Abstract
Purpose
Female breast cancer (BC) is the leading cause of cancer incidence and mortality in India, and accounted for 13.5% of new cancer cases and 10% of cancer-related deaths in 2020. This study aims to estimate and report the female BC burden in India at state level from 2012 to 2016 in terms of years of life lost, years lived with disability, and disability-adjusted life years (DALYs), and to project the burden for the year 2025.
Methods
The cancer incidence and mortality data from 28 population-based cancer registries were analysed. The mean mortality to incidence ratio was estimated, and mortality figures were adjusted for underreporting. The burden of female BC was estimated at national and subnational levels using Census data, World Health Organisation’s lifetables, disability weights, and the DisMod-II tool. A negative binomial regression is employed to project burden for 2025.
Results
The burden of BC among Indian women in 2016 was estimated to be 515.4 DALYs per 100,000 women after age standardization. The burden metrics at state level exhibited substantial heterogeneity. Notably, Tamil Nadu, Telangana, Karnataka, and Delhi had a higher burden of BC than states in the eastern and north-eastern regions. The projection for 2025 indicates to a substantial increase, reaching 5.6 million DALYs.
Conclusion
The female BC burden in India was significantly high in 2016 and is expected to substantially increase. Undertaking a multidisciplinary, context-specific approach for its prevention and control can address this rising burden.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cancer is estimated to have caused 9·6 million global deaths in 2017 [1]. Globally, cardiovascular diseases are the leading cause of disability-adjusted life years (DALYs), followed by cancer. Although nearly half of all cancer cases occur in countries with a high Sustainable Development Index (SDI), only a quarter of the DALYs burden is borne by these countries [1]. This suggests that countries with a low SDI face a significant cancer burden. For India, Global cancer observatory (GLOBOCAN) projected 1.3 million new cancer cases and approximately 850,000 cancer-related deaths by 2020. Breast cancer was the leading cause of cancer incidence and mortality in India, accounting for 13.5% of new cancer cases and 10.6% of all cancer deaths [2].
In addition, there is a disparity in leveraging the accessibility of existing facilities and the detection of disease in its advanced stages, putting the survival of women with breast cancer at risk despite advancements in treatment modalities. Patients with stage I disease had a better survival rate of 93.3%, while those with stage IV disease had a survival rate of 24.5%, with an overall survival rate of 73.8% [3]. A population-based study conducted in South India indicated that patients with a lower educational background have lower survival rates which can be attributed to their cancer being in a more advanced stage at the time of diagnosis [4].
Population-based cancer registries (PBCRs) provide a solid foundation for studying the cancer burden across regions and over time in India. Multiple cancer burden studies, including the most recent study by the Indian Council of Medical Research-National Centre of Disease Informatics and Research (ICMR-NCDIR) on cancer burdens in India, have relied on these data [5]. Breast cancer accounted for 21.8% of the total cancer burden in women as measured by DALYs. Under the National Programme for Noncommunicable Diseases (NP-NCD), the Ministry of Health and Family Welfare (MoHFW) has implemented breast cancer population screening programme for all women aged between 30 and 69 years [6]. Despite this, only 1.6% of women aged 30–69 years in India have ever undergone breast cancer screening [7].
India is not a homogeneous country, and each state has distinct demographic, economic, and cultural characteristics. In addition, it has been observed that the incidence, mortality, and mortality-to-incidence ratio (MIR) of breast cancer are closely related to the geographical indicators of development [8]. Examining breast cancer epidemiology at regional levels could, therefore, aid policymakers in tailoring screening and treatment programmes based on local needs to effectively combat the growing breast cancer burden. This study aims to estimate and report the state-wise burden of female breast cancer in India from 2012 to 2016 in terms of Years Lived with Disability (YLDs), Years of Life Lost (YLLs) and DALYs, and to project the burden for the year 2025.
Materials and methods
Population-based cancer registries (PBCRs) serves as reliable and consistent, long-term, national sources of data on the incidence, survival estimates, and trends of cancer in the country. Since the establishment of the National Cancer Registry Programme (NCRP) in 1981, it has served as a valuable data source on the burden of cancer through its network of 28 PBCRs that covers 3.5% of rural, 42.9% of urban, and 53.6% of semi-urban population [9,10,11].
