Abstract
Purpose
Although the relationship between oral contraceptive (OC) use and colorectal cancer (CRC) risk has been studied extensively, the results of epidemiological studies are controversial. Therefore, we carried out a meta-analysis of epidemiological studies to summarize the available evidence and to quantify the potential dose–response relation.
Methods
We searched PubMed database for studies of OC use and CRC risk that were published until the end of March 2014. Random- and fixed-effects models were applied to estimate summary relative risks (RRs) and 95 % confidence intervals (CIs).
Results
Twelve cohorts and seventeen case–control studies with a total of 15,790 CRC cases were included in the final analysis. The summary RR for the ever versus never category of OC use was 0.82 (95 % CI 0.76–0.88). Similar result was observed when we compared the longest duration of OC use with the shortest duration (RR = 0.86, 95 % CI 0.76–0.96). Furthermore, the results of stratified analysis were comparable to those of overall meta-analysis. In dose–response analysis, significant inverse associations emerged in nonlinear models for the duration of OC use and CRC (P nonlinearity = 0.001). The greatest risk reduction was observed when the duration of OC use was approximately 42 months. There was moderate heterogeneity in the analysis, and no evidence of small-study bias was observed.
Conclusions
Based on the findings of this meta-analysis, ever use of OC is associated with lower risk of CRC. Additionally, there is a statistically significant nonlinear inverse association between the duration of OC use and CRC risk.




Similar content being viewed by others
References
Ferlay J, Soerjomataram I, Ervik M et al (2013) GLOBOCAN 2012 v1.0, Cancer Incidence and Mortality Worldwide: IARC CancerBase No. 11 [Internet]. Lyon, France: International Agency for Research on Cancer; 2013. Available from: http://globocan.iarc.fr, Accessed on 1/April/2014
Lin JH, Giovannucci E (2010) Sex hormones and colorectal cancer: what have we learned so far? J Natl Cancer Inst 102:1746–1747
McMichael AJ, Potter JD (1980) Reproduction, endogenous and exogenous sex hormones, and colon cancer: a review and hypothesis. J Natl Cancer Inst 65:1201–1207
Ma J, Pollak MN, Giovannucci E, Chan JM, Tao Y et al (1999) Prospective study of colorectal cancer risk in men and plasma levels of insulin-like growth factor (IGF)-I and IGF-binding protein-3. J Natl Cancer Inst 91:620–625
Weissberger AJ, Ho KK, Lazarus L (1991) Contrasting effects of oral and transdermal routes of estrogen replacement therapy on 24-hour growth hormone (GH) secretion, insulin-like growth factor I, and GH-binding protein in postmenopausal women. J Clin Endocrinol Metab 72:374–381
Campagnoli C, Abba C, Ambroggio S, Peris C (2003) Differential effects of progestins on the circulating IGF-I system. Maturitas 46(Suppl 1):S39–S44
Gunter MJ, Hoover DR, Yu H, Wassertheil-Smoller S, Rohan TE et al (2008) Insulin, insulin-like growth factor-I, endogenous estradiol, and risk of colorectal cancer in postmenopausal women. Cancer Res 68:329–337
Narisawa T, Magadia NE, Weisburger JH, Wynder EL (1974) Promoting effect of bile acids on colon carcinogenesis after intrarectal instillation of N-methyl-N′-nitro-N-nitrosoguanidine in rats. J Natl Cancer Inst 53:1093–1097
Chlebowski RT, Wactawski-Wende J, Ritenbaugh C, Hubbell FA, Ascensao J et al (2004) Estrogen plus progestin and colorectal cancer in postmenopausal women. N Engl J Med 350:991–1004
Ritenbaugh C, Stanford JL, Wu L, Shikany JM, Schoen RE et al (2008) Conjugated equine estrogens and colorectal cancer incidence and survival: the Women’s Health Initiative randomized clinical trial. Cancer Epidemiol Biomarkers Prev 17:2609–2618
Bosetti C, Bravi F, Negri E, La Vecchia C (2009) Oral contraceptives and colorectal cancer risk: a systematic review and meta-analysis. Hum Reprod Update 15:489–498
Cibula D, Gompel A, Mueck AO, La Vecchia C, Hannaford PC et al (2010) Hormonal contraception and risk of cancer. Hum Reprod Update 16:631–650
