Abstract
Purpose
In 2007, the World Cancer Research Fund (WCRF) and American Institute for Cancer Research (AICR) published eight recommendations regarding body weight, physical activity, and dietary behaviors aimed at reducing cancer incidence worldwide. In this paper, we assess whether meeting the WCRF/AICR recommendations is associated with lower colorectal cancer (CRC) incidence; evaluate whether particular recommendations are most strongly associated with lower CRC incidence; and assess whether associations differ by sex.
Methods
We operationalized six of the recommendations (related to body weight, physical activity, energy density, plant foods, red and processed meat, and alcohol) and examined their association with CRC incidence over 7.6 years of follow-up in the prospective VITamins And Lifestyle Study cohort. Participants included 66,920 adults aged 50–76 years at baseline (2000–2002) with no history of CRC and with complete data for the recommendations evaluated. Incident colorectal cancers (n = 546) were tracked through 2009.
Results
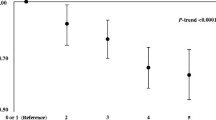
Compared with meeting no recommendations, meeting 1–3 recommendations was associated with 34–45 % lower CRC incidence, and meeting 4–6 was associated with 58 % lower incidence (95 % CI 34 %, 74 %) in fully adjusted analyses. The recommendations most strongly associated with lower CRC risk for women were related to body fatness and red and processed meat, while for men these were alcohol intake and red and processed meat. Differences by sex were statistically significant (p < 0.05) for the recommendations related to body weight and to alcohol.
Conclusions
Meeting the WCRF/AICR recommendations, particularly those related to alcohol, body weight, and red and processed meat, could substantially reduce CRC incidence; however, associations differ by sex.
Similar content being viewed by others
References
Marmot M, Atinmo T, Byers T et al (2007) Food, Nutrition, Physical Activity, and the Prevention of Cancer: a Global Perspective. World Cancer Research Fund/American Institute for Cancer Research, Washington
Romaguera D, Vergnaud A-C, Peeters PH et al (2012) Is concordance with World Cancer Research Fund/American Institute for Cancer Research guidelines for cancer prevention related to subsequent risk of cancer? Results from the EPIC study. Am J Clin Nutr 96:150–163. doi:10.3945/ajcn.111.031674
Hastert TA, Beresford SAA, Patterson RE et al (2013) Adherence to WCRF/AICR cancer prevention recommendations and risk of post-menopausal breast cancer. Cancer Epidemiol Biomarker Prev. doi:10.1158/1055-9965.EPI-13-0210
Lucas AL, Bravi F, Boffetta P et al (2016) Adherence to World Cancer Research Fund/American Institute for Cancer Research recommendations and pancreatic cancer risk. Cancer Epidemiol 40:15–21. doi:10.1016/j.canep.2015.10.026
Nomura SJO, Inoue-Choi M, Lazovich D, Robien K (2016) WCRF/AICR recommendation adherence and breast cancer incidence among postmenopausal women with and without non-modifiable risk factors. Int J Cancer n/a-n/a. doi:10.1002/ijc.29994
Hastert TA, Beresford SAA, Sheppard L, White E (2014) Adherence to the WCRF/AICR cancer prevention recommendations and cancer-specific mortality: results from the Vitamins and Lifestyle (VITAL) Study. Cancer Causes Control 25:541–552. doi:10.1007/s10552-014-0358-6
Vergnaud A-C, Romaguera D, Peeters PH et al (2013) Adherence to the World Cancer Research Fund/American Institute for Cancer Research guidelines and risk of death in Europe: results from the European Prospective Investigation into Nutrition and Cancer cohort study. Am J Clin Nutr 97:1107–1120. doi:10.3945/ajcn.112.049569
Cerhan JR, Potter JD, Gilmore JME et al (2004) Adherence to the AICR Cancer Prevention Recommendations and Subsequent Morbidity and Mortality in the Iowa Women’s Health Study Cohort. Cancer Epidemiol Biomarkers Prev 13:1114–1120
Inoue-Choi M, Robien K, Lazovich D (2013) Adherence to the WCRF/AICR Guidelines for Cancer Prevention Is Associated with Lower Mortality among Older Female Cancer Survivors. Cancer Epidemiol Biomarker Prev 22:792–802. doi:10.1158/1055-9965.EPI-13-0054
Nomura SJO, Dash C, Rosenberg L et al (2016) Is adherence to diet, physical activity, and body weight cancer prevention recommendations associated with colorectal cancer incidence in African American women? Cancer Causes Control 27:869–879. doi:10.1007/s10552-016-0760-3
Reedy J, Mitrou PN, Krebs-Smith SM et al (2008) Index-based Dietary Patterns and Risk of Colorectal Cancer The NIH-AARP Diet and Health Study. Am J Epidemiol 168:38–48. doi:10.1093/aje/kwn097
Reedy J, Wirfält E, Flood A et al (2010) Comparing 3 Dietary Pattern Methods—Cluster Analysis, Factor Analysis, and Index Analysis—With Colorectal Cancer Risk The NIH–AARP Diet and Health Study. Am J Epidemiol 171:479–487. doi:10.1093/aje/kwp393