Breast cancer incidence and mortality rates for women of various ages were obtained from 28 different PBCRs across India. Breast cancer incidence and mortality were determined using the ICD-10 code “C50” [12]. We searched for available evidence on the reported mortality to incidence ratio (MIR) in India to adjust the mortality numbers for underreporting of mortality in the country. Two national level studies were identified, with an average MIR for cancer of 35.0% and 75.4% [13, 14]. As a result, all longitudinal data points with reported MIR of 35.0% for breast cancer from PBCRs between 2005 and 2016 were extracted to estimate a standard MIR for breast cancer among Indian women. A total of 33 data points had an MIR of 35.0%, from which a mean MIR of 45.7 was estimated for breast cancer. Based on Akaike's and Bayesian information criteria, the gamma distribution was identified as the best fit to the data. The mean MIR was calculated using the Markov Chain Monte Carlo method. For the registries with reported MIRs less than 45.7%, the MIR was replaced with 45.7%, and adjusted mortality numbers were computed. These adjusted mortality figures were used for further analysis and burden estimation.
Breast cancer incidence and mortality rates were calculated for quinquennial age groups. The incidence rate for a specific group was calculated by dividing the number of newly diagnosed breast cancer cases in a given year by the corresponding mid-year population. Similarly, the mortality rate for a specific group was calculated by dividing the number of breast cancer deaths in a given year (adjusted) by the corresponding mid-year population. The difference distribution method was used to project state-level populations by age for the years 2012 to 2016. The estimated age wise distribution of the female population at all PBCRs for the years 2012 to 2016 is given in Supplementary Table 1.
Estimation of burden
The breast cancer burden was estimated and reported in terms of YLLs, YLDs, and DALYs per 100,000 female population for each state using the corresponding available registry. If registry data for a specific state were unavailable, the closest possible registry data were used for estimation. YLLs were calculated by multiplying the total number of breast cancer deaths in a given age group by the standard life expectancy for that age group. The WHO standard life tables were used to calculate the standard life expectancies of different age groups (Supplementary Table 2). YLDs were calculated by multiplying the total number of prevalent breast cancer cases by the disability weight. The prevalence estimates were generated using the DisMod-II tool [15] with incidence, mortality, MIR, total population, and all-cause mortality rate as inputs. The Sample Registration System (SRS) was used to obtain age-specific all-cause mortality rates for women between 2012 and 2016 [16]. According to the Global Burden of Disease study, the disability weight for metastatic cancer is 0.45 [17]. The DALY metrics were computed by adding the estimated YLLs and YLDs. Finally, the burden metrics (YLLs, YLDs, and DALYs) were age standardized using the WHO World Population Standard Distribution [18]. Furthermore, breast cancer burden metrics for 2025 were projected using data from 2001 to 2016. Negative binomial regression was used for projection because the conditional mean of the burden metrics was less than the conditional variance.
Results
Breast cancer burden at regional level
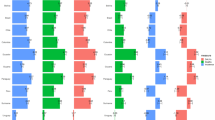
Breast cancer was estimated to result in 515.4 Age-Standardized Rate (ASR)-DALYs per 100,000 Indian women in 2016. Of this, only 14.2 DALYs were contributed by YLDs, while the remaining were contributed by YLLs. The overall burden before age standardization was 468.2 DALYs per 100,000 women. Notably, the burden varied significantly by region. The northern and southern regions exhibited the highest burden in the country, with 685.5 and 677.6 DALYs per 100,000 women, respectively. Central India followed closely with a breast cancer burden of 635.5 DALYs per 100,000 women, while other parts of the country depicted a lower burden. The north-eastern region had the lowest breast cancer burden, with 287.8 DALYs per 100,000 women (refer to Table 1 and Fig. 1).
