Abstract
Introduction
Breast cancer patients with invasive lobular carcinoma (ILC) have an increased risk of positive margins after surgery and often show little response to neoadjuvant chemotherapy (NAC). We aimed to investigate surgical outcomes in patients with ILC treated with NAC.
Methods
In this retrospective cohort study, all breast cancer patients with ILC treated with NAC who underwent surgery at the Netherlands Cancer Institute from 2010 to 2019 were selected. Patients with mixed type ILC in pre-NAC biopsies were excluded if the lobular component was not confirmed in the surgical specimen. Main outcomes were tumor-positive margins and re-excision rate. Associations between baseline characteristics and tumor-positive margins were assessed, as were complications, locoregional recurrence rate (LRR), recurrence-free survival (RFS), and overall survival (OS).
Results
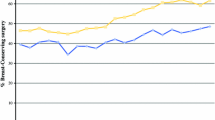
We included 191 patients. After NAC, 107 (56%) patients had breast conserving surgery (BCS) and 84 (44%) patients underwent mastectomy. Tumor-positive margins were observed in 67 (35%) patients. Fifty five (51%) had BCS and 12 (14%) underwent mastectomy (p value < 0.001). Re-excision was performed in 35 (33%) patients with BCS and in 4 (5%) patients with mastectomy. Definitive surgery was mastectomy in 107 (56%) patients and BCS in 84 (44%) patients. Tumor-positive margins were associated with cT ≥ 3 status (OR 4.62, 95% CI 1.26–16.98, p value 0.021) in the BCS group. Five-year LRR (4.7%), RFS (81%), and OS (93%) were not affected by type of surgery after NAC.
Conclusion
Although 33% of ILC breast cancer patients undergoing BCS after NAC required re-excision for positive resection margins, it is considered safe given that five-year RFS remained excellent and LRR and OS did not differ by extent of surgery.

Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the corresponding author, IVDP, upon reasonable request.
Abbreviations
- ALND:
-
Axillary lymph node dissection
- BCS:
-
Breast conserving surgery
- BCT:
-
Breast conserving therapy
- CI:
-
Confidence interval
- DCIS:
-
Ductal carcinoma in situ
- HER2:
-
Human Epidermal growth factor Receptor 2
- HR:
-
Hormone receptor
- ILC:
-
Invasive lobular carcinoma
- LCIS:
-
Lobular carcinoma in situ
- LRR:
-
Locoregional recurrence rate
- MARI:
-
Marked axillary lymph node
- MRI:
-
Magnetic resonance imaging
- NKI-AVL:
-
Netherlands Cancer Institute-Antoni van Leeuwenhoek
- NAC:
-
Neoadjuvant chemotherapy
- OR:
-
Odds ratio
- OS:
-
Overall survival
- pCR:
-
Pathologic complete response
- rCR:
-
Radiologic complete response
- RFS:
-
Recurrence free survival
- rPR:
-
Radiologic partial response
- TN:
-
Triple negative
References
van der Noordaa MEM, Ioan I, Rutgers EJ, van Werkhoven E, Loo CE, Voorthuis R et al (2021) Breast-conserving therapy in patients with cT3 breast cancer with good response to neoadjuvant systemic therapy results in excellent local control: a comprehensive cancer center experience. Ann Surg Oncol 28(12):7383–7394. https://doi.org/10.1245/s10434-021-09865-4
Spronk PER, Volders JH, van den Tol P, Smorenburg CH, Vrancken PM (2019) Breast conserving therapy after neoadjuvant chemotherapy; data from the Dutch Breast Cancer Audit. Eur J Surg Oncol 45(2):110–117. https://doi.org/10.1016/j.ejso.2018.09.027
Shin HC, Han W, Moon HG, Im SA, Moon WK, Park IA et al (2013) Breast-conserving surgery after tumor downstaging by neoadjuvant chemotherapy is oncologically safe for stage III breast cancer patients. Ann Surg Oncol 20(8):2582–2589. https://doi.org/10.1245/s10434-013-2909-6
Simons JM, Jacobs JG, Roijers JP, Beek MA, Boonman-de Winter LJM, Rijken AM et al (2021) Disease-free and overall survival after neoadjuvant chemotherapy in breast cancer: breast-conserving surgery compared to mastectomy in a large single-centre cohort study. Breast Cancer Res Treat 185(2):441–451. https://doi.org/10.1007/s10549-020-05966-y
Mamtani A, King TA (2018) Lobular breast cancer: different disease, different algorithms? Surg Oncol Clin N Am 27(1):81–94. https://doi.org/10.1016/j.soc.2017.07.005
Sikov WM, Berry DA, Perou CM, Singh B, Cirrincione CT, Tolaney SM et al (2015) Impact of the addition of carboplatin and/or bevacizumab to neoadjuvant once-per-week paclitaxel followed by dose-dense doxorubicin and cyclophosphamide on pathologic complete response rates in stage II to III triple-negative breast cancer: CALGB 40603 (Alliance). J Clin Oncol 33(1):13–21. https://doi.org/10.1200/JCO.2014.57.0572
