Abstract
Purpose
Breast cancer that overexpresses the human epidermal growth factor receptor-2 (HER2) and both estrogen (ER) and progesterone (PR) receptors is recently recognized as a subtype (triple-positive) with distinctive behavior and response to treatment. In this study, we investigate the treatment outcomes and the beneficial effect of anti-HER2 treatment in relation to level of hormone-receptor (HR) expression.
Methods
Consecutive breast cancer patients with triple-positive disease, diagnosed, treated and followed at our institution between 2006 and 2016 were enrolled. Disease-free survival (DFS) was studied in relation to the level of HR-positivity.
Results
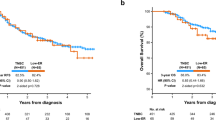
During the study period, a total of 312 were enrolled; median age (range) was 47 (20–83) years. Fifty (16.0%) of the enrolled patients received adjuvant chemotherapy without trastuzumab (cohort A). All remaining patients were treated with both chemotherapy and trastuzumab and were divided into two groups: Cohort B with both ER and PR scores ≥ 50% (n = 130, 41.7%) and Cohort C with ER and/or PR < 50% (n = 132, 42.3%). After a median follow-up of 47 months, 14 (28.0%), 30 (23.1%) and 20 (15.2%) patients in cohorts A, B, and C had an event in a form of local/system relapse or death while disease-free. The estimated 5-year DFS was 56.2%, 75.4%, and 80.8%, respectively, and at 7 year was 56.2%, 67.1%, and 78.0%, respectively (p < 0.001).
Conclusions
HER2-positive tumors are not homogeneous; stronger ER/PR co-expression may weaken the beneficial effect of anti-HER2 therapy. Such findings may have potential implication on modifying anti-HER2 treatment based on the strength of HR expression.


Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AC:
-
Adriamycin and cyclophosphamide
- ASCO:
-
American Society of Clinical Oncology
- BCS:
-
Breast-conserving surgery
- BMI:
-
Body mass index
- CAP:
-
College of American Pathologists
- CPG:
-
Clinical practice guidelines
- DCIS:
-
Ductal carcinoma in situ
- DFS:
-
Disease-free survival
- ER:
-
Estrogen receptor
- FISH:
-
Fluorescence in situ hybridization
- HER2:
-
Human epidermal growth factor receptor-2
- HR:
-
Hormone receptor
- IHC:
-
Immune histochemical staining
- IRB:
-
Institutional Review Board
- MRM:
-
Modified radical mastectomy
- PR:
-
Progesterone receptor
- LCIS:
-
Lobular carcinoma in situ
- LVI:
-
Lymphovascular invasion
- OS:
-
Overall survival
- TPBC:
-
Triple-positive breast cancer
References
Prat A, Baselga J (2008) The role of hormonal therapy in the management of hormonal-receptor-positive breast cancer with co-expression of HER2. Nat Clin Pract Oncol 5:531–542. https://doi.org/10.1038/ncponc1179
Henry NL, Somerfield MR, Abramson VG et al (2016) Role of patient and disease factors in adjuvant systemic therapy decision making for early-stage, operable breast cancer: American Society of Clinical Oncology endorsement of cancer care Ontario guideline recommendations. J Clin Oncol 34:2303–2311. https://doi.org/10.1200/JCO.2015.65.8609
Gutierrez C, Schiff R (2011) HER2: biology, detection, and clinical implications. Arch Pathol Lab Med 135:55–62. https://doi.org/10.1043/2010-0454-RAR.1