Breast cancer burden state-wise
At the state level, Kerala had the highest crude rate of DALYs in India, with 733.9 per 100,000 women, followed by Tamil Nadu. Meghalaya exhibited a remarkably low burden at 87 DALYs per 100,000 women. However, on age standardization, the rankings of the states changed due to different age structures. Three southern states, Telangana, Karnataka, and Tamil Nadu, had a breast cancer burden of more than 700 DALYs per 100,000 women, with Telangana having the highest (779.0 DALYs per 100,000 women). The age-adjusted female breast cancer burden in Kerala dropped to 597.3 DALYs per 100,000 women. Several northern and southern states also had high burdens, with 600 DALYs per 100,000 women. Many north-eastern states had a lower burden of breast cancer, with Meghalaya having the lowest burden (142.4 DALYs per 100,000 women) (refer to Table 1 and Fig. 2).
Proportion contribution of YLLs and YLDs
An analysis of the burden in terms of YLLs and YLDs revealed a similar pattern. The burden of YLLs and YLDs was highest in the northern, southern, and central regions of India, while it was lowest in the western, eastern, and north-eastern regions. Arunachal Pradesh was an exception, with a significantly high burden of disability due to breast cancer (YLDs: 29.4 per 100,000 women). The age distribution of DALYs (refer to Fig. 3) indicated that women aged 50 to 69 years experienced the highest burden of breast cancer. The burden gradually increased to this maximum and then gradually decreased after 69 years, with more than three quarters of the breast cancer burden occurring after the reproductive age group of 49 years.
Table 2 displays the crude as well as age-standardized incidence and mortality rates for each registry. The crude incidence rate was highest in the Thiruvananthapuram district registry (47.0 per 100,000 women), followed by Chennai and Kollam districts. However, on age standardization, urban-based registries such as Chennai, Bangalore, Hyderabad district, and Delhi had the highest incidence of breast cancer, whereas mostly rural registries like those in the north-eastern states and Barshi rural had very low incidence rates. This urban–rural split was also observed in age-standardized mortality rates. The national age-standardized rates of breast cancer incidence and mortality were 32.0 and 15.1 per 100,000 women, respectively.
Burden projected for 2025
According to the projections, the burden of female breast cancer in India in 2025 is expected to be 5.6 million DALYs. Premature death due to breast cancer (YLLs) would contribute 5.3 million DALYs to the total burden, with the remaining due to disability (YLDs) (refer to Table 3).
Discussion
This study examines the state-wise burden of female breast cancer in India in 2016 using data from 28 population-based cancer registries under NCRP across the country. In 2018, the age-standardized breast cancer incidence among women in South Central Asia was 25.9 per 100,000 women, according to the GLOBOCAN study [8, 19]. According to the Global Burden of Diseases (GBD) study, the age-standardized rate in South Central Asia in 2016 was 21.6 per 100,000 women [20]. These studies estimated the national and subnational burdens using a wide range of data sources. However, our study only used data from population-based cancer registries under NCRP, which are mainly in urban areas. Rural women are less likely to develop breast cancer than their urban counterparts, and age-standardized incidence rates are higher in urban and metro areas, with Hyderabad, Chennai, Bangalore, and Delhi as leading Indian cities [21, 22]. Urban factors such as a sedentary lifestyle, high obesity rates, delayed age at marriage and childbirth, and minimal breastfeeding have been attributed to a higher burden of breast cancer in urban areas compared to their rural counterparts [23]. This is supported by our study's findings, which indicate that urban registries such as Chennai, Bangalore, and Delhi had higher incidence rates than rural registries. This can explain why our study found a higher incidence of breast cancer (32.0 per 100,000 women) than the GBD and GLOBOCAN estimates.
The study found that the breast cancer burden is higher in the state of Telangana. The relatively low literacy rate among females, higher life expectancy than the national average, high tobacco use, and alcohol consumption among women contributed to the increase in cancer burden in the state [24, 25]. In addition, one in three women were found to be overweight/obese, ranking 6th among the states of India, which is an important risk factor for breast cancer [26]. This was attributed to changing lifestyles, sedentary behaviour, unhealthy eating, and inadequate physical activity [27]. An average delay of 271 days (as noted in a study from neighboring state of Odisha) in disclosing symptoms to loved ones before taking steps toward diagnosis contributes to the late diagnosis of cancer [28].
