Abstract
Purpose
The goal of this study is to evaluate the influence of shoulder exercises with restricted amplitude movement (RAM) or free amplitude movement (FAM) performed from the first postoperative day (1st POD) on the incidence of surgical wound complications (SWC) in breast cancer.
Methods
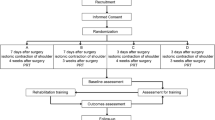
This study comprises a randomized clinical trial with an intention-to-treat analysis including 465 women aged 18 to 79, who underwent curative surgery for breast cancer. Participants were submitted to perform free amplitude movement (FAM) or restricted amplitude movement (RAM) shoulder exercises, until the 30th postoperative day. The outcome measures were the SWC: seroma, dehiscence, necrosis, infection, hematoma and bruise.
Results
461 participants completed the follow-up. Thirty days after surgery, 63.8% of the women presented some surgical wound complication, with necrosis (39.3%) and seroma (30.8%) as the most frequent. No statistically significant differences in SWC according to postoperative amplitude shoulder exercise (FAM vs RAM), even after a stratified analysis by type of surgery (segmentectomy vs mastectomy) or axillary approach (axillary lymphadenectomy versus sentinel lymph node biopsy) were observed.
Conclusion
FAM exercises do not increase the incidence of postoperative wound complications compared to RAM exercises.
Trial registration: NCT03796845

Similar content being viewed by others
References
Hoekstra HJ, Wobbes T, Heineman E, Haryono S, Aryandono T et al (2016) Fighting global disparities in cancer care: a surgical oncology view. Ann Surg Oncol 23(7):2131–2136. https://doi.org/10.1245/s10434-016-5194-3
Macedo FO, Bergmann A, Koifman RJ, Torres DM, Costa RM, Silva IF (2018) Axillary surgery in breast cancer: acute postoperative complications in a hospital cohort of women of Rio de Janeiro Brazil. Mastology 28:80–86
Glas De NA, Kiderlen M, Bastiaannet E, De Craen AJ, van de Water W, van de Velde CJ, Liefers GJ et al (2013) Postoperative complications and survival of elderly breast cancer patients: a FOCUS study analysis. Breast Cancer Res Treat;138(2):561–9. doi: 10.1007/s10549-013-2462-9.
Stan D, Loprinzi CL, Ruddy KJ (2013) Breast cancer survivorship issues. Hematol Oncol Clin N Am 27(4):805–827. https://doi.org/10.1016/j.hoc.2013.05.005
Ribeiro Pereira ACP, Koifman RJ, Bergmann A (2017) Incidence and risk factors of lymphedema after breast cancer treatment: 10 years of follow-up. Breast 36:67–73. https://doi.org/10.1016/j.breast.2017.09.006
de Carvalho FN, Bergmann A, Koifman RJ (2014) Functionality in women with breast cancer: the use of international classification of functioning, disability and health (ICF) in clinical practice. J Phys Ther Sci 26(5):721–730. https://doi.org/10.1589/jpts.26.721
Bergmann A, Mendes VV, Dias RA, Silva BA, Ferreira MGCL, Fabro EAN (2012) Incidence and risk factors for axillary web syndrome after breast cancer surgery. Breast Cancer Res Treat 131(3):987–992. https://doi.org/10.1007/s10549-011-1805-7
Springer BA, Levy E, McGarvey C, Pfalzer LA, Stout NL, Gerber LH, Soballe PW, Danoff J (2010) Pre-operative assessment enables early diagnosis and recovery of shoulder function in patients with breast cancer. Breast Cancer Res Treat 120(1):135–147. https://doi.org/10.1007/s10549-009-0710-9
Zomkowski K, de Souza BC, da Silva FP, Moreira GM, de Cunha N, Sperandio FF (2018) Physical symptoms and working performance in female breast cancer survivors: a systematic review. Disabil Rehabil 40(13):1485–1493. https://doi.org/10.1080/09638288.2017.1300950
Baima J, Reynolds SG, Edmiston K, Larkin A, Ward BM, O'Connor A (2017) Teaching of independent exercises for prehabilitation in breast cancer. J Cancer Educ 32(2):252–256. https://doi.org/10.1007/s13187-015-0940-y
de Oliveira MM, de Rezende LF, de Amaral MT, Silva MP, Morais SS, Gurgel MS (2014) Manual lymphatic drainage versus exercise in the early postoperative period for breast cancer. Physiother Theory Pract 30(6):384–389. https://doi.org/10.3109/09593985.2013.876695