Cortes J, Saura C, Bellet M, Munoz-Couselo E, Ramirez-Merino N, Calvo V, Perez J, Vidal M (2011) HER2 and hormone receptor-positive breast cancer–blocking the right target. Nat Rev Clin Oncol 8:307–311
Untch M, Fasching PA, Konecny GE, Hasmuller S, Lebeau A, Kreienberg R, Camara O, Muller V, du Bois A, Kuhn T, Stickeler E, Harbeck N, Hoss C, Kahlert S, Beck T, Fett W, Mehta KM, von Minckwitz G, Loibl S (2011) Pathologic complete response after neoadjuvant chemotherapy plus trastuzumab predicts favorable survival in human epidermal growth factor receptor 2-overexpressing breast cancer: results from the TECHNO trial of the AGO and GBG study groups. J Clin Oncol 29:3351–3357. https://doi.org/10.1200/JCO.2010.31.4930
Giuliano M, Trivedi MV, Schiff R (2013) Bidirectional crosstalk between the estrogen receptor and human epidermal growth factor receptor 2 signaling pathways in breast cancer: molecular basis and clinical implications. Breast Care (Basel) 8:256–262. https://doi.org/10.1159/000354253
De Laurentiis M, Arpino G, Massarelli E, Ruggiero A, Carlomagno C, Ciardiello F, Tortora G, D’Agostino D, Caputo F, Cancello G, Montagna E, Malorni L, Zinno L, Lauria R, Bianco AR, De Placido S (2005) A meta-analysis on the interaction between HER-2 expression and response to endocrine treatment in advanced breast cancer. Clin Cancer Res 11:4741–4748. https://doi.org/10.1158/1078-0432.CCR-04-2569
Iancu G, Vasile D, Iancu RC, Daviţoiu DV (2017) “Triple positive” breast cancer—a novel category? Rom J Morphol Embryol 58:21–26
Vici P, Pizzuti L, Sperduti I, Frassoldati A, Natoli C, Gamucci T, Tomao S, Michelotti A, Moscetti L, Gori S, Baldini E, Giotta F, Cassano A, Santini D, Giannarelli D, Di Lauro L, Corsi DC, Marchetti P, Sini V, Sergi D, Barba M, Maugeri-Saccà M, Russillo M, Mentuccia L, D’Onofrio L, Iezzi L, Scinto AF, Da Ros L, Bertolini I, Basile ML, Rossi V, De Maria R, Montemurro F (2016) “Triple positive” early breast cancer: an observational multicenter retrospective analysis of outcome. Oncotarget 7:17932–17944. https://doi.org/10.18632/oncotarget.7480
You SH, Chae BJ, Eom YH, Yoo TK, Kim YS, Kim JS, Park WC (2018) Clinical differences in triple-positive operable breast cancer subtypes in Korean patients: an analysis of Korean breast cancer registry data. J Breast Cancer 21:415–424. https://doi.org/10.4048/jbc.2018.21.e53
Montemurro F, Di Cosimo S, Arpino G (2013) Human epidermal growth factor receptor 2 (HER2)-positive and hormone receptor-positive breast cancer: new insights into molecular interactions and clinical implications. Ann Oncol 24:2715–2724. https://doi.org/10.1093/annonc/mdt287
Allison KH, Hammond MEH, Dowsett M, McKernin SE, Carey LA, Fitzgibbons PL, Hayes DF, Lakhani SR, Chavez-MacGregor M, Perlmutter J, Perou CM, Regan MM, Rimm DL, Symmans WF, Torlakovic EE, Varella L, Viale G, Weisberg TF, McShane LM, Wolff AC (2020) Estrogen and progesterone receptor testing in breast cancer: ASCO/CAP guideline update. J Clin Oncol 38:1346–1366. https://doi.org/10.1200/JCO.19.02309
Wang Y-C, Morrison G, Gillihan R, Guo J, Ward RM, Fu X, Botero MF, Healy NA, Hilsenbeck SG, Phillips GL, Chamness GC, Rimawi MF, Osborne CK, Schiff R (2011) Different mechanisms for resistance to trastuzumab versus lapatinib in HER2-positive breast cancers—role of estrogen receptor and HER2 reactivation. Breast Cancer Res 13:R121. https://doi.org/10.1186/bcr3067