The GBD also looked at regional variations in female breast cancer. The crude DALYs were found to be higher in states such as Kerala, Punjab, Tamil Nadu, Delhi, Maharashtra, Karnataka, and Haryana [20]. With the exception of Maharashtra, these states have higher DALYs in our study as well. However, the female breast cancer burden estimate for Maharashtra was simply an average of a number of registries that included both urban and rural registries. In our study, we may have underestimated the burden for Maharashtra. However, the majority of these burden differences between states can be explained by their socio-economic development.
Socio-economic factors significantly shape the cancer burden, affecting access to healthcare, preventive measures, and treatment outcomes. Individuals with lower socio-economic status encounter barriers to timely and quality healthcare, leading to delayed cancer detection, compounded by limited resources and health literacy. Occupational exposures and financial strain heighten cancer risks and impact treatment accessibility. Geographical and psychosocial disparities further complicate the issue. Research priorities may inadvertently overlook cancers prevalent in lower socio-economic groups. Recognizing and addressing these disparities is crucial for equitable cancer control, ensuring universal access to prevention, early detection, and treatment. In India, the correlation between cancer prevalence and socio-economic inequalities is evident, emphasizing the need to reevaluate resource allocation and enhance access to healthcare and social support systems [29,30,31,32].
Even global studies have found that developed countries have a higher incidence of breast cancer than developing and underdeveloped countries [19]. This can be applied to India, where more developed states like Tamil Nadu, Telangana, Karnataka, and Delhi have a much higher burden of breast cancer than states in the eastern and north-eastern regions. This is due to known risk factors such as delayed first childbirth, lower parity, higher levels of obesity, a shorter duration of breastfeeding, and physical inactivity, all of which are linked to a region's socio-economic development [33]. Another possible explanation is that states with more advanced healthcare infrastructure have higher levels of awareness, screening, and diagnosis rates.
In developing Asian countries, the incidence of breast cancer peaked in the forties during the early twenty-first century, whereas it peaked in the sixties in developed countries [34, 35]. Our finding that breast cancer incidence peaked after the age of 50 suggests that the age of onset in India has changed since the previous decade, moving from the forties to fifty and above. This is a positive finding despite the rising incidence of breast cancer, as the prognosis for breast cancer in younger women is typically worse [36]. The results of the projection indicated a significant increase in the burden of female breast cancer in India from 2016 levels. Several studies in India have found that the age-standardized incidence of breast cancer is significantly increasing [36,37,38].
The increasing incidence of breast cancer in India underscores the urgent need for comprehensive awareness campaigns and screening programs [39]. A significant concern is that a majority of women diagnosed with breast cancer in the country present with advanced stages or metastatic disease, suggesting a lack of awareness [36]. India faces remarkably low rates of breast cancer screening, encompassing self-breast examination and mammography [40]. Numerous barriers contribute to this, including personal factors (lack of awareness about screening services, methods, lack of prioritization of health, and inadequate education), economic constraints, social stigma around the disease, distrust in the healthcare systems and professionals, inadequate health infrastructure, fears regarding surgical procedures like mastectomy [31, 41,42,43,44,45].
Recognizing the need for intervention, mandatory screening, incentivization, and awareness creation emerge as crucial factors facilitating breast cancer screening. Hence, adopting a multidisciplinary approach that not only raises awareness but also promotes screening and facilitates treatment becomes imperative. Strengthening screening, diagnostic, and treatment facilities for breast cancer patients in India could potentially reduce premature mortality, prevent catastrophic health expenditures, and enhance overall survival rates.