Testa A, Iannace C, Di Libero L (2014) Strengths of early physical rehabilitation programs in surgical breast cancer patients: results of a randomized controlled study. Eur J Phys Rehabil Med 50(3):275–284
Rezende LF, Beletti PO, Franco RL, Moraes SS, Gurgel MSC (2006) Exercícios livres versus direcionados nas complicações pós-operatórias de câncer de mama. Rev Assoc Med Bras 52(1):37–42
Silva MPP, Derchain FM, Rezende L, Cabello C, Martinez EZ (2004) Movimento do ombro após cirurgia por carcinoma invasor da mama: estudo randomizado prospectivo controlado de exercícios livres versus limitados a 90º no pós-operatorio. Rev Bras Ginecol Obstet 26:125–130
Shamley DR, Barker K, Simonite V, Beardshaw A (2005) Delayed versus immediate exercises following surgery for breast cancer: a systematic review. Breast Cancer Res Treat 90(3):263–271
De Groef A, Van Kampen M, Dieltjens E, Christiaens MR, Neven P, Geraerts I, Devoogdt N (2015) Effectiveness of postoperative physical therapy for upper-limb impairments after breast cancer treatment: a systematic review. Arch Phys Med Rehabil 96(6):1140–1153. https://doi.org/10.1016/j.apmr.2015.01.006
McNeely ML, Campbell K, Ospina M, Rowe BH, Dabbs K, Klassen TP, Mackey J, Courneya K (2010) Exercise interventions for upper-limb dysfunction due to breast cancer treatment. Cochrane Database Syst Rev 6:CD005211. https://doi.org/10.1002/14651858.CD005211.pub2
Cinar N, Seckin U, Keskin D, Bodur H, Bozkurt B, Cengiz O (2008) The effectiveness of early rehabilitation in patients with modified radical mastectomy. Cancer Nurs 31(2):160–165. https://doi.org/10.1097/01.NCC.0000305696
Gozzo TO, Almeida AM, Panobianco MS, Brito LGO, Carrara HHA (2008) Estudo comparativo da eficácia da movimentacão precoce do braço no controle do seroma pos-linfadenectomia axilar em mulheres com câncer de mama. Rev Bras de Mastologia 18:58–62
Sampathraju S, Rodrigues G (2010) Seroma formation after mastectomy: pathogenesis and prevention. Indian J Surg Oncol 1(4):328–333. https://doi.org/10.1007/s13193-011-0067-5
Harris SR, Schmitz KH, Campbell KL, McNeely ML (2012) Clinical practice guidelines for breast cancer rehabilitation: syntheses of guideline recommendations and qualitative appraisals. Cancer 118(8 Suppl):2312–2324. https://doi.org/10.1002/cncr.27461
Tood J, Scally A, Dodwell D, Horgan K, Topping AN (2008) A randomised controlled trial of two programmes of shoulder exercise following axillary node dissection for invasive breast cancer. Physiotherapy 94(4):265–273
Petito EL, Esteves MT, Elias S, Facina G, Nazário AC, Gutiérrez MG (2014) The influence of the initiation of an exercise programme on seroma formation and dehiscence following breast cancer surgery. J Clin Nurs 23(21–22):3087–3094. https://doi.org/10.1111/jocn.12544
Lauridsen MC, Christiansen P, Hessov I (2005) The effect of physiotherapy on shoulder function in patients surgically treated for breast cancer: a randomized study. Acta Oncol 44(5):449–457
Ganz PA (2008) Psychological and social aspects of breast cancer. Oncology (Williston Park) 22(6):642–646
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The study protocol was approved by the Brazilian National Cancer Institute (INCA) Research Ethics Committee.
Informed consent
All patients were informed of the study protocol and signed an informed consent form before assessment.
Research involving human and animal participants
This article does not contain any studies with animals performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Teodózio, C.G.C., Marchito, L.d.O., Fabro, E.A.N. et al. Shoulder amplitude movement does not influence postoperative wound complications after breast cancer surgery: a randomized clinical trial. Breast Cancer Res Treat 184, 97–105 (2020). https://doi.org/10.1007/s10549-020-05826-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-020-05826-9