Abstract
Purpose
To investigate the performance of an imaging and biopsy parameters-based multivariate model in decreasing unnecessary surgeries for high-risk breast lesions.
Methods
In an IRB-approved study, we retrospectively reviewed all high-risk lesions (HRL) identified at imaging-guided biopsy in our institution between July 1, 2014-July 1, 2017. Lesions were categorized high-risk-I (HR-I = atypical ductal hyperplasia, atypical lobular hyperplasia, lobular carcinoma in situ and atypical papillary lesion) and II (HR-II = Flat epithelial atypia, radial scar, benign papilloma). Patient risk factors, lesion features, detection and biopsy modality, excision and cancer upgrade rates were collected. Reference standard for upgrade was either excision or at least 2-year imaging follow-up. Multiple logistic regression analysis was performed to develop a multivariate model using HRL type, lesion and biopsy needle size for surgical cancer upgrade with performance assessed using ROC analysis.
Results
Of 699 HRL in 652 patients, 525(75%) had reference standard available, and 48/525(9.1%) showed cancer at surgical excision. Excision (84.5% vs 51.1%) and upgrade (17.6%vs1.8%) rates were higher in HR-I compared to HR-II (p < 0.01). In HR-I, small needle size < 12G vs ≥ 12G [32.1% vs 13.2%, p < 0.01] and less cores [< 6 vs ≥ 6, 28.6%vs13.7%, p = 0.01] were significantly associated with higher cancer upgrades. Our multivariate model had an AUC = 0.87, saving 28.1% of benign surgeries with 100% sensitivity, based on HRL subtype, lesion size(mm, continuous), needle size (< 12G vs ≥ 12G) and biopsy modality (US vs MRI vs stereotactic)
Conclusion
Our multivariate model using lesion size, needle size and patient age had a high diagnostic performance in decreasing unnecessary surgeries and shows promise as a decision support tool.

Similar content being viewed by others
Abbreviations
- HRL:
-
High-risk breast lesions
- HR-I:
-
High-risk I group
- HR-II:
-
High-risk II group
- ADH:
-
Atypical ductal hyperplasia
- ALH:
-
Atypical lobular hyperplasia
- LCIS:
-
Lobular carcinoma in situ (LCIS)
- FEA:
-
Flat epithelial atypia
- RS:
-
Radial scar
- DCIS:
-
Ductal Carcinoma in Situ
References
Morrow M, Schnitt SJ, Norton L (2015) Current management of lesions associated with an increased risk of breast cancer. Nat Rev Clin Oncol 12(4):227–238. https://doi.org/10.1038/nrclinonc.2015.8
Page DL, Dupont WD, Rogers LW, Rados MS (1985) Atypical hyperplastic lesions of the female breast. A long-term follow-up study Cancer 55(11):2698–2708
Dillon MF, McDermott EW, Hill AD, O'Doherty A, O'Higgins N, Quinn CM (2007) Predictive value of breast lesions of "uncertain malignant potential" and "suspicious for malignancy" determined by needle core biopsy. Ann Surg Oncol 14(2):704–711. https://doi.org/10.1245/s10434-006-9212-8
Mooney KL, Bassett LW, Apple SK (2016) Upgrade rates of high-risk breast lesions diagnosed on core needle biopsy: a single-institution experience and literature review. Mod Pathol 29(12):1471–1484. https://doi.org/10.1038/modpathol.2016.127
Taffurelli M, Pellegrini A, Ghignone F, Santini D, Zanotti S, Serra M (2016) Positive predictive value of breast lesions of uncertain malignant potential (B3): Can we identify high risk patients? The value of a multidisciplinary team and implications in the surgical treatment. Surg Oncol 25(2):119–122. https://doi.org/10.1016/j.suronc.2016.04.002
