancer risk and that specific social and built environment factors contribute to socio-econmic differences in risk.
Methods
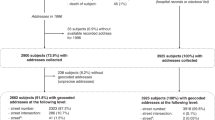
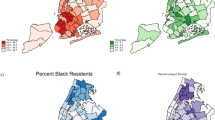
We used multi-level data, combining individual-level data (including education and known prostate cancer risk factors) for prostate cancer cases (n = 775) and controls (n = 542) from the San Francisco Bay Area Prostate Cancer Study, a population-based case–control study, with contextual-level data on neighborhood socio-economic status (nSES) and specific social and built environment factors from the California Neighborhoods Data System. Multivariable logistic regression models were used to compute adjusted odds ratios separately for localized and advanced stage prostate cancer while controlling for neighborhood clustering.
Results
We found a more than twofold increased risk of both localized and advanced prostate cancer with increasing levels of nSES, and decreased risk of advanced prostate cancer with increasing levels of education. For localized disease, the nSES association was largely explained by known prostate cancer risk factors and specific neighborhood environment factors; population density, crowding, and residential mobility. For advanced disease, associations with education and nSES were not fully explained by any available individual- or neighborhood-level factors.
Conclusions
These results demonstrate the importance of specific neighborhood social and built environment factors in understanding risk of localized prostate cancer. Further research is needed to understand the factors underpinning the associations between individual- and neighborhood-level SES and risk of advanced prostate cancer.
Similar content being viewed by others
References
American Cancer Society (2017) Cancer facts and figs (2017). American Cancer Society, Atlanta
Howlader N, Noone AM, Krapcho M, Miller DC, Bishop K, Altekruse S, CL. K, Yu M, Ruhl J, Tatalovich Z, Mariotto A, Lewis DR, Chen HS, Feuer EJ, Cronin KA SEER cancer statistics review, 1975–2013, National Cancer Institute. Bethesda, MD, http://seer.cancer.gov/csr/1975_2013/, based on November 2015 SEER data submission, posted to the SEER web site, April 2016
Hoffman RM, Gilliland FD, Eley JW, Harlan LC, Stephenson RA, Stanford JL, Albertson PC, Hamilton AS, Hunt WC, Potosky AL (2001) Racial and ethnic differences in advanced-stage prostate cancer: the Prostate Cancer Outcomes Study. J Natl Cancer Inst 93(5):388–395
Chornokur G, Dalton K, Borysova ME, Kumar NB (2011) Disparities at presentation, diagnosis, treatment, and survival in African American men, affected by prostate cancer. Prostate 71(9):985–997
Pudrovska T, Anishkin A (2015) Clarifying the positive association between education and prostate cancer: a Monte Carlo simulation approach. J Appl Gerontol 34(3):293–316
Sanderson M, Coker AL, Perez A, Du XL, Peltz G, Fadden MK (2006) A multilevel analysis of socioeconomic status and prostate cancer risk. Ann Epidemiol 16(12):901–907. https://doi.org/10.1016/j.annepidem.2006.02.006
Cheng I, Witte JS, McClure LA, Shema SJ, Cockburn MG, John EM, Clarke CA (2009) Socioeconomic status and prostate cancer incidence and mortality rates among the diverse population of California. Cancer Causes Control 20(8):1431–1440. https://doi.org/10.1007/s10552-009-9369-0
Hastert TA, Beresford SA, Sheppard L, White E (2015) Disparities in cancer incidence and mortality by area-level socioeconomic status: a multilevel analysis. J Epidemiol Community Health 69(2):168–176. https://doi.org/10.1136/jech-2014-204417
Yin D, Morris C, Allen M, Cress R, Bates J, Liu L (2010) Does socioeconomic disparity in cancer incidence vary across racial/ethnic groups? Cancer Causes Control 21(10):1721–1730. https://doi.org/10.1007/s10552-010-9601-y
