Abstract
Purpose
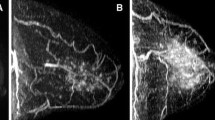
Breast fibroglandular tissue (FGT), as visualized on a mammogram (mammographic density, MD), is one of the strongest known risk factors for breast cancer. FGT is also visible on breast MRI, and increased background parenchymal enhancement (BPE) in the FGT has been identified as potentially a major breast cancer risk factor. The aim of this exploratory study was to examine the biologic basis of BPE.
Methods
We examined the unaffected contra-lateral breast of 80 breast cancer patients undergoing a prophylactic mastectomy before any treatment other than surgery of their breast cancer. BPE was classified on the BI-RADS scale (minimal/mild/moderate/marked). Slides were stained for microvessel density (MVD), CD34 (another measure of endothelial density), glandular tissue within the FGT and VEGF. Spearman correlations were used to evaluate the associations between BPE and these pathologic variables.
Results
In pre-menopausal patients, BPE was highly correlated with MVD, CD34 and glandular concentration within the FGT, and the pathologic variables were themselves highly correlated. The expression of VEGF was effectively confined to terminal duct lobular unit (TDLU) epithelium. The same relationships of the four pathologic variables with BPE were seen in post-menopausal patients, but the relationships were much weaker and not statistically significant.
Conclusion
The strong correlation of BPE and MVD together with the high correlation of MVD with glandular concentration seen in pre-menopausal patients indicates that increased breast cancer risk associated with BPE in pre-menopausal women is likely to result from its association with increased concentration of glandular tissue in the FGT. The effective confinement of VEGF expression to the TDLUs shows that the signal for MVD growth arises directly from the glandular tissue. Further studies are needed to understand the basis of BPE in post-menopausal women.


Similar content being viewed by others
Abbreviations
- ACR:
-
American College of Radiology
- BI-RADS:
-
Breast Imaging Reporting and Data System
- BPE:
-
Background parenchymal enhancement
- FGT:
-
Fibroglandular tissue
- IHC:
-
Immunohistochemistry
- MD:
-
Mammographic density
- MRI:
-
Magnetic resonance imaging
- MSK:
-
Memorial Sloan Kettering Cancer Center
- MVD:
-
Microvessel density
- TDLU:
-
Terminal duct lobular unit
- VEGF:
-
Vascular endothelial growth factor
References
McCormack VA, dos Santos Silva I (2006) Breast density and parenchymal patterns as markers of breast cancer risk: a meta-analysis. Cancer Epidemiol Biomark Prev 15(6):1159–1169. https://doi.org/10.1158/1055-9965.epi-06-0034
Morris EA (2010) Diagnostic breast MR imaging: current status and future directions. Magn Reson Imaging Clin N Am 18(1):57–74. https://doi.org/10.1016/j.mric.2009.09.005
King V, Brooks JD, Bernstein JL, Reiner AS, Pike MC, Morris EA (2011) Background parenchymal enhancement at breast MR imaging and breast cancer risk. Radiology 260(1):50–60. https://doi.org/10.1148/radiol.11102156
Dontchos BN, Rahbar H, Partridge SC, Korde LA, Lam DL, Scheel JR, Peacock S, Lehman CD (2015) Are qualitative assessments of background parenchymal enhancement, amount of fibroglandular tissue on MR images, and mammographic density associated with breast cancer risk? Radiology 276(2):371–380. https://doi.org/10.1148/radiol.2015142304
Telegrafo M, Rella L, Stabile Ianora AA, Angelelli G, Moschetta M (2016) Breast MRI background parenchymal enhancement (BPE) correlates with the risk of breast cancer. Magn Reson Imaging 34(2):173–176. https://doi.org/10.1016/j.mri.2015.10.014
Wu S, Berg WA, Zuley ML, Kurland BF, Jankowitz RC, Nishikawa R, Gur D, Sumkin JH (2016) Breast MRI contrast enhancement kinetics of normal parenchyma correlate with presence of breast cancer. Breast Cancer Res 18(1):76. https://doi.org/10.1186/s13058-016-0734-0
Grimm LJ, Saha A, Ghate SV, Kim C, Soo MS, Yoon SC, Mazurowski MA (2018) Relationship between background parenchymal enhancement on high-risk screening MRI and future breast cancer risk. Acad Radiol. https://doi.org/10.1016/j.acra.2018.03.013