Murray M (2016) Pathologic High-risk Lesions, Diagnosis and Management. Clin Obstet Gynecol 59(4):727–732. https://doi.org/10.1097/grf.0000000000000234
Neal L, Sandhu NP, Hieken TJ, Glazebrook KN, Mac Bride MB, Dilaveri CA, Wahner-Roedler DL, Ghosh K, Visscher DW (2014) Diagnosis and management of benign, atypical, and indeterminate breast lesions detected on core needle biopsy. Mayo Clin Proc 89(4):536–547. https://doi.org/10.1016/j.mayocp.2014.02.004
Gao Y, Albert M, Young Lin LL, Lewin AA, Babb JS, Heller SL, Moy L (2018) What Happens after a Diagnosis of High-Risk Breast Lesion at Stereotactic Vacuum-assisted Biopsy? An Observational Study of Postdiagnosis Management and Imaging Adherence. Radiology 287(2):423–431. https://doi.org/10.1148/radiol.2017171665
Nazarali SA, Narod SA (2014) Tamoxifen for women at high risk of breast cancer. Breast Cancer 6:29–36. https://doi.org/10.2147/BCTT.S43763
Vogel VG (2009) The NSABP Study of Tamoxifen and Raloxifene (STAR) trial. Expert Rev Anticancer Ther 9(1):51–60. https://doi.org/10.1586/14737140.9.1.51
Fisher B, Costantino JP (2006) RESPONSE Re Tamoxifen for the Prevention of Breast Cancer: Current Status of the National Surgical Adjuvant Breast and Bowel Project P-1 Study. J Natl Cancer Inst 98(9):643–644. https://doi.org/10.1093/jnci/djj168
Gulla S, Lancaster R, De Los SJ (2018) High-Risk Breast Lesions and Current Management. Semin Roentgenol 53(4):252–260. https://doi.org/10.1053/j.ro.2018.08.001
Bevers TB, Helvie M, Bonaccio E, Calhoun KE, Daly MB, Farrar WB, Garber JE, Gray R, Greenberg CC, Greenup R, Hansen NM, Harris RE, Heerdt AS, Helsten T, Hodgkiss L, Hoyt TL, Huff JG, Jacobs L, Lehman CD, Monsees B, Niell BL, Parker CC, Pearlman M, Philpotts L, Shepardson LB, Smith ML, Stein M, Tumyan L, Williams C, Bergman MA, Kumar R (2018) Breast Cancer Screening and Diagnosis, Version 32018, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw 16(11):1362–1389. https://doi.org/10.6004/jnccn.2018.0083
Surgeons TASoB (2016) Consensus Guideline on Concordance Assessment of Image-Guided Breast Biopsies and Management of Borderline or High-Risk Lesions
Rageth CJ, O'Flynn EAM, Pinker K, Kubik-Huch RA, Mundinger A, Decker T, Tausch C, Dammann F, Baltzer PA, Fallenberg EM, Foschini MP, Dellas S, Knauer M, Malhaire C, Sonnenschein M, Boos A, Morris E, Varga Z (2019) Second International Consensus Conference on lesions of uncertain malignant potential in the breast B3 lesions. Breast Cancer Res Treat 174 (2): 279–296. doi:https://doi.org/10.1007/s10549-018-05071-1
Falomo E, Adejumo C, Carson KA, Harvey S, Mullen L, Myers K (2019) Variability in the Management Recommendations Given for High-risk Breast Lesions Detected on Image-guided Core Needle Biopsy at US Academic Institutions. Curr Probl Diagn Radiol 48(5):462–466. https://doi.org/10.1067/j.cpradiol.2018.06.004
Foster MC, Helvie MA, Gregory NE, Rebner M, Nees AV, Paramagul C (2004) Lobular carcinoma in situ or atypical lobular hyperplasia at core-needle biopsy: is excisional biopsy necessary? Radiology 231(3):813–819. https://doi.org/10.1148/radiol.2313030874
Ibrahim N, Bessissow A, Lalonde L, Mesurolle B, Trop I, Lisbona A, El-Khoury M (2012) Surgical outcome of biopsy-proven lobular neoplasia: is there any difference between lobular carcinoma in situ and atypical lobular hyperplasia? AJR Am J Roentgenol 198(2):288–291. https://doi.org/10.2214/AJR.11.7212