Singh GK, Jemal A (2017) Socioeconomic and racial/ethnic disparities in cancer mortality, incidence, and survival in the United States, 1950–2014: over six decades of changing patterns and widening inequalities. J Environ Public Health. https://doi.org/10.1155/2017/2819372
Ward E, Jemal A, Cokkinides V, Singh GK, Cardinez C, Ghafoor A, Thun M (2004) Cancer disparities by race/ethnicity and socioeconomic status. CA Cancer J Clin 54(2):78–93
Oliver MN, Smith E, Siadaty M, Hauck FR, Pickle LW (2006) Spatial analysis of prostate cancer incidence and race in Virginia, 1990–1999. Am J Prev Med 30(2 Suppl):S67–S76. https://doi.org/10.1016/j.amepre.2005.09.008
Major JM, Norman Oliver M, Doubeni CA, Hollenbeck AR, Graubard BI, Sinha R (2012) Socioeconomic status, healthcare density, and risk of prostate cancer among African American and Caucasian men in a large prospective study. Cancer Causes Control 23(7):1185–1191. https://doi.org/10.1007/s10552-012-9988-8
Liu L, Cozen W, Bernstein L, Ross RK, Deapen D (2001) Changing relationship between socioeconomic status and prostate cancer incidence. J Natl Cancer Inst 93(9):705–709
Clegg LX, Reichman ME, Miller BA, Hankey BF, Singh GK, Lin YD, Goodman MT, Lynch CF, Schwartz SM, Chen VW, Bernstein L, Gomez SL, Graff JJ, Lin CC, Johnson NJ, Edwards BK (2009) Impact of socioeconomic status on cancer incidence and stage at diagnosis: selected findings from the surveillance, epidemiology, and end results: National Longitudinal Mortality Study. Cancer Causes Control 20(4):417–435. https://doi.org/10.1007/s10552-008-9256-0
Steenland K, Rodriguez C, Mondul A, Calle EE, Thun M (2004) Prostate cancer incidence and survival in relation to education (United States). Cancer Causes Control 15(9):939–945. https://doi.org/10.1007/s10552-004-2231-5
Shariff-Marco S, Yang J, John EM, Sangaramoorthy M, Hertz A, Koo J, Nelson DO, Schupp CW, Shema SJ, Cockburn M (2014) Impact of neighborhood and individual socioeconomic status on survival after breast cancer varies by race/ethnicity: the Neighborhood and Breast Cancer Study. Cancer Epidemiol Prev Biomark 23(5):793–811
Macintyre S, Ellaway A, Cummins S (2002) Place effects on health: how can we conceptualise, operationalise and measure them? Soc Sci Med 55(1):125–139
DeRouen MC, Schupp CW, Koo J, Yang J, Hertz A, Shariff-Marco S, Cockburn M, Nelson DO, Ingles SA, John EM (2018) Impact of individual and neighborhood factors on disparities in prostate cancer survival. Cancer Epidemiol 53:1–11
Gomez SL, Shariff-Marco S, DeRouen M, Keegan TH, Yen IH, Mujahid M, Satariano WA, Glaser SL (2015) The impact of neighborhood social and built environment factors across the cancer continuum: current research, methodological considerations, and future directions. Cancer 121(14):2314–2330. https://doi.org/10.1002/cncr.29345
Bostwick DG, Burke HB, Djakiew D, Euling S, Ho S, Landolph J, Morrison H, Sonawane B, Shifflett T, Waters DJ (2004) Human prostate cancer risk factors. Cancer 101(S10):2371–2490
Gomez SL, Glaser SL, McClure LA, Shema SJ, Kealey M, Keegan TH, Satariano WA (2011) The California Neighborhoods Data System: a new resource for examining the impact of neighborhood characteristics on cancer incidence and outcomes in populations. Cancer Causes Control 22(4):631–647
John EM, Schwartz GG, Koo J, Van Den Berg D, Ingles SA (2005) Sun exposure, vitamin D receptor gene polymorphisms, and risk of advanced prostate cancer. Cancer Res 65(12):5470–5479. https://doi.org/10.1158/0008-5472.CAN-04-3134
John EM, Stern MC, Sinha R, Koo J (2011) Meat consumption, cooking practices, meat mutagens, and risk of prostate cancer. Nutr Cancer 63(4):525–537. https://doi.org/10.1080/01635581.2011.539311
Semaphore Corporation (2011) ZP4: Address correction data and software. http://www.semaphorecorp.com/zp4/zp4.html
Goldberg DW (2009) The Texas A&M WebGIS Open Source Geocoding Platform. Technical Report No 11. University of South California GIS Research Laboratory, Los Angeles CA
ArcGIS. Version 10 (2011) Environmental Systems Research Institute, Inc.