Strengths and limitations
This study reports the breast cancer burden for each Indian state in terms of YLDs, YLLs, and DALYs. Cancer registries play a vital role in collecting incidence, and mortality data and monitoring and evaluating cancer control programs [46]. The data for the study were collected from 28 population-based cancer registries covering 10% of the population in India's various states with annual coverage ranging from a low of 0.69 lakhs to a high coverage of 81.0 lakhs [22]. Population-based cancer registries also ensure that nearly all incident cases within the target populations are recorded. In India, population-based cancer registries (PBCRs) serve as the primary and reliable long-term data sources, offering valuable insights into the magnitude and patterns of cancer. Due to the limited availability of mortality data, we depend on real-time information from PBCRs for both cancer incidence and mortality statistics. The data from some of the PBCRs are regularly published in successive volumes of Cancer Incidence in Five Continents (CI-5) by WHO-IACR/IARC.
In low- and middle-income countries, only a fraction of deaths are recorded in vital registration systems, which may underestimate cause-specific mortality. In this study, however, this issue has been effectively addressed by calculating the national average MIR and adjusting the mortality numbers to account for this under registration of deaths. This study's estimated MIR was nearly comparable to other MIR estimates for India. GLOBOCAN—2018 estimated India's MIR to be between 0 and 59 [8], while GBD—2016 estimated it to be between 0 and 52 [47].
The location of the functioning cancer registries is an important limitation of this study. Assuming that states in the same region would have similar breast cancer epidemiology, estimates for states without a registry were derived from the registry closest to them. Furthermore, the rural component of PBCRs is not presented in the majority of States. However, healthcare in India is primarily a state subject; consequently, screening rates and treatment efficacy can differ between states within the same region. The socio-economic development of the states within a region can also vary, resulting in variations in the health-promoting behaviours of the populations. Even within states, registries are predominantly urban, limiting their applicability to the entire state.
Conclusion
In India, the burden metrics for female breast cancer at the state level demonstrate substantial heterogeneity. This is a result of regional and state-specific differences in lifestyle, exposure to risk factors, and healthcare accessibility. These results show how important it is to design and use strategies based on local needs if we want to halt the rising number of breast cancer cases in the country.
Data availability
Data is available within this paper. The corresponding author can be contacted at director-ncdir@icmr.gov.in for further clarification if required.
Abbreviations
- BC:
-
Breast cancer
- YLLs:
-
Years of life lost
- YLDs:
-
Years lived with disability
- DALYs:
-
Disability adjusted life years
- SDI:
-
Sustainable development index
- PBCR:
-
Population-based cancer registries
- NP-NCD:
-
National programme for noncommunicable diseases
- MoHFW:
-
Ministry of health and family welfare
- MIR:
-
Mortality-to-incidence ratio
- NCRP:
-
National cancer registry programme
- SRS:
-
Sample registration system
- WHO:
-
World health organization
- ASR:
-
Age standardized rate
- GBD:
-
Global burden of diseases
- GLOBOCAN:
-
Global cancer observatory
References
Fitzmaurice C, Abate D, Abbasi N, Abbastabar H, Abd-Allah F, Abdel-Rahman O, Abdelaim A et al (2019) Global burden of disease cancer collaboration. Global, regional, and national cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life-years for 29 cancer groups, 1990 to 2017: a systematic analysis for the global burden of disease study. JAMA Oncol 5(12):1749–68. https://doi.org/10.1001/jamaoncol.2019.2996