Lamb LR, Bahl M, Hughes KS, Lehman CD (2018) Pathologic Upgrade Rates of High-Risk Breast Lesions on Digital Two-Dimensional vs Tomosynthesis Mammography. J Am Coll Surg 226(5):858–867. https://doi.org/10.1016/j.jamcollsurg.2017.12.049
Linsk A, Mehta TS, Dialani V, Brook A, Chadashvili T, Houlihan MJ, Sharma R (2018) Surgical upgrade rate of breast atypia to malignancy: An academic center's experience and validation of a predictive model. Breast J 24(2):115–119. https://doi.org/10.1111/tbj.12885
Menes TS, Rosenberg R, Balch S, Jaffer S, Kerlikowske K, Miglioretti DL (2014) Upgrade of high-risk breast lesions detected on mammography in the Breast Cancer Surveillance Consortium. Am J Surg 207(1):24–31. https://doi.org/10.1016/j.amjsurg.2013.05.014
Middleton LP, Sneige N, Coyne R, Shen Y, Dong W, Dempsey P, Bevers TB (2014) Most lobular carcinoma in situ and atypical lobular hyperplasia diagnosed on core needle biopsy can be managed clinically with radiologic follow-up in a multidisciplinary setting. Cancer Med 3(3):492–499. https://doi.org/10.1002/cam4.223
Muller KE, Roberts E, Zhao L, Jorns JM (2018) Isolated Atypical Lobular Hyperplasia Diagnosed on Breast Biopsy: Low Upgrade Rate on Subsequent Excision With Long-Term Follow-up. Arch Pathol Lab Med 142(3):391–395. https://doi.org/10.5858/arpa.2017-0155-OA
Sen LQ, Berg WA, Hooley RJ, Carter GJ, Desouki MM, Sumkin JH (2016) Core Breast Biopsies Showing Lobular Carcinoma In Situ Should Be Excised and Surveillance Is Reasonable for Atypical Lobular Hyperplasia. AJR Am J Roentgenol 207(5):1132–1145. https://doi.org/10.2214/AJR.15.15425
Shah-Khan MG, Geiger XJ, Reynolds C, Jakub JW, Deperi ER, Glazebrook KN (2012) Long-term follow-up of lobular neoplasia (atypical lobular hyperplasia/lobular carcinoma in situ) diagnosed on core needle biopsy. Ann Surg Oncol 19(10):3131–3138. https://doi.org/10.1245/s10434-012-2534-9
Rendi MH, Dintzis SM, Lehman CD, Calhoun KE, Allison KH (2012) Lobular in-situ neoplasia on breast core needle biopsy: imaging indication and pathologic extent can identify which patients require excisional biopsy. Ann Surg Oncol 19(3):914–921. https://doi.org/10.1245/s10434-011-2034-3
Murray MP, Luedtke C, Liberman L, Nehhozina T, Akram M, Brogi E (2013) Classic lobular carcinoma in situ and atypical lobular hyperplasia at percutaneous breast core biopsy: outcomes of prospective excision. Cancer 119(5):1073–1079. https://doi.org/10.1002/cncr.27841
Bahl M, Barzilay R, Yedidia AB, Locascio NJ, Yu L, Lehman CD (2018) High-Risk Breast Lesions: A Machine Learning Model to Predict Pathologic Upgrade and Reduce Unnecessary Surgical Excision. Radiology 286(3):810–818. https://doi.org/10.1148/radiol.2017170549
Pena A, Shah SS, Fazzio RT, Hoskin TL, Brahmbhatt RD, Hieken TJ, Jakub JW, Boughey JC, Visscher DW, Degnim AC (2017) Multivariate model to identify women at low risk of cancer upgrade after a core needle biopsy diagnosis of atypical ductal hyperplasia. Breast Cancer Res Treat 164(2):295–304. https://doi.org/10.1007/s10549-017-4253-1
Chen LY, Hu J, Tsang JYS, Lee MA, Ni YB, Chan SK, Tse GMK (2019) Diagnostic upgrade of atypical ductal hyperplasia of the breast based on evaluation of histopathological features and calcification on core needle biopsy. Histopathology 75(3):320–328. https://doi.org/10.1111/his.13881