Schneeweiss A, Chia S, Hickish T, Harvey V, Eniu A, Hegg R et al (2013) Pertuzumab plus trastuzumab in combination with standard neoadjuvant anthracycline-containing and anthracycline-free chemotherapy regimens in patients with HER2−positive early breast cancer: a randomized phase II cardiac safety study (TRYPHAENA). Ann Oncol 24(9):2278–2284. https://doi.org/10.1093/annonc/mdt182
van Ramshorst MS, van der Voort A, van Werkhoven ED, Mandjes IA, Kemper I, Dezentje VO et al (2018) Neoadjuvant chemotherapy with or without anthracyclines in the presence of dual HER2 blockade for HER2−positive breast cancer (TRAIN-2): a multicentre, open-label, randomised, phase 3 trial. Lancet Oncol 19(12):1630–1640. https://doi.org/10.1016/S1470-2045(18)30570-9
Dossus L, Benusiglio PR (2015) Lobular breast cancer: incidence and genetic and non-genetic risk factors. Breast Cancer Res 17:37. https://doi.org/10.1186/s13058-015-0546-7
O’Connor DJ, Davey MG, Barkley LR, Kerin MJ (2022) Differences in sensitivity to neoadjuvant chemotherapy among invasive lobular and ductal carcinoma of the breast and implications on surgery-A systematic review and meta-analysis. Breast 61:1–10. https://doi.org/10.1016/j.breast.2021.11.017
Lips EH, Mukhtar RA, Yau C, de Ronde JJ, Livasy C, Carey LA et al (2012) Lobular histology and response to neoadjuvant chemotherapy in invasive breast cancer. Breast Cancer Res Treat 136(1):35–43. https://doi.org/10.1007/s10549-012-2233-z
Mann RM, Cho N, Moy L (2019) Breast MRI: state of the art. Radiology 292(3):520–536. https://doi.org/10.1148/radiol.2019182947
Loo CE, Straver ME, Rodenhuis S, Muller SH, Wesseling J, Vrancken Peeters MJ et al (2011) Magnetic resonance imaging response monitoring of breast cancer during neoadjuvant chemotherapy: relevance of breast cancer subtype. J Clin Oncol 29(6):660–666. https://doi.org/10.1200/JCO.2010.31.1258
Kim J, Han BK, Ko EY, Ko ES, Choi JS, Park KW (2022) Prediction of pathologic complete response on MRI in patients with breast cancer receiving neoadjuvant chemotherapy according to molecular subtypes. Eur Radiol 32(6):4056–4066. https://doi.org/10.1007/s00330-021-08461-0
Janssen LM, den Dekker BM, Gilhuijs KGA, van Diest PJ, van der Wall E, Elias SG (2022) MRI to assess response after neoadjuvant chemotherapy in breast cancer subtypes: a systematic review and meta-analysis. NPJ Breast Cancer 8(1):107. https://doi.org/10.1038/s41523-022-00475-1
McCart Reed AE, Kutasovic JR, Lakhani SR, Simpson PT (2015) Invasive lobular carcinoma of the breast: morphology, biomarkers and ’omics. Breast Cancer Res 17:12. https://doi.org/10.1186/s13058-015-0519-x
Kim SY, Cho N, Park IA, Kwon BR, Shin SU, Kim SY et al (2018) Dynamic contrast-enhanced breast MRI for evaluating residual tumor size after neoadjuvant chemotherapy. Radiology 289(2):327–334. https://doi.org/10.1148/radiol.2018172868
Olsen MA, Nickel KB, Margenthaler JA, Wallace AE, Mines D, Miller JP et al (2015) Increased risk of surgical site infection among breast-conserving surgery re-excisions. Ann Surg Oncol 22(6):2003–2009. https://doi.org/10.1245/s10434-014-4200-x
Fraser VJ, Nickel KB, Fox IK, Margenthaler JA, Olsen MA (2016) The epidemiology and outcomes of breast cancer surgery. Trans Am Clin Climatol Assoc 127:46–58
Xue DQ, Qian C, Yang L, Wang XF (2012) Risk factors for surgical site infections after breast surgery: a systematic review and meta-analysis. Eur J Surg Oncol 38(5):375–381. https://doi.org/10.1016/j.ejso.2012.02.179
O’Connell RL, Rattay T, Dave RV, Trickey A, Skillman J, Barnes NLP et al (2019) The impact of immediate breast reconstruction on the time to delivery of adjuvant therapy: the iBRA-2 study. Br J Cancer 120(9):883–895. https://doi.org/10.1038/s41416-019-0438-1
Tolaney SM, Barry WT, Dang CT, Yardley DA, Moy B, Marcom PK et al (2015) Adjuvant paclitaxel and trastuzumab for node-negative, HER2−positive breast cancer. N Engl J Med 372(2):134–141. https://doi.org/10.1056/NEJMoa1406281
Koolen BB, Donker M, Straver ME, van der Noordaa MEM, Rutgers EJT, Valdes Olmos RA et al (2017) Combined PET-CT and axillary lymph node marking with radioactive iodine seeds (MARI procedure) for tailored axillary treatment in node-positive breast cancer after neoadjuvant therapy. Br J Surg 104(9):1188–1196. https://doi.org/10.1002/bjs.10555
Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R et al (2009) New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer 45(2):228–247. https://doi.org/10.1016/j.ejca.2008.10.026
Nationaal Borstkanker Overleg Nederland NIV. Borstkanker 2020. https://richtlijnendatabase.nl/richtlijn/borstkanker/algemeen.html.
