Abstract
Purpose
Mastectomy, breast reconstruction (BR) and breast conserving therapy (BCT) are core components of the treatment paradigm for early-stage disease but are differentially associated with significant financial burdens. Given recent price transparency regulations, we sought to characterize rates of disclosure for breast cancer-related surgery, including mastectomy, BCT, and BR (oncoplastic reconstruction, implant, pedicled flap and free flap) and identify associated factors.
Methods
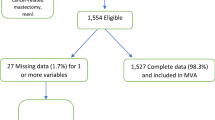
For this cross-sectional analysis, cost reports were obtained from the Turquoise Health price transparency platform for all U.S. hospitals meeting national accreditation standards for breast cancer care. The Healthcare Cost Report Information System was used to collect facility-specific data. Addresses were geocoded to identify hospital referral and census regions while data from CMS was also used to identify the geographic practice cost index. We leveraged a Poisson regression model and relevant Medicare billing codes to analyze factors associated with price disclosure and the availability of an OOP price estimator.
Results
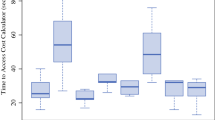
Of 447 identified hospitals, 221 (49.4%) disclosed prices for mastectomy and 188 42.1%) disclosed prices for both mastectomy and some form of reconstruction including oncoplastic reduction (n = 184, 97.9%), implants (n = 187, 99.5%), pedicled flaps (n = 89, 47.3%), and free flaps (n = 81, 43.1%). Non-profit status and increased market competition were associated with price nondisclosure. 121 hospitals (27.1%) had an out-of-pocket price estimator that included at least one breast surgery.
Conclusions
Most eligible hospitals did not disclose prices for breast cancer surgery. Distinct hospital characteristics were associated with price disclosure. Breast cancer patients face persistent difficulty in accessing costs.

Similar content being viewed by others
References
Giaquinto A, Sung H, Miller K et al (2022) Breast cancer statistics. CA Cancer J Clin 72(6):524–541
Winters Z, Benson J, Pusic A (2010) A systematic review of the clinical evidence to guide treatment recommendations in breast reconstruction based on patient- reported outcome measures and health-related quality of life. Ann Surg 252(6):929–942
Bailey C, Selber J, Liu J, Lee C, Offodile AC 2nd (2021) Current practice and perceptions regarding cost communication in breast cancer reconstruction: survey results of the American Society of Plastic Surgeons. Ann Surg Oncol 28(1):376–385
Greenup R, Rushing C, Fish L et al (2019) Financial costs and burden related to decisions for breast cancer surgery. J Oncol Pract 15(8):e666–e676
Offodile AC 2nd, Lee C (2018) Future directions for breast reconstruction on the 20th Anniversary of the Women’s Health and Cancer Rights Act. JAMA Surg 153(7):605–606
Wharam J, Zhang F, Wallace J et al (2019) Vulnerable and less vulnerable women in high-deductible health plans experienced delayed breast cancer care. Health Aff 38(3):408–415
Zafar S, Abernethy A (2013) Financial toxicity, part I: a new name for a growing problem. Oncology 27(2):80–81
Offodile AC 2nd, Asaad M, Boukovalas S et al (2021) Financial toxicity following surgical treatment for breast cancer: a cross-sectional pilot study. Ann Surg Oncol 28(5):2451–2462
Coroneos C, Lin Y, Sidey-Gibbons C et al (2020) Correlation between financial toxicity, quality of life, and patient satisfaction in an insured population of breast cancer surgical patients: a single-institution retrospective study. J Am Coll Surg 232(3):253–263
Bailey C, Asaad M, Boukovalas S et al (2021) Understanding the relationship between breast reconstruction subtype and risk of financial toxicity: a single-institution pilot study. Plast Reconstr Surg 148(1):1e–11e
Fayanju O, Greenup R, Zafar S, Hyslop T, Hwang E, Fish L (2023) Modifiable barriers and facilitators for breast cancer care: a thematic analysis of patient and provider perspectives. J Surg Res 284:269–279
Rochlin D, Rizk N, Matros E, Wagner T, Sheckter C (2022) Commercial price variation for breast reconstruction in the era of price transparency. JAMA Surg 158:152
Price transparency data for researchers. Turquoise health. https://turquoise.health/researchers. Accessed 14 Oct 2023
Jiang J, Makary M, Bai G (2022) Commercial negotiated prices for CMS-specified shoppable radiology services in U.S. hospitals. Radiology 302(3):622–624
Sanchez G (2022) Variation in reported hospital cash prices across the United States and how they compare to reported payer-specific negotiated rates. Econ Lett 211:110226
Berlin N, Chopra Z, Bryant A et al (2022) Individualized out-of-pocket price estimators for “shoppable” surgical procedures: a Nationwide Cross-Sectional Study of US hospitals. Ann Surg Open 3(2):e162
Cost Reports (2022) Centers for Medicare and Medicaid Services. https://www.cms.gov/data-research/statistics-trends-and-reports/cost-reports. Accessed 14 Oct 2023
Fulton B (2017) Health care market concentration trends in the United States: evidence and policy responses. Health Aff 36(9):1530–1538
Gaynor M, Ho K, Town R (2015) The industrial organization of healthcare markets. J Econ Lit 53(2):235–284
Capps C, Dranove D (2004) Hospital consolidation and negotiated PPO prices. Health Aff 23(2):175–181
Centers for Medicare and Medicaid Services (2023) National physician fee schedule and relative value files. https://www.cms.gov/medicare/payment/fee-schedules/physician/pfs-relative-value-files. Accessed 14 Oct 2023
