Abstract
Introduction
Current international guidelines, including the Choosing Wisely Initiative, recommends against the routine use of systemic imaging studies or tumor markers in early‐stage breast cancer. Accumulating data suggests that adherence to these guidelines is low. We aimed to investigate the execution of unnecessary diagnostic tests among Israeli breast cancer patients and identify factors associated with their performance.
Methods
A retrospective analysis was conducted involving a database of early breast cancer patients treated at Tel Aviv Sourasky Medical Center. A survey was distributed among Israeli surgeons and oncologists specializing in breast cancer treatment.
Results
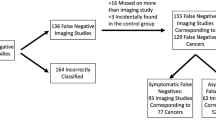
The study included early breast cancer patients (n = 178), who have no indication for completing systemic evaluation. Nearly half of the patients (76, 42%) were referred to 128 unjustified diagnostic studies, with the most common referral comprising a PET-CT (n = 39 30.5%). As expected, none of the tests led to any change in either disease staging or alteration in clinical management. Variables associated with systemic evaluation included younger age (61.8% for < 50 years vs 38.9% for > 50 years, p = 0.02), diagnosis by palpable mass compared to screening mammography (26.9% vs 52.9% p = 0.043, respectively) and higher tumor grade (33.7% vs 52.2% p = 0.02, respectively). In concordance with the findings of the database, the physicians’ survey revealed low adherence to guidelines and a role of the treating physicians’ subjective feelings. Doctors were more likely to recommend unnecessary studies when presented with a clinical case as an image, than to an informative question.
Conclusions
Our data indicate a high rate of non-adherence to guidelines, physicians recommending extensive systemic evaluation for women with early breast cancer. These deviations from the guidelines are associated with subjective factors, some of them being physician-dependent. Initiatives aimed at improving adherence to guidelines, and specifically to guidelines recommending "doing less" should therefore include not just knowledge-based education but also encourage conversation about what is appropriate and necessary.




Similar content being viewed by others
References
Ferlay J, Colombet M, Soerjomataram I et al (2019) Estimating the global cancer incidence and mortality in 2018: GLOBOCAN sources and methods. Int J Cancer 144:1941–1953. https://doi.org/10.1002/ijc.31937
Cianfrocca M, Goldstein LJ (2004) Prognostic and predictive factors in early-stage breast cancer. Oncologist 9:606–616. https://doi.org/10.1634/theoncologist.9-6-606
Goetz MP, Gradishar WJ, Anderson BO et al (2019) NCCN Guidelines Insights: Breast Cancer, Version 3.2018: Featured Updates to the NCCN Guidelines. J Natl Compr Canc Netw 17:118–126. https://doi.org/10.6004/jnccn.2019.0009
Cardoso F, Kyriakides S, Ohno S et al (2019) Early breast cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up†. Ann Oncol 30:1194–1220. https://doi.org/10.1093/annonc/mdz173
Lichter AS (2018) From choosing wisely to using wisely: increasing the value of cancer care through clinical research. J Clin Oncol 36:1387–1388. https://doi.org/10.1200/JCO.2018.78.4264
Louie RJ, Tonneson JE, Gowarty M et al (2015) Complete blood counts, liver function tests, and chest x-rays as routine screening in early-stage breast cancer: value added or just cost? Breast Cancer Res Treat 154:99–103. https://doi.org/10.1007/s10549-015-3593-y
Debald M, Wolfgarten M, Kreklau P et al (2014) Staging of primary breast cancer is not indicated in asymptomatic patients with early tumor stages. Oncol Res Treat 37:400–405. https://doi.org/10.1159/000363528
Puglisi F, Follador A, Minisini AM et al (2005) Baseline staging tests after a new diagnosis of breast cancer: further evidence of their limited indications. Ann Oncol 16:263–266. https://doi.org/10.1093/annonc/mdi063
Jm B, Km K, Rk B, Nl H (2016) Incidental radiologic findings at breast cancer diagnosis and likelihood of disease recurrence. Breast Cancer Res Treat 155:395–403. https://doi.org/10.1007/s10549-016-3687-1