Fernandez E, La Vecchia C, Balducci A, Chatenoud L, Franceschi S et al (2001) Oral contraceptives and colorectal cancer risk: a meta-analysis. Br J Cancer 84:722–727
Gierisch JM, Coeytaux RR, Urrutia RP, Havrilesky LJ, Moorman PG et al (2013) Oral contraceptive use and risk of breast, cervical, colorectal, and endometrial cancers: a systematic review. Cancer Epidemiol Biomarkers Prev 22:1931–1943
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 339:b2535
Zervoudakis A, Strickler HD, Park Y, Xue X, Hollenbeck A et al (2011) Reproductive history and risk of colorectal cancer in postmenopausal women. J Natl Cancer Inst 103:826–834
Tsilidis KK, Allen NE, Key TJ, Bakken K, Lund E et al (2010) Oral contraceptives, reproductive history and risk of colorectal cancer in the European Prospective Investigation into Cancer and Nutrition. Br J Cancer 103:1755–1759
Kabat GC, Miller AB, Rohan TE (2008) Oral contraceptive use, hormone replacement therapy, reproductive history and risk of colorectal cancer in women. Int J Cancer 122:643–646
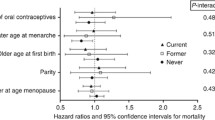
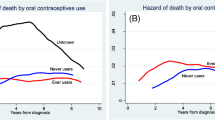
Hannaford PC, Selvaraj S, Elliott AM, Angus V, Iversen L et al (2007) Cancer risk among users of oral contraceptives: cohort data from the Royal College of General Practitioner’s oral contraception study. BMJ 335:651
Lin J, Zhang SM, Cook NR, Manson JE, Buring JE et al (2007) Oral contraceptives, reproductive factors, and risk of colorectal cancer among women in a prospective cohort study. Am J Epidemiol 165:794–801
Rosenblatt KA, Gao DL, Ray RM, Nelson ZC, Thomas DB (2004) Contraceptive methods and induced abortions and their association with the risk of colon cancer in Shanghai, China. Eur J Cancer 40:590–593
Vessey M, Painter R, Yeates D (2003) Mortality in relation to oral contraceptive use and cigarette smoking. Lancet 362:185–191
van Wayenburg CA, van der Schouw YT, van Noord PA, Peeters PH (2000) Age at menopause, body mass index, and the risk of colorectal cancer mortality in the Dutch Diagnostisch Onderzoek Mammacarcinoom (DOM) cohort. Epidemiology 11:304–308
Troisi R, Schairer C, Chow WH, Schatzkin A, Brinton LA et al (1997) Reproductive factors, oral contraceptive use, and risk of colorectal cancer. Epidemiology 8:75–79
Martinez ME, Grodstein F, Giovannucci E, Colditz GA, Speizer FE et al (1997) A prospective study of reproductive factors, oral contraceptive use, and risk of colorectal cancer. Cancer Epidemiol Biomarkers Prev 6:1–5
Bostick RM, Potter JD, Kushi LH, Sellers TA, Steinmetz KA et al (1994) Sugar, meat, and fat intake, and non-dietary risk factors for colon cancer incidence in Iowa women (United States). Cancer Causes Control 5:38–52
Rudolph A, Toth C, Hoffmeister M, Roth W, Herpel E et al (2013) Colorectal cancer risk associated with hormone use varies by expression of estrogen receptor-beta. Cancer Res 73:3306–3315
Lo AC, Soliman AS, Khaled HM, Aboelyazid A, Greenson JK (2010) Lifestyle, occupational, and reproductive factors and risk of colorectal cancer. Dis Colon Rectum 53:830–837
Long MD, Martin CF, Galanko JA, Sandler RS (2010) Hormone replacement therapy, oral contraceptive use, and distal large bowel cancer: a population-based case–control study. Am J Gastroenterol 105:1843–1850
Campbell PT, Newcomb P, Gallinger S, Cotterchio M, McLaughlin JR (2007) Exogenous hormones and colorectal cancer risk in Canada: associations stratified by clinically defined familial risk of cancer. Cancer Causes Control 18:723–733
Nichols HB, Trentham-Dietz A, Hampton JM, Newcomb PA (2005) Oral contraceptive use, reproductive factors, and colorectal cancer risk: findings from Wisconsin. Cancer Epidemiol Biomarkers Prev 14:1212–1218
Levi F, Pasche C, Lucchini F, La Vecchia C (2003) Oral contraceptives and colorectal cancer. Dig Liver Dis 35:85–87
Fernandez E, La Vecchia C, Franceschi S, Braga C, Talamini R et al (1998) Oral contraceptive use and risk of colorectal cancer. Epidemiology 9:295–300