Bennani-Baiti B, Dietzel M, Baltzer PA (2016) MRI background parenchymal enhancement is not associated with breast cancer. PLoS ONE 11(7):e0158573. https://doi.org/10.1371/journal.pone.0158573
Hansen NL, Kuhl CK, Barabasch A, Strobel K, Schrading S (2014) Does MRI breast “density” (degree of background enhancement) correlate with mammographic breast density? J Magn Reson Imaging 40(2):483–489. https://doi.org/10.1002/jmri.24495
King V, Gu Y, Kaplan JB, Brooks JD, Pike MC, Morris EA (2012) Impact of menopausal status on background parenchymal enhancement and fibroglandular tissue on breast MRI. Eur Radiol 22(12):2641–2647. https://doi.org/10.1007/s00330-012-2553-8
Scaranelo AM, Carrillo MC, Fleming R, Jacks LM, Kulkarni SR, Crystal P (2013) Pilot study of quantitative analysis of background enhancement on breast MR images: association with menstrual cycle and mammographic breast density. Radiology 267(3):692–700. https://doi.org/10.1148/radiol.13120121
King V, Kaplan J, Pike MC, Liberman L, David Dershaw D, Lee CH, Brooks JD, Morris EA (2012) Impact of tamoxifen on amount of fibroglandular tissue, background parenchymal enhancement, and cysts on breast magnetic resonance imaging. Breast J 18(6):527–534. https://doi.org/10.1111/tbj.12002
King V, Goldfarb SB, Brooks JD, Sung JS, Nulsen BF, Jozefara JE, Pike MC, Dickler MN, Morris EA (2012) Effect of aromatase inhibitors on background parenchymal enhancement and amount of fibroglandular tissue at breast MR imaging. Radiology 264(3):670–678. https://doi.org/10.1148/radiol.12112669
Mousa NA, Eiada R, Crystal P, Nayot D, Casper RF (2012) The effect of acute aromatase inhibition on breast parenchymal enhancement in magnetic resonance imaging: a prospective pilot clinical trial. Menopause 19(4):420–425. https://doi.org/10.1097/gme.0b013e31823772a8
Pfleiderer S, Sachse S, Sauner D, Marx C, Malich A, Wurdinger S, Kaiser W (2004) Changes in magnetic resonance mammography due to hormone replacement therapy. Breast Cancer Res 6(3):R232 R238
Delille J-P, Slanetz PJ, Yeh ED, Kopans DB, Halpern EF, Garrido L (2005) Hormone replacement therapy in postmenopausal women: breast tissue perfusion determined with MR imaging—initial observations. Radiology 235(1):36–41. https://doi.org/10.1148/radiol.2351040012
Reichenbach JR, Przetak C, Klinger G, Kaiser WA (1999) Assessment of breast tissue changes on hormonal replacement therapy using MRI: a pilot study. J Comput Assist Tomogr 23(3):407–413
Prentice RL, Chlebowski RT, Stefanick ML, Manson JE, Langer RD, Pettinger M, Hendrix SL, Hubbell FA, Kooperberg C, Kuller LH, Lane DS, McTiernan A, O’Sullivan MJ, Rossouw JE, Anderson GL (2008) Conjugated equine estrogens and breast cancer risk in the Women’s Health Initiative clinical trial and observational study. Am J Epidemiol 167(12):1407–1415. https://doi.org/10.1093/aje/kwn090
Lewin AA, Kim SG, Babb JS, Melsaether AN, McKellop J, Moccaldi M, Klautau Leite AP, Moy L (2016) Assessment of background parenchymal enhancement and lesion kinetics in breast MRI of BRCA 1/2 mutation carriers compared to matched controls using quantitative kinetic analysis. Acad Radiol 23(3):358–367. https://doi.org/10.1016/j.acra.2015.11.011
DeMartini WB, Liu F, Peacock S, Eby PR, Gutierrez RL, Lehman CD (2012) Background parenchymal enhancement on breast MRI: impact on diagnostic performance. AJR Am J Roentgenol 198(4):W373–W380. https://doi.org/10.2214/AJR.10.6272
Howe LR, Subbaramaiah K, Hudis CA, Dannenberg AJ (2013) Molecular pathways: adipose inflammation as a mediator of obesity-associated cancer. Clin Cancer Res 19(22):6074–6083. https://doi.org/10.1158/1078-0432.CCR-12-2603
Simpson ER, Brown KA (2013) Obesity and breast cancer: role of inflammation and aromatase. J Mol Endocrinol 51(3):T51–T59. https://doi.org/10.1530/JME-13-0217
Fina L, Molgaard HV, Robertson D, Bradley NJ, Monaghan P, Delia D, Sutherland DR, Baker MA, Greaves MF (1990) Expression of the CD34 gene in vascular endothelial cells. Blood 75(12):2417–2426
Matsumoto K, Ema M (2014) Roles of VEGF-A signalling in development, regeneration, and tumours. J Biochem 156(1):1–10. https://doi.org/10.1093/jb/mvu031
