Abstract
Purpose
Cancer and its treatments accelerate biological aging. This analysis tested the hypothesis that exercise and diet reduce oxidative stress and prevent telomere shortening in breast cancer survivors.
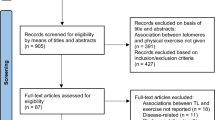
Methods
In a 2 × 2 factorial design, 342 breast cancer survivors who were insufficiently physically active and had overweight or obesity at enrollment were randomized to one of four treatment groups for 52 weeks: control, exercise alone, diet alone, or exercise plus diet. The endpoints of this analysis were the change from baseline to week 52 in 8-iso-prostaglandin F2α (8-iso-PGF2α) and lymphocyte telomere length.
Results
Baseline telomere length was shorter than age-adjusted normative values (median difference: − 1.8 kilobases; 95% CI − 2.4, − 1.1); equivalent to 21 years (95% CI 17, 25) of accelerated chronological aging. Compared to control, exercise alone did not change 8-iso-PGF2α [9.9%; 95% confidence interval (CI) − 1.0, 20.8] or telomere length (13.8%; 95% CI − 15.6, 43.3). Compared to control, diet alone was associated with reduced 8-iso-PGF2α (− 10.5%; 95% CI − 19.5, − 1.5) but did not change telomere length (12.1%; 95% CI − 17.2, 41.3). Compared to control, exercise plus diet was associated with reduced 8-iso-PGF2α (− 9.8%; 95% CI − 18.7, − 0.9) but did not change telomere length (− 8.5%; 95% CI − 32.1, 15.2). Change in 8-iso-PGF2α did not correlate with change in telomere length (r = 0.07; 95% CI − 0.07, 0.20).
Conclusion
In breast cancer survivors, diet alone or exercise plus diet were associated with reduced oxidative stress but did not change telomere length. This analysis may inform future trials that aim to optimize healthy aging in cancer survivors.
Similar content being viewed by others
Data availability
The data described in this manuscript are available upon submission of a research proposal and approval by the corresponding author.
References
Carroll JE, Bower JE, Ganz PA (2022) Cancer-related accelerated ageing and biobehavioural modifiers: a framework for research and clinical care. Nat Rev Clin Oncol 19:173–187. https://doi.org/10.1038/s41571-021-00580-3
Cupit-Link MC et al (2017) Biology of premature ageing in survivors of cancer. ESMO Open 2:e000250. https://doi.org/10.1136/esmoopen-2017-000250
Gallicchio L et al (2018) The effect of cancer treatments on telomere length: a systematic review of the literature. J Natl Cancer Inst 110:1048–1058. https://doi.org/10.1093/jnci/djy189
Blackburn EH (1991) Structure and function of telomeres. Nature 350:569–573. https://doi.org/10.1038/350569a0
Baird DM, Kipling D (2004) The extent and significance of telomere loss with age. Ann N Y Acad Sci 1019:265–268. https://doi.org/10.1196/annals.1297.044
Whittemore K et al (2019) Telomere shortening rate predicts species life span. Proc Natl Acad Sci USA 116:15122–15127. https://doi.org/10.1073/pnas.1902452116
Sanders JL, Newman AB (2013) Telomere length in epidemiology: a biomarker of aging, age-related disease, both, or neither? Epidemiol Rev 35:112–131. https://doi.org/10.1093/epirev/mxs008
Duggan C et al (2014) Change in peripheral blood leukocyte telomere length and mortality in breast cancer survivors. J Natl Cancer Inst 106:dju035. https://doi.org/10.1093/jnci/dju035
von Zglinicki T (2002) Oxidative stress shortens telomeres. Trends Biochem Sci 27:339–344. https://doi.org/10.1016/s0968-0004(02)02110-2
Houben JM et al (2008) Telomere length assessment: biomarker of chronic oxidative stress? Free Radic Biol Med 44:235–246. https://doi.org/10.1016/j.freeradbiomed.2007.10.001
Sies H, Berndt C, Jones DP (2017) Oxidative stress. Annu Rev Biochem 86:715–748. https://doi.org/10.1146/annurev-biochem-061516-045037