Pizzuti L, Krasniqi E, Barchiesi G, Della Giulia M, Izzo F, Sanguineti G et al (2020) Distinct HR expression patterns significantly affect the clinical behavior of metastatic HER2+ breast cancer and degree of benefit from novel anti-HER2 agents in the real world setting. Int J Cancer 146:1917–1929. https://doi.org/10.1002/ijc.32583
Schedin TB, Borges VF, Shagisultanova E (2018) Overcoming therapeutic resistance of triple positive breast cancer with CDK4/6 inhibition. Int J Breast Cancer. https://doi.org/10.1155/2018/7835095
Weiser MR, Montgomery LL, Tan LK, Susnik B, Leung DYH, Borgen PI, Cody HS (2001) Lymphovascular invasion enhances the prediction of non-sentinel node metastases in breast cancer patients with positive sentinel nodes. Ann Surg Oncol 8:145–149. https://doi.org/10.1007/s10434-001-0145-y
Hamy A-S, Lam G-T, Laas E, Darrigues L, Balezeau T, Guerin J, Livartowski A, Sadacca B, Pierga J-Y, Vincent-Salomon A (2018) Lymphovascular invasion after neoadjuvant chemotherapy is strongly associated with poor prognosis in breast carcinoma. Breast Cancer Res Treat 169:295–304
Krishnamurti U, Wetherilt CS, Yang J, Peng L, Li X (2017) Tumor-infiltrating lymphocytes are significantly associated with better overall survival and disease-free survival in triple-negative but not estrogen receptor–positive breast cancers. Hum Pathol 64:7–12
Van Calster B, Vanden Bempt I, Drijkoningen M, Pochet N, Cheng J, Van Huffel S, Hendrickx W, Decock J, Huang H-J, Leunen K, Amant F, Berteloot P, Paridaens R, Wildiers H, Van Limbergen E, Weltens C, Timmerman D, Van Gorp T, Smeets A, Van den Bogaert W, Vergote I, Christiaens M-R, Neven P (2009) Axillary lymph node status of operable breast cancers by combined steroid receptor and HER-2 status: triple positive tumours are more likely lymph node positive. Breast Cancer Res Treat 113:181–187. https://doi.org/10.1007/s10549-008-9914-7
Alzahrani W, Althoubaity F, Alsobhi D, Mohamed Y, AlMutairi A, Sindi D, Alharbi R, Zaidi N (2019) Clinicopathological features and metastatic pattern of triple-positive breast cancer among female patients at a tertiary care hospital. Cureus 11:e6458. https://doi.org/10.7759/cureus.6458
Gershon N, Berchenko Y, Hall PS, Goldstein DA (2019) Cost effectiveness and affordability of trastuzumab in sub-Saharan Africa for early stage HER2-positive breast cancer. Cost Eff Resour Alloc 17:5. https://doi.org/10.1186/s12962-019-0174-7
Cameron D, Piccart-Gebhart MJ, Gelber RD, Procter M, Goldhirsch A, de Azambuja E, Castro G Jr, Untch M, Smith I, Gianni L, Baselga J, Al-Sakaff N, Lauer S, McFadden E, Leyland-Jones B, Bell R, Dowsett M, Jackisch C (2017) 11 years’ follow-up of trastuzumab after adjuvant chemotherapy in HER2-positive early breast cancer: final analysis of the HERceptin adjuvant (HERA) trial. Lancet 389:1195–1205. https://doi.org/10.1016/S0140-6736(16)32616-2
Earl HM, Hiller L, Vallier A-L, Loi S, McAdam K, Hughes-Davies L et al (2019) 6 versus 12 months of adjuvant trastuzumab for HER2-positive early breast cancer (PERSEPHONE): 4-year disease-free survival results of a randomised phase 3 non-inferiority trial. Lancet 393:2599–2612. https://doi.org/10.1016/S0140-6736(19)30650-6