Vos EL, Siesling S, Baaijens MHA, Verhoef C, Jager A, Voogd AC et al (2017) Omitting re-excision for focally positive margins after breast-conserving surgery does not impair disease-free and overall survival. Breast Cancer Res Treat 164(1):157–167. https://doi.org/10.1007/s10549-017-4232-6
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205–213. https://doi.org/10.1097/01.sla.0000133083.54934.ae
Straver ME, Rutgers EJ, Rodenhuis S, Linn SC, Loo CE, Wesseling J et al (2010) The relevance of breast cancer subtypes in the outcome of neoadjuvant chemotherapy. Ann Surg Oncol 17(9):2411–2418. https://doi.org/10.1245/s10434-010-1008-1
Tubiana-Hulin M, Stevens D, Lasry S, Guinebretiere JM, Bouita L, Cohen-Solal C et al (2006) Response to neoadjuvant chemotherapy in lobular and ductal breast carcinomas: a retrospective study on 860 patients from one institution. Ann Oncol 17(8):1228–1233. https://doi.org/10.1093/annonc/mdl114
Boughey JC, Wagner J, Garrett BJ, Harker L, Middleton LP, Babiera GV et al (2009) Neoadjuvant chemotherapy in invasive lobular carcinoma may not improve rates of breast conservation. Ann Surg Oncol 16(6):1606–1611. https://doi.org/10.1245/s10434-009-0402-z
Dillon MF, Hill AD, Fleming FJ, O’Doherty A, Quinn CM, McDermott EW et al (2006) Identifying patients at risk of compromised margins following breast conservation for lobular carcinoma. Am J Surg 191(2):201–205. https://doi.org/10.1016/j.amjsurg.2005.03.041
Mann RM, Hoogeveen YL, Blickman JG, Boetes C (2008) MRI compared to conventional diagnostic work-up in the detection and evaluation of invasive lobular carcinoma of the breast: a review of existing literature. Breast Cancer Res Treat 107(1):1–14. https://doi.org/10.1007/s10549-007-9528-5
Mann RM, Loo CE, Wobbes T, Bult P, Barentsz JO, Gilhuijs KG et al (2010) The impact of preoperative breast MRI on the re-excision rate in invasive lobular carcinoma of the breast. Breast Cancer Res Treat 119(2):415–422. https://doi.org/10.1007/s10549-009-0616-6
van Loevezijn AA, Geluk CS, van den Berg MJ, van Werkhoven ED, Vrancken Peeters M, van Duijnhoven FH et al (2023) Immediate or delayed oncoplastic surgery after breast conserving surgery at the Netherlands Cancer Institute: a cohort study of 251 cases. Breast Cancer Res Treat. https://doi.org/10.1007/s10549-022-06841-8
Fodor J, Major T, Toth J, Sulyok Z, Polgar C (2011) Comparison of mastectomy with breast-conserving surgery in invasive lobular carcinoma: 15-Year results. Rep Pract Oncol Radiother 16(6):227–231. https://doi.org/10.1016/j.rpor.2011.06.005
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by AKEvanH and AAvanL. The first draft of the manuscript was written by AKEvanH and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors have no relevant financial or non-financial interests to disclose.
Ethical approval
This study was approved by the institutional review board of the Netherlands Cancer Institute.
Consent to participate
Informed consent was obtained from all individual participants by ‘general hospital informed consent’ from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
van Hemert, A., van Loevezijn, A.A., Bosman, A. et al. Breast surgery after neoadjuvant chemotherapy in patients with lobular carcinoma: surgical and oncologic outcome. Breast Cancer Res Treat 204, 497–507 (2024). https://doi.org/10.1007/s10549-023-07192-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-023-07192-8