Cracowski JL, Durand T, Bessard G (2002) Isoprostanes as a biomarker of lipid peroxidation in humans: physiology, pharmacology and clinical implications. Trends Pharmacol Sci 23:360–366. https://doi.org/10.1016/s0165-6147(02)02053-9
Dai Q et al (2009) Oxidative stress, obesity, and breast cancer risk: results from the Shanghai Women’s Health Study. J Clin Oncol 27:2482–2488. https://doi.org/10.1200/JCO.2008.19.7970
Polidori MC et al (2000) Physical activity and oxidative stress during aging. Int J Sports Med 21:154–157. https://doi.org/10.1055/s-2000-8881
Vincent HK, Innes KE, Vincent KR (2007) Oxidative stress and potential interventions to reduce oxidative stress in overweight and obesity. Diabetes Obes Metab 9:813–839. https://doi.org/10.1111/j.1463-1326.2007.00692.x
Mundstock E et al (2015) Effects of physical activity in telomere length: Systematic review and meta-analysis. Ageing Res Rev 22:72–80. https://doi.org/10.1016/j.arr.2015.02.004
Mundstock E et al (2015) Effect of obesity on telomere length: systematic review and meta-analysis. Obesity (Silver Spring) 23:2165–2174. https://doi.org/10.1002/oby.21183
Greenlee H et al (2016) Trends in obesity prevalence in adults with a history of cancer: results from the us national health interview survey, 1997 to 2014. J Clin Oncol 34:3133–3140. https://doi.org/10.1200/JCO.2016.66.4391
Thraen-Borowski KM, Gennuso KP, Cadmus-Bertram L (2017) Accelerometer-derived physical activity and sedentary time by cancer type in the United States. PLoS One 12:e0182554. https://doi.org/10.1371/journal.pone.0182554
Garland SN et al (2014) Physical activity and telomere length in early stage breast cancer survivors. Breast Cancer Res 16:413. https://doi.org/10.1186/s13058-014-0413-y
Sanft T et al (2018) Randomized controlled trial of weight loss versus usual care on telomere length in women with breast cancer: the lifestyle, exercise, and nutrition (LEAN) study. Breast Cancer Res Treat 172:105–112. https://doi.org/10.1007/s10549-018-4895-7
Santa-Maria CA et al (2020) The effects of a remote-based weight loss program on adipocytokines, metabolic markers, and telomere length in breast cancer survivors: the POWER-remote trial. Clin Cancer Res 26:3024–3034. https://doi.org/10.1158/1078-0432.CCR-19-2935
Winkels RM et al (2017) The women in steady exercise research (WISER) survivor trial: The innovative transdisciplinary design of a randomized controlled trial of exercise and weight-loss interventions among breast cancer survivors with lymphedema. Contemp Clin Trials 61:63–72. https://doi.org/10.1016/j.cct.2017.07.017
Schmitz KH et al (2016) TREC to WHERE? Transdisciplinary research on energetics and cancer. Clin Cancer Res 22:1565–1571. https://doi.org/10.1158/1078-0432.CCR-14-1214
Schmitz KH et al (2019) Effect of home-based exercise and weight loss programs on breast cancer-related lymphedema outcomes among overweight breast cancer survivors: the wiser survivor randomized clinical trial. JAMA Oncol 5:1605–1613. https://doi.org/10.1001/jamaoncol.2019.2109
Brown JC et al (2021) A randomized trial of exercise and diet on body composition in survivors of breast cancer with overweight or obesity. Breast Cancer Res Treat 189:145–154. https://doi.org/10.1007/s10549-021-06284-7
Brown JC et al (2021) A randomized trial of exercise and diet on health-related quality of life in survivors of breast cancer with overweight or obesity. Cancer 127:3856–3864. https://doi.org/10.1002/cncr.33752
D’Alonzo NJ et al (2021) WISER survivor trial: combined effect of exercise and weight loss interventions on insulin and insulin resistance in breast cancer survivors. Nutrients. https://doi.org/10.3390/nu13093108
Health, UDo and H Services (2009) Common terminology criteria for adverse events (CTCAE) version 4.0. National Cancer Institute
Sturgeon KM et al (2018) Strategic recruitment of an ethnically diverse cohort of overweight survivors of breast cancer with lymphedema. Cancer 124:95–104. https://doi.org/10.1002/cncr.30935