Joensuu H, Bono P, Kataja V, Alanko T, Kokko R, Asola R, Utriainen T, Turpeenniemi-Hujanen T, Jyrkkiö S, Möykkynen K, Helle L, Ingalsuo S, Pajunen M, Huusko M, Salminen T, Auvinen P, Leinonen H, Leinonen M, Isola J, Kellokumpu-Lehtinen P-L (2009) Fluorouracil, epirubicin, and cyclophosphamide with either docetaxel or vinorelbine, with or without trastuzumab, as adjuvant treatments of breast cancer: final results of the FinHer trial. J Clin Oncol 27:5685–5692. https://doi.org/10.1200/JCO.2008.21.4577
Purmonen TT, Pänkäläinen E, Turunen JHO, Asseburg C, Martikainen JA (2011) Short-course adjuvant trastuzumab therapy in early stage breast cancer in Finland: cost-effectiveness and value of information analysis based on the 5-year follow-up results of the FinHer trial. Acta Oncol (Madr) 50:344–352. https://doi.org/10.3109/0284186X.2011.553841
Neyt M, Huybrechts M, Hulstaert F, Vrijens F, Ramaekers D (2008) Trastuzumab in early stage breast cancer: a cost-effectiveness analysis for Belgium. Health Policy 87:146–159. https://doi.org/10.1016/j.healthpol.2007.11.003
Rimawi MF, Cecchini RS, Rastogi P, Geyer CE, Fehrenbacher L, Stella PJ, Dayao Z, Rabinovitch R, Dyar SH, Flynn PJ, Baez-Diaz L, Paik S, Swain SM, Mamounas EP, Osborne CK, Wolmark N (2017) Abstract S3-06: a phase III trial evaluating pCR in patients with HR+, HER2-positive breast cancer treated with neoadjuvant docetaxel, carboplatin, trastuzumab, and pertuzumab (TCHP) +/− estrogen deprivation: NRG Oncology/NSABP B-52. Cancer Res. https://doi.org/10.1158/1538-7445.SABCS16-S3-06
Llombart-Cussac A, Cortés J, Paré L, Galván P, Bermejo B, Martínez N, Vidal M, Pernas S, López R, Muñoz M, Nuciforo P, Morales S, Oliveira M, de la Peña L, Peláez A, Prat A (2017) HER2-enriched subtype as a predictor of pathological complete response following trastuzumab and lapatinib without chemotherapy in early-stage HER2-positive breast cancer (PAMELA): an open-label, single-group, multicentre, phase 2 trial. Lancet Oncol 18:545–554. https://doi.org/10.1016/S1470-2045(17)30021-9
Kaufman B, Mackey JR, Clemens MR, Bapsy PP, Vaid A, Wardley AM, Tjulandin S, Jahn M, Lehle M, Feyereislova A, Révil C, Jones A (2009) Trastuzumab plus anastrozole versus anastrozole alone for the treatment of postmenopausal women with human epidermal growth factor receptor 2-positive, hormone receptor-positive metastatic breast cancer: results from the randomized phase III TAnDEM study. J Clin Oncol. https://doi.org/10.1200/JCO.2008.20.6847
von Minckwitz G, Procter M, de Azambuja E, Zardavas D, Benyunes M, Viale G, Suter T, Arahmani A, Rouchet N, Clark E, Knott A, Lang I, Levy C, Yardley DA, Bines J, Gelber RD, Piccart M, Baselga J, APHINITY Steering Committee, and Investigators (2017) Adjuvant pertuzumab and trastuzumab in early HER2-positive breast cancer. N Engl J Med 377(2):122–131
Zambelli A, Pappagallo G, Marchetti P (2020) Adding pertuzumab to adjuvant therapy for high-risk HER2-positive early breast cancer in APHINITY: a GRADE analysis. J Comp Eff Res 9(6):423–430. https://doi.org/10.2217/cer-2019-0168