White E, Patterson RE, Kristal AR et al (2004) VITamins And Lifestyle Cohort Study: study Design and Characteristics of Supplement Users. Am J Epidemiol 159:83–93. doi:10.1093/aje/kwh010
Schakel SF, Buzzard IM, Gebhardt SE (1997) Procedures for Estimating Nutrient Values for Food Composition Databases. J Food Compos Anal 10:102–114. doi:10.1006/jfca.1997.0527
Kristal AR, Vizenor NC, Patterson RE et al (2000) Precision and Bias of Food Frequency-based Measures of Fruit and Vegetable Intakes. Cancer Epidemiol Biomarker Prev 9:939–944
Thompson FE, Kipnis V, Midthune D et al (2008) Performance of a food-frequency questionnaire in the US NIH–AARP (National Institutes of Health-American Association of Retired Persons) Diet and Health Study. Public Health Nutr 11:183–195. doi:10.1017/S1368980007000419
Hu FB, Rimm E, Smith-Warner SA et al (1999) Reproducibility and validity of dietary patterns assessed with a food-frequency questionnaire. Am J Clin Nutr 69:243–249
Patterson RE, Kristal AR, Tinker LF et al (1999) Measurement characteristics of the Women’s Health Initiative food frequency questionnaire. Ann Epidemiol 9:178–187. doi:10.1016/S1047-2797(98)00055-6
Littman AJ, White E, Kristal AR et al (2004) Assessment of a one-page questionnaire on long-term recreational physical activity. Epidemiology 15:105–113
Kuczmarski MF, Kucszmarski RJ, Najjar M (2001) Effects of age on validity of self-reported height, weight, and body mass index: findings from the Third National Health and Nutrition Examination Survey, 1988–1994. J Am Diet Assoc 101:28–34. doi:10.1016/S0002-8223(01)00008-6
Obesity: Preventing and Managing the Global Epidemic (2000). World Health Organization
ICD Conversion Programs - SEER. http://seer.cancer.gov/tools/conversion/. Accessed 9 Feb 2016
Kirkegaard H, Johnsen NF, Christensen J et al (2010) Association of adherence to lifestyle recommendations and risk of colorectal cancer: a prospective Danish cohort study. BMJ 341:c5504. doi:10.1136/bmj.c5504
Wei EK, Colditz GA, Giovannucci EL et al (2009) Cumulative Risk of Colon Cancer up to Age 70 Years by Risk Factor Status Using Data From the Nurses’ Health Study. Am J Epidemiol 170:863–872. doi:10.1093/aje/kwp210
Platz EA, Willett WC, Colditz GA et al (2000) Proportion of colon cancer risk that might be preventable in a cohort of middle-aged US men. Cancer Causes Control 11:579–588. doi:10.1023/A:1008999232442
Driver JA, Gaziano JM, Gelber RP et al (2007) Development of a Risk Score for Colorectal Cancer in Men. Am J Med 120:257–263. doi:10.1016/j.amjmed.2006.05.055
Chan D, Lau R, Aune D et al (2011) P1-109 The WCRF/AICR continuous update project: dietary fibre intake and colorectal cancer incidence. J Epidemiol Community Health 65:A97–A97. doi:10.1136/jech.2011.142976d.2
Giovannucci E, Wu K. Cancers of the Colon and Rectum. In: Cancer Epidemiology and Prevention. 3rd ed. New York, Oxford University Press
Renehan AG, Tyson M, Egger M et al (2008) Body-mass index and incidence of cancer: a systematic review and meta-analysis of prospective observational studies. The Lancet 371:569–578. doi:10.1016/S0140-6736(08)60269-X
White E, Armstrong BK, Saracci R (2008) Principles of exposure measurement in epidemiology, 2nd edn. Oxford University Press, New York
Funding
This work was financially supported by the Biobehavioral Cancer Prevention and Control Training Program at the University of Washington funded by the National Cancer Institute (R25CA92408 to TAH) and by the National Cancer Institute and the National Institutes of Health Office of Dietary Supplements (K05CA154337 to EW). The VITAL cohort was funded by the National Cancer Institute (R01CA74846).
Authors’ contribution
TAH and EW designed the research, including project conception and development of the overall research plan. EW provided essential materials and study oversight. TAH analyzed the data, wrote the paper, and had primary responsibility for final content. All authors read and reviewed the final manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to disclose.
Appendix
Appendix
In the Fall of 2011 we convened an expert panel of nutritional epidemiologists (Emily White, Alan Kristal, Ruth Patterson, Shirley Beresford) with knowledge of the VITAL cohort and the WCRF/AICR recommendations to determine the approach and appropriate cutoffs to be used when operationalizing these recommendations in the VITAL cohort. Decisions on how to operationalize each recommendation were made by first attempting to define adherence using the “Personal Recommendations,” with additional information from the “Public Health Goals” and included references used to determine cutoffs when the personal recommendations were not specific. When the personal recommendations included clear targets, those values were used. The expert panel also decided that the overall analysis approach would treat each recommendation as either being met or not met and that we would not include partial adherence points for the recommendations.