Taves DR (1974) Minimization: a new method of assigning patients to treatment and control groups. Clin Pharmacol Ther 15:443–453. https://doi.org/10.1002/cpt1974155443
Campbell KL et al (2019) Exercise guidelines for cancer survivors: consensus statement from international multidisciplinary roundtable. Med Sci Sports Exerc 51:2375–2390. https://doi.org/10.1249/MSS.0000000000002116
Schmitz KH et al (2009) Weight lifting in women with breast-cancer-related lymphedema. N Engl J Med 361:664–673. https://doi.org/10.1056/NEJMoa0810118
Schmitz KH et al (2010) Weight lifting for women at risk for breast cancer-related lymphedema: a randomized trial. JAMA 304:2699–2705. https://doi.org/10.1001/jama.2010.1837
Rock CL et al (2012) Nutrition and physical activity guidelines for cancer survivors. CA Cancer J Clin 62:243–274. https://doi.org/10.3322/caac.21142
Wadden TA et al (2011) A two-year randomized trial of obesity treatment in primary care practice. N Engl J Med 365:1969–1979. https://doi.org/10.1056/NEJMoa1109220
Lee YY et al (2016) Assessment of isoprostanes in human plasma: technical considerations and the use of mass spectrometry. Lipids 51:1217–1229. https://doi.org/10.1007/s11745-016-4198-x
Milne GL et al (2007) Quantification of F2-isoprostanes as a biomarker of oxidative stress. Nat Protoc 2:221–226. https://doi.org/10.1038/nprot.2006.375
O’Callaghan N et al (2008) A quantitative real-time PCR method for absolute telomere length. Biotechniques 44:807–809. https://doi.org/10.2144/000112761
Pocock SJ, Hughes MD (1990) Estimation issues in clinical trials and overviews. Stat Med 9:657–671. https://doi.org/10.1002/sim.4780090612
Akacha M, Bretz F, Ruberg S (2017) Estimands in clinical trials—broadening the perspective. Stat Med 36:5–19. https://doi.org/10.1002/sim.7033
Ottenbacher KJ (1991) Interpretation of interaction in factorial analysis of variance design. Stat Med 10:1565–1571. https://doi.org/10.1002/sim.4780101008
McAlister FA et al (2003) Analysis and reporting of factorial trials: a systematic review. JAMA 289:2545–2553. https://doi.org/10.1001/jama.289.19.2545
Montgomery AA, Peters TJ, Little P (2003) Design, analysis and presentation of factorial randomised controlled trials. BMC Med Res Methodol 3:26. https://doi.org/10.1186/1471-2288-3-26
Fitzmaurice GM, Laird NM, Ware JH, Analysis AL (2012) Hoboken. Wiley, NJ
Rubin DB (1986) Statistical matching using file concatenation with adjusted weights and multiple imputations. J Bus Econ Stat 4:87–94. https://doi.org/10.2307/1391390
Alder JK et al (2018) Diagnostic utility of telomere length testing in a hospital-based setting. Proc Natl Acad Sci USA 115:E2358–E2365. https://doi.org/10.1073/pnas.1720427115
Guida JL et al (2019) Measuring aging and identifying aging phenotypes in cancer survivors. J Natl Cancer Inst 111:1245–1254. https://doi.org/10.1093/jnci/djz136
Guida JL et al (2021) Strategies to prevent or remediate cancer and treatment-related aging. J Natl Cancer Inst 113:112–122. https://doi.org/10.1093/jnci/djaa060
Mason C et al (2013) Independent and combined effects of dietary weight loss and exercise on leukocyte telomere length in postmenopausal women. Obesity (Silver Spring) 21:E549–E554. https://doi.org/10.1002/oby.20509
Lee JD et al (2017) The role of biomarkers of oxidative stress in breast cancer risk and prognosis: a systematic review of the epidemiologic literature. J Womens Health (Larchmt) 26:467–482. https://doi.org/10.1089/jwh.2016.5973
Duggan C et al (2016) Dietary weight loss, exercise, and oxidative stress in postmenopausal women: a randomized controlled trial. Cancer Prev Res (Phila) 9:835–843. https://doi.org/10.1158/1940-6207.CAPR-16-0163