Best Hospitals Award Methodology. Women’s choice award. https://womenschoiceaward.com/hospitalmethodology/#:~:text=The%20Women's%20Choice%20Award%C2%AE,women%20make%20smart%20healthcare%20choices. Accessed 14 Oct 2023
Garg A (2020) Community-based cancer care quality and expertise in a COVID-19 era and beyond. Am J Clin Oncol 43(8):537–538
List of CPT/HCPCS Codes (2022) Centers for Medicare and Medicaid services. https://www.cms.gov/medicare/regulations-guidance/physician-self-referral/list-cpt/hcpcs-codes. Accessed 14 Oct 2023
von Elm E, Altman D, Egger M et al (2008) The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol 61(4):344–349
Jiang JX, Makary MA, Bai G (2021) Where are the high-price hospitals? With the transparency rule in effect, colonoscopy prices suggest they’re all over the place. In: Health Affairs Blog: Health Affairs
Nierengarten MB (2021) Greater price transparency needed for thyroid cancer treatment among US cancer centres. Lancet Oncol 22(7):914
Berkowitz ST, Siktberg J, Hamdan SA, Triana AJ, Patel SN (2021) Health care price transparency in ophthalmology. JAMA Ophthalmol 139(11):1210–1216
Chino F, Johnson J, Moss H (2021) Compliance with price transparency rules at US National Cancer Institute-Designated Cancer Centers. JAMA Oncol 7(12):1903–1904
Centers for Medicare & Medicaid Services (2020) Women’s Health and Cancer Rights Act (WHCRA). https://www.cms.gov/cciio/programs-and-initiatives/other-insurance-protections/whcra_factsheet. Accessed 14 Oct 2023
Banegas M, Guy GJ, de Moor J et al (2016) For working-age cancer survivors, medical debt and bankruptcy create financial hardships. Health Aff 35(1):54–61
Meneses K, Azuero A, Hassey L, McNees P, Isu M (2012) Does economic burden influence quality of life in breast cancer survivors? Gyn Onc 124(3):437–443
Obeng-Gyasi S, Timsina L, Bhattacharyya O, Fisher C, Haggstrom D (2021) Bankruptcy among insured surgical patients with breast cancer: who is at risk? Cancer 127(12):2083–2090
Haque Q, Ahmadzada M, Janumpally S et al (2022) Adherence to a Federal Hospital price transparency rule and associated financial and marketplace factors. JAMA 327(21):2143–2145
Centers for Medicare & Medicaid Services. Hospital price transparency resources. https://www.cms.gov/priorities/key-initiatives/hospital-price-transparency. Accessed 14 Oct 2023
Jiang JX, Krishnan R, Bai G (2023) Price transparency in hospitals—current research and future directions. JAMA Netw Open 6(1):e2249588–e2249588
Department of Health and Human Services (2019) Medicare and Medicaid Programs: CY 2020 hospital outpatient PPS policy changes and payment rates and ambulatory surgical center payment system policy changes and payment rates. Price transparency requirements for hospitals to make standard charges public
Jiang J, Makary MA, Bai G (2021) Comparison of US hospital cash prices and commercial negotiated prices for 70 services. JAMA Netw Open 4(12):e2140526–e2140526
Desai S, Hatfield L, Hicks A, Chernew M, Mehrotra A (2016) Association between availability of a price transparency tool and outpatient spending. JAMA 315(17):1874–1881
Mehrotra A, Brannen T, Sinaiko A (2014) Use patterns of a state health care price transparency web site: what do patients shop for? Inquiry. https://doi.org/10.1177/0046958014561496
Sinaiko A, Rosenthal M (2016) Examining a health care price transparency tool: who uses it, and how they shop for care. Health Aff 35(4):662
Jagsi R, Ward K, Abrahamse P et al (2018) Unmet need for clinician engagement regarding financial toxicity after diagnosis of breast cancer. Cancer 124(18):3668–3676
Ho V, Offodile AC 2nd (2018) Making “Cents” for the patient: improving health care through consumerism. Baker Institute for Health Policy
Mariotto AB, Enewold L, Zhao J, Zeruto CA, Yabroff KR (2020) Medical care costs associated with cancer survivorship in the United States. Cancer Epidemiol Biomarkers Prev 29(7):1304–1312
Centers for Medicare & Medicaid Services (2021) Medicare program: hospital outpatient prospective payment and ambulatory surgical center payment systems and quality reporting programs; price transparency of hospital standard charges; radiation oncology model; request for information on rural emergency hospitals
Shah SA, Song Z (2021) Navigating hospital price transparency-a cautionary tale. J Gen Intern Med 37(5):1306–1309
Kliff S, Katz J (2021) Hospitals and insurers didn’t want you to see these prices. Here’s why. New York Times
Gilligan T, Coyle N, Frankel RM et al (2017) Patient-clinician communication: American Society of Clinical Oncology Consensus Guideline. J Clin Oncol 35(31):3618–3632
Yousuf Zafar S (2015) Financial toxicity of cancer care: it’s time to intervene. J Natl Cancer Inst 108(5):370
Offodile AC 2nd, Gallagher K, Angove R, Tucker-Seeley R, Balch A, Shankaran V (2022) Financial navigation in cancer care delivery: state of the evidence, opportunities for research, and future directions. J Clin Oncol 40(21):2291–2294
Acknowledgements
We would like to acknowledge Dr. Anaeze Offodile II, MD, MPH for his guidance and support.
Funding
No funding was used for this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors have no relevant conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Shah, S.A., Zhang, Y., Correa, A.M. et al. Rates of price disclosure associated with the surgical treatment of early-stage breast cancer one year after implementation of federal regulations. Breast Cancer Res Treat 203, 397–406 (2024). https://doi.org/10.1007/s10549-023-07160-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-023-07160-2