Ravaioli A, Pasini G, Polselli A et al (2002) Staging of breast cancer: new recommended standard procedure. Breast Cancer Res Treat 72:53–60. https://doi.org/10.1023/A:1014900600815
Wahl RL, Siegel BA, Coleman RE et al (2004) Prospective multicenter study of axillary nodal staging by positron emission tomography in breast cancer: a report of the staging breast cancer with PET Study Group. J Clin Oncol 22:277–285. https://doi.org/10.1200/JCO.2004.04.148
Kumar R, Chauhan A, Zhuang H et al (2006) Clinicopathologic factors associated with false negative FDG–PET in primary breast cancer. Breast Cancer Res Treat 98:267–274. https://doi.org/10.1007/s10549-006-9159-2
Podoloff DA, Advani RH, Allred C et al (2007) NCCN task force report: positron emission tomography (PET)/computed tomography (CT) scanning in cancer. J Natl Compr Canc Netw 5(Suppl 1):S1–22
Brennan ME, Houssami N (2012) Evaluation of the evidence on staging imaging for detection of asymptomatic distant metastases in newly diagnosed breast cancer. Breast 21:112–123. https://doi.org/10.1016/j.breast.2011.10.005
Tanaka S, Sato N, Fujioka H et al (2012) Use of contrast-enhanced computed tomography in clinical staging of asymptomatic breast cancer patients to detect asymptomatic distant metastases. Oncol Lett 3:772–776. https://doi.org/10.3892/ol.2012.594
Chand N, Cutress RI, Oeppen RS, Agrawal A (2013) Staging investigations in breast cancer: collective opinion of UK breast surgeons. Int J Breast Cancer 2013:506172. https://doi.org/10.1155/2013/506172
Burgess C, Cornelius V, Love S et al (2005) Depression and anxiety in women with early breast cancer: five year observational cohort study. BMJ 330:702. https://doi.org/10.1136/bmj.38343.670868.D3
Mehnert A, Brähler E, Faller H et al (2014) Four-week prevalence of mental disorders in patients with cancer across major tumor entities. J Clin Oncol 32:3540–3546. https://doi.org/10.1200/JCO.2014.56.0086
Myers RE, Johnston M, Pritchard K et al (2001) Baseline staging tests in primary breast cancer: a practice guideline. CMAJ 164:1439–1444
Lavery HJ, Brajtbord JS, Levinson AW et al (2011) Unnecessary imaging for the staging of low-risk prostate cancer is common. Urology 77:274–278. https://doi.org/10.1016/j.urology.2010.07.491
Simos D, Hutton B, Clemons M (2015) Are physicians choosing wisely when imaging for distant metastases in women with operable breast cancer? J Oncol Pract 11:62–68. https://doi.org/10.1200/JOP.2014.000125
Hong J-Y, Han K, Jung J-H, Kim JS (2019) Association of exposure to diagnostic low-dose ionizing radiation with risk of cancer among youths in South Korea. JAMA Netw Open 2:e1910584–e1910584. https://doi.org/10.1001/jamanetworkopen.2019.10584
Fredholm H, Eaker S, Frisell J et al (2009) Breast cancer in young women: poor survival despite intensive treatment. PLoS ONE 4:e7695. https://doi.org/10.1371/journal.pone.0007695
Anders CK, Johnson R, Litton J et al (2009) Breast cancer before age 40 years. Semin Oncol 36:237–249. https://doi.org/10.1053/j.seminoncol.2009.03.001
Partridge AH, Hughes ME, Warner ET et al (2016) Subtype-dependent relationship between young age at diagnosis and breast cancer survival. J Clin Oncol 34:3308–3314. https://doi.org/10.1200/JCO.2015.65.8013
Levinson W, Kallewaard M, Bhatia RS et al (2015) “Choosing Wisely”: a growing international campaign. BMJ Qual Saf 24:167–174. https://doi.org/10.1136/bmjqs-2014-003821
Detsky AS, Verma AA (2012) A new model for medical education: celebrating restraint. JAMA 308:1329–1330. https://doi.org/10.1001/2012.jama.11869
Lakhani A, Lass E, Silverstein WK et al (2016) Choosing wisely for medical education: six things medical students and trainees should question. Acad Med 91:1374–1378. https://doi.org/10.1097/ACM.0000000000001325
Funding
This study was not funded.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All author declare no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Aks, R., Peleg Hasson, S., Sivan, A. et al. Diagnostic workup of early-stage breast cancer: can we choose more wisely?. Breast Cancer Res Treat 183, 741–748 (2020). https://doi.org/10.1007/s10549-020-05813-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-020-05813-0