Gomez SL, Glaser SL, McClure LA, Shema SJ, Kealey M, Keegan TH, Satariano WA (2011) The California Neighborhoods Data System: a new resource for examining the impact of neighborhood characteristics on cancer incidence and outcomes in populations. Cancer Causes Control 22(4):631–647. https://doi.org/10.1007/s10552-011-9736-5
Yost K, Perkins C, Cohen R, Morris C, Wright W (2001) Socioeconomic status and breast cancer incidence in California for different race/ethnic groups. Cancer Causes Control 12(8):703–711
Keegan TH, Hurley S, Goldberg D, Nelson DO, Reynolds P, Bernstein L, Horn-Ross PL, Gomez SL (2012) The association between neighborhood characteristics and body size and physical activity in the California teachers study cohort. Am J Public Health 102(4):689–697
Keegan TH, Shariff-Marco S, Sangaramoorthy M, Koo J, Hertz A, Schupp CW, Yang J, John EM, Gomez SL (2014) Neighborhood influences on recreational physical activity and survival after breast cancer. Cancer Causes Control 25(10):1295–1308. https://doi.org/10.1007/s10552-014-0431-1
Thornton LE, Pearce JR, Kavanagh AM (2011) Using Geographic Information Systems (GIS) to assess the role of the built environment in influencing obesity: a glossary. Int J Behav Nutr Phys Act 8(1):71
Robbins AS, Yin D, Parikh-Patel A (2007) Differences in prognostic factors and survival among White men and Black men with prostate cancer, California, 1995–2004. Am J Epidemiol 166(1):71–78. https://doi.org/10.1093/aje/kwm052
National Establishment Time-Series (NETS) Database 2009 (2008). Oakland, CA
California Department of Food and Agriculture (2010) California Certified Farmers’ Market Database
Shariff-Marco S, Gomez SL, Sangaramoorthy M, Yang J, Koo J, Hertz A, John EM, Cheng I, Keegan TH (2015) Impact of neighborhoods and body size on survival after breast cancer diagnosis. Health Place 36:162–172. https://doi.org/10.1016/j.healthplace.2015.10.003
Gunier RB, Hertz A, Von Behren J, Reynolds P (2003) Traffic density in California: socioeconomic and ethnic differences among potentially exposed children. J Expo Anal Environ Epidemiol 13(3):240–246. https://doi.org/10.1038/sj.jea.7500276
Baade PD, Yu XQ, Smith DP, Dunn J, Chambers SK (2015) Geographic disparities in prostate cancer outcomes–review of international patterns. Asian Pac J Cancer Prev 16(3):1259–1275
Baquet CR, Horm JW, Gibbs T, Greenwald P (1991) Socioeconomic factors and cancer incidence among blacks and whites. J Natl Cancer Inst 83(8):551–557
Meijer M, Bloomfield K, Engholm G (2013) Neighbourhoods matter too: the association between neighbourhood socioeconomic position, population density and breast, prostate and lung cancer incidence in Denmark between 2004 and 2008. J Epidemiol Community Health 67(1):6–13. https://doi.org/10.1136/jech-2011-200192
Obertova Z, Brown C, Holmes M, Lawrenson R (2012) Prostate cancer incidence and mortality in rural men—a systematic review of the literature. Rural Remote Health 12(2):2039
Blewett LA, Johnson PJ, Lee B, Scal PB (2008) When a usual source of care and usual provider matter: adult prevention and screening services. J Gen Intern Med 23(9):1354
Sarfaty M, Wender R, Smith R (2011) Promoting cancer screening within the patient centered medical home. CA Cancer J Clin 61(6):397–408. https://doi.org/10.3322/caac.20125
Ferrante JM, Balasubramanian BA, Hudson SV, Crabtree BF (2010) Principles of the patient-centered medical home and preventive services delivery. Ann Fam Med 8(2):108–116. https://doi.org/10.1370/afm.1080
Fisher ES (2008) Building a medical neighborhood for the medical home. N Engl J Med 359(12):1202–1205. https://doi.org/10.1056/NEJMp0806233
Zafar SY, Peppercorn JM, Schrag D, Taylor DH, Goetzinger AM, Zhong X, Abernethy AP (2013) The financial toxicity of cancer treatment: a pilot study assessing out-of-pocket expenses and the insured cancer patient’s experience. Oncologist 18(4):381–390
Krieger N, Chen JT, Waterman PD (2010) Decline in US breast cancer rates after the Women’s Health Initiative: socioeconomic and racial/ethnic differentials. Am J Public Health 100(Suppl 1):S132–S139. https://doi.org/10.2105/AJPH.2009.181628
Gomez SL, Hurley S, Canchola AJ, Keegan TH, Cheng I, Murphy JD, Clarke CA, Glaser SL, Martinez ME (2016) Effects of marital status and economic resources on survival after cancer: a population-based study. Cancer 122(10):1618–1625. https://doi.org/10.1002/cncr.29885
Acknowledgments
The authors thank Jennifer Jain for her help with manuscript preparation.
Funding
This work was supported by Grant W81XWH-10-1-0374 (SLG) from the United States Army Medical Research and Material Command. Data collection for the parent study was funded by Grants 864A-8702-S3514 and 99-00527V-10182 (EMJ) from the Cancer Research Fund, under Interagency Agreement #97-12013 (University of California contract #98-0092-V) with the Department of Health Services Cancer Research Program. The collection of cancer incidence data used in this study was supported by the California Department of Public Health as part of the statewide cancer reporting program mandated by California Health and Safety Code Section 103885; the National Cancer Institute’s Surveillance, Epidemiology and End Results Program under contract HHSN261201000140C awarded to the Cancer Prevention Institute of California, contract HHSN261201000035C awarded to the University of Southern California, and contract HHSN261201000034C awarded to the Public Health Institute; and the Centers for Disease Control and Prevention’s National Program of Cancer Registries, under agreement U58DP003862-01 awarded to the California Department of Public Health. The ideas and opinions expressed herein are those of the author(s) and endorsement by the State of California, Department of Public Health the National Cancer Institute, and the Centers for Disease Control and Prevention or their Contractors and Subcontractors is not intended nor should be inferred.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
DeRouen, M.C., Schupp, C.W., Yang, J. et al. Impact of individual and neighborhood factors on socioeconomic disparities in localized and advanced prostate cancer risk. Cancer Causes Control 29, 951–966 (2018). https://doi.org/10.1007/s10552-018-1071-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-018-1071-7