Williams KE, Amin A, Hill J, Walter C, Inciardi M, Gatewood J, Redick M, Wick J, Hunt S, Winblad O (2019) Radiologic and Pathologic Features Associated With Upgrade of Atypical Ductal Hyperplasia at Surgical Excision. Acad Radiol 26(7):893–899. https://doi.org/10.1016/j.acra.2018.09.010
Masood S (2012) Why the term 'low-grade ductal carcinoma in situ' should be changed to 'borderline breast disease': diagnostic and clinical implications. Womens Health (Lond) 8(1):57–62. https://doi.org/10.2217/whe.11.88
D’Orsi CJSE, Mendelson EB, Morris EA et al (2013) ACR BI-RADS® Atlas. Breast Imaging Reporting and Data System, Reston, VA, American College of Radiology
Narod SA, Iqbal J, Giannakeas V, Sopik V, Sun P (2015) Breast Cancer Mortality After a Diagnosis of Ductal Carcinoma In Situ. JAMA Oncol 1(7):888–896. https://doi.org/10.1001/jamaoncol.2015.2510
van Seijen M, Lips EH, Thompson AM, Nik-Zainal S, Futreal A, Hwang ES, Verschuur E, Lane J, Jonkers J, Rea DW, Wesseling J, team P, (2019) Ductal carcinoma in situ: to treat or not to treat, that is the question. Br J Cancer 121(4):285–292. https://doi.org/10.1038/s41416-019-0478-6
Pilewskie M, Olcese C, Patil S, Van Zee KJ (2016) Women with Low-Risk DCIS Eligible for the LORIS Trial After Complete Surgical Excision: How Low Is Their Risk After Standard Therapy? Ann Surg Oncol 23(13):4253–4261. https://doi.org/10.1245/s10434-016-5595-3
Elshof LE, Tryfonidis K, Slaets L, van Leeuwen-Stok AE, Skinner VP, Dif N, Pijnappel RM, Bijker N, Rutgers EJ, Wesseling J (2015) Feasibility of a prospective, randomised, open-label, international multicentre, phase III, non-inferiority trial to assess the safety of active surveillance for low risk ductal carcinoma in situ - The LORD study. Eur J Cancer 51(12):1497–1510. https://doi.org/10.1016/j.ejca.2015.05.008
Hwang ES, Hyslop T, Lynch T, Frank E, Pinto D, Basila D, Collyar D, Bennett A, Kaplan C, Rosenberg S, Thompson A, Weiss A, Partridge A (2019) The COMET (Comparison of Operative versus Monitoring and Endocrine Therapy) trial: a phase III randomised controlled clinical trial for low-risk ductal carcinoma in situ (DCIS). BMJ Open 9(3):e026797. https://doi.org/10.1136/bmjopen-2018-026797
Hong YR, Song BJ, Jung SS, Kang BJ, Kim SH, Chae BJ (2016) Predictive Factors for Upgrading Patients with Benign Breast Papillary Lesions Using a Core Needle Biopsy. J Breast Cancer 19(4):410–416. https://doi.org/10.4048/jbc.2016.19.4.410
Han SH, Kim M, Chung YR, Yun B, Jang M, Kim SM, Kang E, Kim EK, Park SY (2018) Benign Intraductal Papilloma without Atypia on Core Needle Biopsy Has a Low Rate of Upgrading to Malignancy after Excision. J Breast Cancer 21(1):80–86. https://doi.org/10.4048/jbc.2018.21.1.80
Pareja F, Corben AD, Brennan SB, Murray MP, Bowser ZL, Jakate K, Sebastiano C, Morrow M, Morris EA, Brogi E (2016) Breast intraductal papillomas without atypia in radiologic-pathologic concordant core-needle biopsies: Rate of upgrade to carcinoma at excision. Cancer 122(18):2819–2827. https://doi.org/10.1002/cncr.30118
El Khoury M, Sanchez LM, Lalonde L, Trop I, David J, Mesurolle B (2017) Is the outcome at surgery different when flat epithelial atypia and lobular neoplasia are found in association at biopsy? Br J Radiol 90(1072):20160750. https://doi.org/10.1259/bjr.20160750