World Health Organisation (2021) The global cancer observatory, source: Globocan 2020, 356-india-fact-sheets.pdf. Factsheet-India. World Health Organisation. https://gco.iarc.fr/today/data/factsheets/populations/356-india-fact-sheets.pdf. Accessed 17 Jan 2023
Nandakumar A, Rath GK, Kataki AC, Bapsy PP, Gupta PC, Gangadharan P et al (2016) Decreased survival with mastectomy Vis-à-vis breast-conserving surgery in stage II and III breast cancers: a comparative treatment effectiveness study. J Glob Oncol 3(4):304–313. https://doi.org/10.1200/JGO.2016.004614
Mathew A, George PS, Kunnambath R, Mathew BS, Kumar A, Syampramod R, Booth CM (2020) Educational status, cancer stage, and survival in South India: a population-based study. JCO Glob Oncol 6:1704–1711. https://doi.org/10.1200/GO.20.00259
Kulothungan V, Sathishkumar K, Leburu S, Ramamoorthy T, Stephen S, Basavarajappa D et al (2022) Burden of cancers in India–estimates of cancer crude incidence, YLLs, YLDs and DALYs for 2021 and 2025 based on national cancer registry program. BMC Cancer 22(1):527. https://doi.org/10.1186/s12885-022-09578-1
Banerjee B (2017) Chapter-30 national programme for prevention and control of cancer, diabetes, cardiovascular diseases and stroke (NPCDCS). DK Taneja’s health policies and programmes in India, 15th edn. Jaypee Brothers Medical Publishers Ltd, New Delhi, p 15
Indian Council of Medical Research–National Centre for Disease Informatics and Research (2020) National noncommunicable disease monitoring survey 2017–18. Indian Council of Medical Research–National Centre for Disease Informatics and Research. https://www.ncdirindia.org/nnms/. Accessed 14 Feb 2023
Sharma R (2021) Global, regional, national burden of breast cancer in 185 countries: evidence from GLOBOCAN 2018. Breast Cancer Res Treat 187(2):557–567. https://doi.org/10.1007/s10549-020-06083-6
Indian Council of Medical Research–National Centre for Disease Informatics and Research (2020) Report of national cancer registry programme. Indian Council of Medical Research–National Centre for Disease Informatics and Research. https://www.ncdirindia.org/All_Reports/Report_2020/resources/NCRP_2020_2012_16.pdf. Accessed 19 Aug 2020
Mathur P, Krishnan S, Chaturvedi M, Das P, Kondalli LS, Santhappan S et al (2020) Cancer statistics, 2020: report from national cancer registry programme, India. JCO Glob Oncol 6:1063–1075. https://doi.org/10.1200/GO.20.00122
Krishnan S, Chaturvedi M, Das P, Stephen S, Mathur P (2022) Cancer incidence estimates for 2022 & projection for 2025: result from national cancer registry programme India. Indian J Med Res 156:598–607. https://doi.org/10.4103/ijmr.ijmr_1821_22
World Health Organisation (2020) WHO methods and data sources for global burden of disease estimates 2000–2019. World Health Organisation. https://cdn.who.int/media/docs/default-source/gho-documents/global-health-estimates/ghe2019_daly-methods.pdf
Parkin DM, Bray F (2009) Evaluation of data quality in the cancer registry: principles and methods part II. Completeness. Eur J Cancer Oxf Engl 45(5):756–64. https://doi.org/10.1016/j.ejca.2008.11.033
Dhillon PK, Mathur P, Nandakumar A, Fitzmaurice C, Kumar GA, Mehrotra R et al (2018) The burden of cancers and their variations across the states of India: the global burden of disease study 1990–2016. Lancet Oncol 19(10):1289–1306. https://doi.org/10.1016/S1470-2045(18)30447-9
Barendregt JJ, van Oortmarssen GJ, Vos T, Murray CJL (2003) A generic model for the assessment of disease epidemiology: the computational basis of DisMod II. Popul Health Metr 1:4. https://doi.org/10.1186/1478-7954-1-4
Office of the Registrar General & Census Commissioner, India. Ministry of home affairs, government of India. SRS statistical report. Ministry of home affairs. https://censusindia.gov.in/vital_statistics/SRS_Statistical_Report.html
Global Burden of Disease Collaborative Network (2020) Global burden of disease study 2019 (GBD 2019) disability weights. Institute for Health Metrics and Evaluation (IHME), Seattle, USA