Kampman E, Potter JD, Slattery ML, Caan BJ, Edwards S (1997) Hormone replacement therapy, reproductive history, and colon cancer: a multicenter, case–control study in the United States. Cancer Causes Control 8:146–158
Jacobs EJ, White E, Weiss NS (1994) Exogenous hormones, reproductive history, and colon cancer (Seattle, Washington, USA). Cancer Causes Control 5:359–366
Kampman E, Bijl AJ, Kok C, Van’T VP (1994) Reproductive and hormonal factors in male and female colon cancer. Eur J Cancer Prev 3:329–336
Peters RK, Pike MC, Chang WW, Mack TM (1990) Reproductive factors and colon cancers. Br J Cancer 61:741–748
Kune GA, Kune S, Watson LF (1990) Oral contraceptive use does not protect against large bowel cancer. Contraception 41:19–25
Furner SE, Davis FG, Nelson RL, Haenszel W (1989) A case–control study of large bowel cancer and hormone exposure in women. Cancer Res 49:4936–4940
Potter JD, McMichael AJ (1983) Large bowel cancer in women in relation to reproductive and hormonal factors: a case–control study. J Natl Cancer Inst 71:703–709
Weiss NS, Daling JR, Chow WH (1981) Incidence of cancer of the large bowel in women in relation to reproductive and hormonal factors. J Natl Cancer Inst 67:57–60
Wu-Williams AH, Lee M, Whittemore AS, Gallagher RP, Jiao DA et al (1991) Reproductive factors and colorectal cancer risk among Chinese females. Cancer Res 51:2307–2311
Dorjgochoo T, Shu XO, Li HL, Qian HZ, Yang G et al (2009) Use of oral contraceptives, intrauterine devices and tubal sterilization and cancer risk in a large prospective study, from 1996 to 2006. Int J Cancer 124:2442–2449
Luan NN, Wu QJ, Gong TT, Vogtmann E, Wang YL et al (2013) Breastfeeding and ovarian cancer risk: a meta-analysis of epidemiologic studies. Am J Clin Nutr 98:1020–1031
Guan HB, Wu QJ, Gong TT (2013) Parity and kidney cancer risk: evidence from epidemiologic studies. Cancer Epidemiol Biomarkers Prev 22:2345–2353
Higgins JP, Thompson SG (2002) Quantifying heterogeneity in a meta-analysis. Stat Med 21:1539–1558
DerSimonian R, Laird N (1986) Meta-analysis in clinical trials. Control Clin Trials 7:177–188
Hamling J, Lee P, Weitkunat R, Ambuhl M (2008) Facilitating meta-analyses by deriving relative effect and precision estimates for alternative comparisons from a set of estimates presented by exposure level or disease category. Stat Med 27:954–970
Greenland S, Longnecker MP (1992) Methods for trend estimation from summarized dose-response data, with applications to meta-analysis. Am J Epidemiol 135:1301–1309
Orsini N, Li R, Wolk A, Khudyakov P, Spiegelman D (2012) Meta-analysis for linear and nonlinear dose-response relations: examples, an evaluation of approximations, and software. Am J Epidemiol 175:66–73
Royston P (2000) A strategy for modelling the effect of a continuous covariate in medicine and epidemiology. Stat Med 19:1831–1847
Bagnardi V, Zambon A, Quatto P, Corrao G (2004) Flexible meta-regression functions for modeling aggregate dose-response data, with an application to alcohol and mortality. Am J Epidemiol 159:1077–1086
Egger M, Davey SG, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315:629–634
Begg CB, Mazumdar M (1994) Operating characteristics of a rank correlation test for publication bias. Biometrics 50:1088–1101
Hannaford PC, Iversen L, Macfarlane TV, Elliott AM, Angus V et al (2010) Mortality among contraceptive pill users: cohort evidence from Royal College of General Practitioners’ Oral Contraception Study. BMJ 340:927
Aune D, Lau R, Chan DS, Vieira R, Greenwood DC et al (2011) Nonlinear reduction in risk for colorectal cancer by fruit and vegetable intake based on meta-analysis of prospective studies. Gastroenterology 141:106–118
Everson GT, McKinley C, Kern FJ (1991) Mechanisms of gallstone formation in women. Effects of exogenous estrogen (Premarin) and dietary cholesterol on hepatic lipid metabolism. J Clin Invest 87:237–246
McMichael AJ, Potter JD (1985) Host factors in carcinogenesis: certain bile-acid metabolic profiles that selectively increase the risk of proximal colon cancer. J Natl Cancer Inst 75:185–191