Recommendation 1: body fatness
We set cutoffs of body mass index at baseline of between 18.5 and <25.0 kg/m2 to be consistent with the personal recommendation to “maintain body weight within the normal range from age 21” with a reference to ranges issued by national governments or the World Health Organization (whose cutoffs we used). We opted not to incorporate the additional personal recommendations related to childhood and adolescent body weight and about avoiding weight gain and increases in waist circumference throughout adulthood because the child and adolescent body weight and waist circumference data were not available and, although participant reports of body weight at ages 18, 30, and 45 were available, there were several missing responses, and we were concerned about the accuracy of the provided estimates.
Recommendation 2: physical activity
We utilized the detailed physical activity questionnaire in VITAL, incorporating walking and other moderate and strenuous activities and their frequency and duration over the previous 10 years, to set cutoffs to identify participants meeting the personal recommendation to “be moderately physically active, equivalent to brisk walking for at least 30 min every day.” We ultimately counted participants reporting walking at a moderate or fast (but not casual) pace and/or participating in moderate or strenuous activities (such as running, aerobics, dancing, swimming, cycling, or sports) but not mild exercise (such as golf, slow dancing, or bowling) for an average of at least 30 min per day on an average of at least 5 days per week over at least 7 of the previous 10 years. The personal recommendation to aim for 60 min of moderate or 30 min of vigorous activity every day as fitness improves was not incorporated because data on changes in fitness and activity over time were not available; however, we did capture long-term physical activity patterns by incorporating data from the previous 10 years. The personal recommendation to limit sedentary habits such as watching television was not incorporated because data on sedentary time were not available.
Recommendation 3: foods and drinks that promote weight gain
The personal recommendations to “consume energy-dense foods sparingly,” “avoid sugary drinks,” and “consume ‘fast foods’ sparingly, if at all” did not provide clear cut-points for what constituted meeting this recommendation. The VITAL food frequency questionnaire (FFQ) captures detailed information on beverages and also captures total calories consumed and the average weight in grams of each of the included individual foods and mixed dishes, but does not specifically ask about “fast foods.” We utilized additional information from the associated public health goals that the average energy density of the diets should be lowered to 125 kcal per 100 g to establish our cutoff for dietary energy density of foods consumed. This cutoff excluded beverages, so we further required that participants also consume less than one serving of regular (not diet) soda, fruit drinks, or cranberry juice with added sugar each week. The additional requirement that participants consume fewer than 3 servings of other fruit juices (e.g., orange juice) per week was added in response to suggestions received through peer review of these recommendations.
Recommendation 4: plant foods
The personal recommendations related to plant foods included eating at least 5 portions of fruits and non-starchy vegetables every day, relatively unprocessed grains and/or legumes with every meal, and limiting refined starches. The expert panel decided that participants would be counted as meeting this recommendation if they consumed at least 5 servings per day of fruits and non-starchy vegetables (fruit juices and white potatoes did not count toward meeting the recommendation) and also consumed at least one serving per day of whole grains or legumes. The VITAL FFQ was not developed to capture whole grains separately from refined grains, so this lower threshold was selected to capture regular consumption of these foods rather than requiring the consumption of at least one serving per meal. An additional personal recommendation that individuals who consume starchy roots or tubers as staples also ensure sufficient intake of non-starchy vegetables, fruits, and legumes was not addressed because this dietary pattern is not common in the USA.
Recommendation 5: animal foods
The expert panel decided to follow the personal recommendation that “people who eat red meat to consume less than 500 g (18 oz) a week, very little, if any to be processed” and count participants as meeting this recommendation if they consumed fewer than 18 oz of red or processed meat (reported as individual foods or mixed dishes such as pasta with meat sauce) per week. The additional requirement that participants consume no more than one serving per week of processed meat was added in response to suggestions received through peer review of these recommendations.
Recommendation 6: alcohol
The expert panel followed the personal recommendation that alcohol consumption should be limited to no more than one drink per day for women and no more than two per day for men, where a drink contains between 10 and 15 g of ethanol.
Recommendation 7: preservation, processing, preparation
The expert panel chose not to operationalize the personal recommendations to avoid salt-preserved foods and to not eat moldy grains or legumes because these practices are not common in the USA and appropriate data are not captured in the VITAL FFQ. The panel further decided not to include the recommendation to limit consumption of processed foods and limit intake to less than 2.4 g sodium per day because the validity of sodium measurement using FFQs has not been established.
Recommendation 8: dietary supplements
The personal recommendation that “dietary supplements are not recommended for cancer prevention” was not operationalized. While the public health goal is to increase the proportion of the population meeting nutritional needs through diet, rather than supplements, the WCRF/AICR also cites studies that have suggested that supplements may reduce cancer risk in certain high-risk groups and declines to make a population-wide recommendation on whether to take or avoid supplements.
Rights and permissions
About this article
Cite this article
Hastert, T.A., White, E. Association between meeting the WCRF/AICR cancer prevention recommendations and colorectal cancer incidence: results from the VITAL cohort. Cancer Causes Control 27, 1347–1359 (2016). https://doi.org/10.1007/s10552-016-0814-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-016-0814-6