Ahmad OB, Boschi-Pinto C, Lopez AD, Murray CJ, Lozano R, Inoue M (2001) Age standardization of rates: a new WHO standard. Geneva World Health Organ 9(10):1–4
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68(6):394–424. https://doi.org/10.3322/caac.21492
India State-Level Disease Burden Initiative Cancer Collaborators (2018) The burden of cancers and their variations across the states of India: the global burden of disease study 1990–2016. Lancet Oncol 19(10):1289–306. https://doi.org/10.1016/S1470-2045(18)30447-9
Nagrani RT, Budukh A, Koyande S, Panse NS, Mhatre SS, Badwe R (2014) Rural urban differences in breast cancer in India. Indian J Cancer 51(3):277–281. https://doi.org/10.4103/0019-509X.146793
Chaturvedi M, Sathishkumar K, Lakshminarayana SK, Nath A, Das P, Mathur P (2022) Women cancers in India: incidence, trends and their clinical extent from the national cancer registry programme. Cancer Epidemiol 80:102248. https://doi.org/10.1016/j.canep.2022.102248
International Agency for Research on Cancer–World Health Organisation (2020) World cancer report: cancer research for cancer prevention. International agency for research on cancer–World health organisation. https://shop.iarc.fr/products/world-cancer-report-cancer-research-for-cancer-prevention-pdf. Accessed 20 Aug 2020
Indian Council of Medical Research–National Centre for Disease Informatics and Research (2021) Profile of cancer and related factors–Telangana. Indian council of medical research–national centre for disease informatics and research. https://ncdirindia.org/All_Reports/State_Factsheet_21/Factsheet/FS_Telangana.pdf. Accessed 3 Sep 2022
Mahajan H, Reddy N, Devi NGM, Poli UR, Jayaram M, Tetali S et al (2023) Projected cancer burden, challenges, and barriers to cancer prevention and control activities in the state of Telangana. PLoS ONE 18(7):e0278357. https://doi.org/10.1371/journal.pone.0278357
Ministry of Health and Family Welfare–Government of India (2020) National family health survey (NFHS 5) 2019–21. Ministry of health and family welfare–Government of India. https://main.mohfw.gov.in/sites/default/files/NFHS-5_Phase-II_0.pdf. Accessed 3 Sep 2022
Ramanujam K, Mergu N, Kondeth H et al (2023) Chronic illness, nutritional status, and factors associated with malnutrition among various age groups residing in urban areas of Telangana and rural areas of Andhra Pradesh. Nutrients 15(20):4470. https://doi.org/10.3390/nu15204470
Weller D, Pati S (2014) P07: patient pathways to cancer diagnosis and delay in care seeking: an exploratory study in Odisha (India). Eur J Cancer Care 23(3):12. https://doi.org/10.1111/ecc.12226
Mohandas K, Mallath D, Taylor DG et al (2014) The growing burden of cancer in India: epidemiology and social context. Lancet Oncol 15(6):e205–e212. https://doi.org/10.1016/S1470-2045(14)70115-9
Mohanty SK, Wadasadawala T, Sen S et al (2023) Socio-economic variations of breast cancer treatment and discontinuation: a study from a public tertiary cancer hospital in Mumbai India. BMC Women Health 23:113. https://doi.org/10.1186/s12905-023-02275-6
Kulothungan V, Ramamoorthy T, Mohan R, Mathur P (2023) Assessing progress of India in reduction of premature mortality due to four noncommunicable diseases towards achieving the WHO 25 × 25 goal and the sustainable development goals. Sustain Dev. https://doi.org/10.1002/sd.2761
Monica MR (2020) An epidemiological study of cervical and breast screening in India: district-level analysis. BMC Womens Health 20(1):225. https://doi.org/10.1186/s12905-020-01083-6
Ginsburg O, Bray F, Coleman MP et al (2017) The global burden of women’s cancers: an unmet grand challenge in global health. Lancet Lond Engl 389(10071):847–860. https://doi.org/10.1016/S0140-6736(16)31392-7
Khokhar A (2012) Breast cancer in India: where do we stand and where do we go? Asian Pac J Cancer Prev 13(10):4861–4866. https://doi.org/10.7314/apjcp.2012.13.10.4861
Agarwal G, Pradeep PV, Aggarwal V, Yip CH, Cheung PSY (2007) Spectrum of breast cancer in Asian women. World J Surg 5:1031–1040. https://doi.org/10.1007/s00268-005-0585-9