Lohmann AE et al (2021) Association of Obesity With Breast Cancer Outcome In Relation To Cancer Subtypes: A Meta-Analysis. J Natl Cancer Inst 113:1465–1475. https://doi.org/10.1093/jnci/djab023
Ligibel JA et al (2017) Randomized phase III trial evaluating the role of weight loss in adjuvant treatment of overweight and obese women with early breast cancer (Alliance A011401): study design. NPJ Breast Cancer 3:37. https://doi.org/10.1038/s41523-017-0040-8
Fiorito G et al (2021) DNA methylation-based biomarkers of aging were slowed down in a two-year diet and physical activity intervention trial: the DAMA study. Aging Cell 20:e13439. https://doi.org/10.1111/acel.13439
Funding
This work was supported by the National Cancer Institute of the National Institutes of Health under Award Numbers U54-CA155850, UL1-TR001878, P30-CA016520, P30-CA006927. The content is solely the authors' responsibility and does not necessarily represent the official views of the National Institutes of Health. BSN Medical donated compression garments, and Nutrisystem, Inc. provided discounted meal replacements. We thank Dr. Sue Rutherford Siegel and the Biomarker Core Laboratory in the Department of Biobehavioral Health, Penn State, for telomere length analysis. Analysis of eicosanoids was performed in the Vanderbilt University Eicosanoid Core Laboratory. Dr. Brown is supported by the National Cancer Institute of the National Institutes of Health under Award Numbers R00-CA218603 and R25-CA203650, the National Institute of General Medicine Sciences of the National Institutes of Health under Award Number U54-GM104940, the National Institute of Diabetes and Digestive and Kidney Diseases of the National Institutes of Health under Award Number P30-DK072476, the Susan G. Komen Foundation, and the American Institute for Cancer Research. Dr. Sturgeon reports receiving grants from the National Institutes of Health. Dr. Sarwer is supported by the National Institute for Diabetes and Digestive and Kidney Disease of the National Institutes of Health under Award Number R01-DK108628. Dr. Sturgeon is supported by the National Center for Advancing Translational Sciences of the National Institutes of Health under Award Numbers UL1-TR002014, UL1-TR000003, and KL2-TR002015. The funding agencies had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
Conception and design of study (JCB, DBS, ABT, KS, AMD, CSD, KHS); acquisition of data (JCB, DBS, KS, AMD, CSD, KHS); analysis and/or interpretation of data (JCB, DBS, ABT, KS, KHS); drafting the manuscript (JCB, KHS); approval of the version of the manuscript to be published (JCS, DBS, ABT, KS, AMD, CSD, KHS).
Corresponding author
Ethics declarations
Conflicts of interest
Dr. Brown reports receiving grants from the National Institutes of Health, the American Institute for Cancer Research, and the Susan G. Komen Foundation. Dr. Sarwer reports receiving grants from the National Institutes of Health and personal fees from Ethicon and Novo Nordisk. Dr. Troxel reports receiving grants from the National Institutes of Health. Dr. DeMichele reports receiving grants from Novartis, Pfizer, Genentech, Calithera, and Menarini. Dr. Denlinger reports honoraria from Zymeworks for data safety and monitoring board committee work. Dr. Schmitz reports receiving grants from the National Institutes of Health, nonfinancial support from BSN Medical, personal fees from Klose Training, and a licensed patent for a Strength After Breast Cancer course. No other disclosures were reported.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Brown, J.C., Sturgeon, K., Sarwer, D.B. et al. The effects of exercise and diet on oxidative stress and telomere length in breast cancer survivors. Breast Cancer Res Treat 199, 109–117 (2023). https://doi.org/10.1007/s10549-023-06868-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-023-06868-5