Issa JP, Ottaviano YL, Celano P, Hamilton SR, Davidson NE et al (1994) Methylation of the oestrogen receptor CpG island links ageing and neoplasia in human colon. Nat Genet 7:536–540
Qiu Y, Waters CE, Lewis AE, Langman MJ, Eggo MC (2002) Oestrogen-induced apoptosis in colonocytes expressing oestrogen receptor beta. J Endocrinol 174:369–377
Campbell-Thompson M, Lynch IJ, Bhardwaj B (2001) Expression of estrogen receptor (ER) subtypes and ERbeta isoforms in colon cancer. Cancer Res 61:632–640
Vongpatanasin W, Tuncel M, Wang Z, Arbique D, Mehrad B et al (2003) Differential effects of oral versus transdermal estrogen replacement therapy on C-reactive protein in postmenopausal women. J Am Coll Cardiol 41:1358–1363
Giovannucci E, Pollak MN, Platz EA, Willett WC, Stampfer MJ et al (2000) A prospective study of plasma insulin-like growth factor-1 and binding protein-3 and risk of colorectal neoplasia in women. Cancer Epidemiol Biomarkers Prev 9:345–349
Sutton-Tyrrell K, Wildman RP, Matthews KA, Chae C, Lasley BL et al (2005) Sex-hormone-binding globulin and the free androgen index are related to cardiovascular risk factors in multiethnic premenopausal and perimenopausal women enrolled in the Study of Women Across the Nation (SWAN). Circulation 111:1242–1249
Chang CK, Ulrich CM (2003) Hyperinsulinaemia and hyperglycaemia: possible risk factors of colorectal cancer among diabetic patients. Diabetologia 46:595–607
Moorman PG, Havrilesky LJ, Gierisch JM, Coeytaux RR, Lowery WJ et al (2013) Oral contraceptives and risk of ovarian cancer and breast cancer among high-risk women: a systematic review and meta-analysis. J Clin Oncol 31:4188–4198
Acknowledgments
This study was supported by The National Natural Science Foundation of China (Grants 81072118, 81172491, and 81101527 for Bei Lin); the PhD Programs Foundation of Ministry of Education of China (Grants 20112104110016 and 20112104120019 for Bei Lin); the Shengjing Free Researcher Project (Grant 200807 for Bei Lin); the Younger research fund of Shengjing Hospital (Grant 2014sj09 for Qi-Jun Wu).
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
10552_2014_483_MOESM1_ESM.tif
Forest plot (fixed-effects model) of ever use of oral contraceptive and colon cancer risk. Squares indicate study-specific relative risks (size of the square reflects the study-specific statistical weight); horizontal lines indicate 95% CIs; diamond indicates the summary relative risk estimate with its 95% CI. CI: confidence interval; RR: relative risk (TIFF 2486 kb)
10552_2014_483_MOESM2_ESM.tif
Forest plot (fixed-effects model) of ever use of oral contraceptive and rectal cancer risk. Squares indicate study-specific relative risks (size of the square reflects the study-specific statistical weight); horizontal lines indicate 95% CIs; diamond indicates the summary relative risk estimate with its 95% CI. CI: confidence interval; RR: relative risk (TIFF 1926 kb)
10552_2014_483_MOESM3_ESM.tif
Forest plot (random-effects model) of the duration of oral contraceptive use and colon cancer risk. Squares indicate study-specific relative risks (size of the square reflects the study-specific statistical weight); horizontal lines indicate 95% CIs; diamond indicates the summary relative risk estimate with its 95% CI. CI: confidence interval; RR: relative risk (TIFF 2142 kb)
10552_2014_483_MOESM4_ESM.tif
Forest plot (fixed-effects model) of the duration of oral contraceptive and rectal cancer risk. Squares indicate study-specific relative risks (size of the square reflects the study-specific statistical weight); horizontal lines indicate 95% CIs; diamond indicates the summary relative risk estimate with its 95% CI. CI: confidence interval; RR: relative risk (TIFF 2015 kb)
Rights and permissions
About this article
Cite this article
Luan, NN., Wu, L., Gong, TT. et al. Nonlinear reduction in risk for colorectal cancer by oral contraceptive use: a meta-analysis of epidemiological studies. Cancer Causes Control 26, 65–78 (2015). https://doi.org/10.1007/s10552-014-0483-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-014-0483-2