Malvia S, Bagadi SA, Dubey US, Saxena S (2017) Epidemiology of breast cancer in Indian women. Asia Pac J Clin Oncol 13(4):289–295. https://doi.org/10.1111/ajco.12661
Sathishkumar KNV, Badwe RA et al (2021) Trends in breast and cervical cancer in India under national cancer registry programme: an age-period-cohort analysis. Cancer Epidemiol 74:101982. https://doi.org/10.1016/j.canep.2021.101982
Dhillon PK, Yeole BB, Dikshit R, Kurkure AP, Bray F (2011) Trends in breast, ovarian and cervical cancer incidence in Mumbai, India over a 30-year period, 1976–2005: an age–period–cohort analysis. Breast J Cancer 105(5):723–730. https://doi.org/10.1038/bjc.2011.301
Mehrotra R, Yadav K (2022) Breast cancer in India: present scenario and the challenges ahead. World J Clin Oncol 13(3):209–218. https://doi.org/10.5306/wjco.v13.i3.209
Pal A, Taneja N, Malhotra N et al (2021) Knowledge, attitude, and practice towards breast cancer and its screening among women in India: a systematic review. J Cancer Res Ther 17(6):1314–1321. https://doi.org/10.4103/jcrt.jcrt_922_20
Kaur K, Jajoo R, Naman S, Kandwal T, Brar GS, Garg P et al (2023) Identifying barriers to early diagnosis of breast cancer and perception of women in Malwa region of Punjab India. Glob Health J 7(1):34–42. https://doi.org/10.1016/j.glohj.2023.02.006
D’almeida D, Latha T (2021) Barriers for early detection of breast cancer among South Indian women. Indian J Commun Med 46(4):706–709. https://doi.org/10.4103/ijcm.IJCM_751_20
Tripathi N, Kadam YR, Dhobale RV, Gore AD (2014) Barriers for early detection of cancer amongst Indian rural women. South Asian J Cancer 3(2):122–127. https://doi.org/10.4103/2278-330X.130449
Mahalakshmi S, Suresh S (2020) Barriers to cancer screening uptake in women: a qualitative study from Tamil Nadu India. Asian Pac J Cancer Prev 21(4):1081–1087. https://doi.org/10.31557/APJCP.2020.21.4.1081
Dey S, Sharma S, Mishra A, Krishnan S, Govil J, Dhillon PK (2016) Breast cancer awareness and prevention behavior among women of Delhi, India: identifying barriers to early detection. Breast Cancer (Auckl) 10:147–156. https://doi.org/10.4137/BCBCR.S40358
International Agency for Research on Cancer–World Health Organisation (2023) Cancer incidence in five continents, vol. XII (IARC CancerBase No. 19). Lyon: international agency for research on cancer–world health organisation. https://ci5.iarc.who.int. Accessed 3 Apr 2023
Sharma R (2019) Breast cancer incidence, mortality and mortality-to-incidence ratio (MIR) are associated with human development, 1990–2016 evidence from global burden of disease study. Breast Cancer Tokyo Jpn 26(4):428–445. https://doi.org/10.1007/s12282-018-00941-4
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
VK and PM designed the study and oversaw the research. VK, PM and TR developed the concept and drafted the manuscript. VK, TR, RM, NT and GJM prepared the tables and figures. VK, TR, KS, RM, NT and GJM reviewed the results. Authors VK and TR performed statistical modelling and finalized the results. Authors VK, PM, TR, KS, and GJM reviewed all versions of the manuscript. VK, PM, TR and KS finalized the manuscript. All authors reviewed and finalized the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors have no relevant financial or non-financial interests to disclose.
Ethical approval
All the data comes from secondary, unidentifiable records. The methods performed were in accordance with the relevant guidelines and regulations. The study has been granted an exemption from requiring ethics approval from the Institutional Ethics Committee at ICMR-NCDIR, Bengaluru. The approval number is NCDIR/IEC/3020/2020.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kulothungan, V., Ramamoorthy, T., Sathishkumar, K. et al. Burden of female breast cancer in India: estimates of YLDs, YLLs, and DALYs at national and subnational levels based on the national cancer registry programme. Breast Cancer Res Treat 205, 323–332 (2024). https://doi.org/10.1007/s10549-024-07264-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-024-07264-3