Curigliano G, Burstein HJ, Winer EP, Gnant M, Dubsky P, Loibl S, Colleoni M, Regan MM, Piccart-Gebhart M, Senn HJ, Thürlimann B, André F, Baselga J, Bergh J, Bonnefoi H, Brucker SY, Cardoso F, Carey L, Ciruelos E, Cuzick J, Denkert C, Di Leo A, Ejlertsen B, Francis P, Galimberti V, Garber J, Gulluoglu B, Goodwin P, Harbeck N, Hayes DF, Huang CS, Huober J, Khaled H, Jassem J, Jiang Z, Karlsson P, Morrow M, Orecchia R, Osborne KC, Pagani O, Partridge AH, Pritchard K, Ro J, Rutgers EJT, Sedlmayer F, Semiglazov V, Shao Z, Smith I, Toi M, Tutt A, Viale G, Watanabe T, Whelan TJ, Xu B (2018) De-escalating and escalating treatments for early-stage breast cancer: the St. Gallen International Expert Consensus Conference on the primary therapy of early breast cancer 2017. Ann Oncol 28(8):1700–1712
Denduluri N, Chavez-MacGregor M, Telli ML, Eisen A, Graff SL, Hassett MJ, Holloway JN, Hurria A, King TA, Lyman GH, Partridge AH, Somerfield MR, Trudeau ME, Wolff AC, Giordano S (2018) Selection of optimal adjuvant chemotherapy and targeted therapy for early breast cancer: ASCO clinical practice guideline focused update. J Clin Oncol 36(23):2433–2443
von Minckwitz G, Huang CS, Mano MS, Loibl S, Mamounas EP, Untch M, Wolmark N, Rastogi P, Schneeweiss A, Redondo A, Fischer HH, Jacot W, Conlin AK, Arce-Salinas C, Wapnir IL, Jackisch C, DiGiovanna MP, Fasching PA, Crown JP, Wülfing P, Shao Z, Rota Caremoli E, Wu H, Lam LH, Tesarowski D, Smitt M, Douthwaite H, Singel SM, Geyer CE Jr, KATHERINE Investigators (2019) Trastuzumab emtansine for residual invasive HER2-positive breast cancer. N Engl J Med 380(7):617–628. https://doi.org/10.1056/NEJMoa1814017
Masuda N, Lee SJ, Ohtani S, Im YH, Lee ES, Yokota I, Kuroi K, Im SA, Park BW, Kim SB, Yanagita Y, Ohno S, Takao S, Aogi K, Iwata H, Jeong J, Kim A, Park KH, Sasano H, Ohashi Y, Toi M (2017) Adjuvant capecitabine for breast cancer after preoperative chemotherapy. N Engl J Med 376(22):2147–2159. https://doi.org/10.1056/NEJMoa1612645
Wu J, Kong R, Tian S, Li H, Wu K, Kong L (2019) Can trastuzumab emtansine be replaced by additional chemotherapy plus targeted therapy for HER2-overexpressing breast cancer patients with residual disease after neoadjuvant chemotherapy? Chin J Cancer Res 31(6):878–891. https://doi.org/10.21147/j.issn.1000-9604.2019.06.04
Alwan NAS, Mualla FH, Al Naqash M, Kathum S, Tawfiq FN, Nadhir S (2017) Clinical and pathological characteristics of triple positive breast cancer among Iraqi patients. Gulf J Oncol 1:51–60
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflicts of interest.
Ethical approval
The study was conducted in accordance with the ethical standards of the institutional research committee [King Hussein Cancer Center Institutional Review Board (IRB)] and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Because of the retrospective nature of the study and the lack of personal details of participants that compromise anonymity, consent was waived.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Abdel-Razeq, H., Edaily, S., Iweir, S. et al. Effect of level of hormone-receptor expression on treatment outcomes of “triple-positive” early-stage breast cancer. Breast Cancer Res Treat 185, 459–467 (2021). https://doi.org/10.1007/s10549-020-05942-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-020-05942-6