Hugar SB, Bhargava R, Dabbs DJ, Davis KM, Zuley M, Clark BZ (2019) Isolated Flat Epithelial Atypia on Core Biopsy Specimens Is Associated With a Low Risk of Upgrade at Excision. Am J Clin Pathol 151(5):511–515. https://doi.org/10.1093/ajcp/aqy175
Lamb LR, Bahl M, Gadd MA, Lehman CD (2017) Flat Epithelial Atypia: Upgrade Rates and Risk-Stratification Approach to Support Informed Decision Making. J Am Coll Surg 225(6):696–701. https://doi.org/10.1016/j.jamcollsurg.2017.08.022
Crystal P, Sadaf A, Bukhanov K, McCready D, O'Malley F, Helbich TH (2011) High-risk lesions diagnosed at MRI-guided vacuum-assisted breast biopsy: can underestimation be predicted? Eur Radiol 21(3):582–589. https://doi.org/10.1007/s00330-010-1949-6
McCroskey Z, Sneige N, Herman CR, Miller RA, Venta LA, Ro JY, Schwartz MR, Ayala AG (2018) Flat epithelial atypia in directional vacuum-assisted biopsy of breast microcalcifications: surgical excision may not be necessary. Mod Pathol 31(7):1097–1106. https://doi.org/10.1038/s41379-018-0035-5
Khoumais NA, Scaranelo AM, Moshonov H, Kulkarni SR, Miller N, McCready DR, Youngson BJ, Crystal P, Done SJ (2013) Incidence of breast cancer in patients with pure flat epithelial atypia diagnosed at core-needle biopsy of the breast. Ann Surg Oncol 20(1):133–138. https://doi.org/10.1245/s10434-012-2591-0
Peres A, Barranger E, Becette V, Boudinet A, Guinebretiere JM, Cherel P (2012) Rates of upgrade to malignancy for 271 cases of flat epithelial atypia (FEA) diagnosed by breast core biopsy. Breast Cancer Res Treat 133(2):659–666. https://doi.org/10.1007/s10549-011-1839-x
Sohn V, Porta R, Brown T (2011) Flat epithelial atypia of the breast on core needle biopsy: an indication for surgical excision. Mil Med 176(11):1347–1350. https://doi.org/10.7205/milmed-d-11-00088
Farshid G, Buckley E (2019) Meta-analysis of upgrade rates in 3163 radial scars excised after needle core biopsy diagnosis. Breast Cancer Res Treat 174(1):165–177. https://doi.org/10.1007/s10549-018-5040-3
Li Z, Ranade A, Zhao C (2016) Pathologic findings of follow-up surgical excision for radial scar on breast core needle biopsy. Hum Pathol 48:76–80. https://doi.org/10.1016/j.humpath.2015.06.028
Weiss JB, Do WS, Forte DM, Sheldon RR, Childers CK, Sohn VY (2019) Is bigger better? Twenty-year institutional experience of atypical ductal hyperplasia discovered by core needle biopsy. Am J Surg 217(5):906–909. https://doi.org/10.1016/j.amjsurg.2019.01.028
Sippo DA, Burk KS, Mercaldo SF, Rutledge GM, Edmonds C, Guan Z, Hughes KS, Lehman CD (2019) Performance of Screening Breast MRI across Women with Different Elevated Breast Cancer Risk Indications. Radiology 292(1):51–59. https://doi.org/10.1148/radiol.2019181136
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
See Table
5,
6,
7,
8,
9,
10.
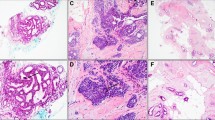
See Fig.
2.
Rights and permissions
About this article
Cite this article
Polat, D.S., Schopp, J.G., Arjmandi, F. et al. Performance of a clinical and imaging-based multivariate model as decision support tool to help save unnecessary surgeries for high-risk breast lesions. Breast Cancer Res Treat 185, 479–494 (2021). https://doi.org/10.1007/s10549-020-05947-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-020-05947-1