Sobolewski C, Cerella C, Dicato M, Ghibelli L, Diederich M (2010) The role of cyclooxygenase-2 in cell proliferation and cell death in human malignancies. Int J Cell Biol. https://doi.org/10.1155/2010/215158
Travis MA, Sheppard D (2014) TGF-beta activation and function in immunity. Annu Rev Immunol 32:51–82. https://doi.org/10.1146/annurev-immunol-032713-120257
Morris PG, Hudis CA, Giri D, Morrow M, Falcone DJ, Zhou XK, Du B, Brogi E, Crawford CB, Kopelovich L, Subbaramaiah K, Dannenberg AJ (2011) Inflammation and increased aromatase expression occur in the breast tissue of obese women with breast cancer. Cancer Prev Res 4(7):1021–1029. https://doi.org/10.1158/1940-6207.CAPR-11-0110
Camerlingo R, Ferraro GA, De Francesco F, Romano M, Nicoletti G, Di Bonito M, Rinaldo M, D’Andrea F, Pirozzi G (2014) The role of CD44+/CD24-/low biomarker for screening, diagnosis and monitoring of breast cancer. Oncol Rep 31(3):1127–1132. https://doi.org/10.3892/or.2013.2943
Delille JP, Slanetz PJ, Yeh ED, Kopans DB, Garrido L (2005) Physiologic changes in breast magnetic resonance imaging during the menstrual cycle: perfusion imaging, signal enhancement, and influence of the T1 relaxation time of breast tissue. Breast J 11(4):236–241. https://doi.org/10.1111/j.1075-122X.2005.21499.x
Dvorak HF, Harvey VS, Estrella P, Brown LF, McDonagh J, Dvorak AM (1987) Fibrin containing gels induce angiogenesis. Implications for tumor stroma generation and wound healing. Lab Invest 57(6):673–686
Dvorak HF, Sioussat TM, Brown LF, Berse B, Nagy JA, Sotrel A, Manseau EJ, Van de Water L, Senger DR (1991) Distribution of vascular permeability factor (vascular endothelial growth factor) in tumors: concentration in tumor blood vessels. J Exp Med 174(5):1275–1278
Roberts WG, Palade GE (1995) Increased microvascular permeability and endothelial fenestration induced by vascular endothelial growth factor. J Cell Sci 108(Pt 6):2369–2379
Dellian M, Witwer BP, Salehi HA, Yuan F, Jain RK (1996) Quantitation and physiological characterization of angiogenic vessels in mice: effect of basic fibroblast growth factor, vascular endothelial growth factor/vascular permeability factor, and host microenvironment. Am J Pathol 149(1):59–71
Ferrara N, Davis-Smyth T (1997) The biology of vascular endothelial growth factor. Endocr Rev 18(1):4–25. https://doi.org/10.1210/edrv.18.1.0287
Toi M, Inada K, Suzuki H, Tominaga T (1995) Tumor angiogenesis in breast cancer: its importance as a prognostic indicator and the association with vascular endothelial growth factor expression. Breast Cancer Res Treat 36(2):193–204
Li T, Sun L, Miller N, Nicklee T, Woo J, Hulse-Smith L, Tsao MS, Khokha R, Martin L, Boyd N (2005) The association of measured breast tissue characteristics with mammographic density and other risk factors for breast cancer. Cancer Epidemiol Biomark Prev 14(2):343–349
Longacre TA, Bartow SA (1986) A correlative morphologic study of human breast and endometrium in the menstrual cycle. Am J Surg Pathol 10:382–393
Acknowledgements
We would especially like to thank all the patients who gave permission to have their tissues used for research.
Funding
This study was funded in part through the National Institutes of Health/National Cancer Institute Support Grant P30 CA008748 to Memorial Sloan Kettering Cancer Center, which also provided special support through an Interdisciplinary Population Science Research award from the Survivorship, Outcomes and Risk Development Funds within Memorial Sloan Kettering Cancer Center. Additional funding was also provided by the Susan G. Komen Foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the Memorial Sloan Kettering Cancer Center institutional national research committee and with the 1964 Helsinki declaration and its later amendments. For this type of study formal consent is not required. This article does not contain any studies with animals performed by any of the authors.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Sung, J.S., Corben, A.D., Brooks, J.D. et al. Histopathologic characteristics of background parenchymal enhancement (BPE) on breast MRI. Breast Cancer Res Treat 172, 487–496 (2018). https://doi.org/10.1007/s10549-018-4916-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-018-4916-6