Abstract
Purpose
There is a lack of real-world studies evaluating the impact on survival of an evidence-based pathway of care in breast cancer. The aim of this work is to investigate the effect of adherence to guidelines on long-term survival for a cohort of Italian breast cancer patients.
Methods
The cohort included incident female breast cancer cases (2007–12), from the registry of the Milan province (Italy), not metastatic at diagnosis and receiving primary surgery. We selected sets of indicators, according to patient and tumor characteristics. We then defined the pathway of care as adherent to guidelines if it fulfilled at least 80% of the indicators. Indicators were measured using different administrative health databases linked on a unique key. A causal inference approach was used, drawing a directed acyclic graph and fitting an inverse probability weighted marginal structural model, accounting for patient’s demographic, socioeconomic and tumor characteristics.
Results
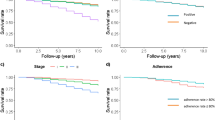
The analysis included 6333 patients, 69% of them were classified as having an adherent care. Mean age was 61 years (standard deviation, 13.6 years) and half of the patients were in Stage I (50%) at diagnosis. Median follow-up time was 5.6 years. Overall, 5-year survival was 90% (95% CI, 89–91%). The estimated risk of death was 30% lower for patients with adherent than nonadherent care (hazard ratio [HR], 0.66; 95% CI, 0.55–0.77).
Conclusions
Our study confirms, in real-world care, the impact on survival of receiving a care pathway adherent to guidelines in non-metastatic breast cancer patients.



Similar content being viewed by others
Abbreviations
- CI:
-
Confidence interval
- DAG:
-
Directed acyclic graph
- HR:
-
Hazard ratio
- IPW:
-
Inverse probability weighted
- RCT:
-
Randomized controlled trial
References
Woolf SH (1993) Practice guidelines: a new reality in medicine. III. Impact on patient care. Arch Intern Med 153:2646–2655. doi:10.1001/archinte.1993.00410230060008
Davis D (2006) Assessing and scaling the knowledge pyramid: the good-guideline guide. Can Med Assoc J 174:337–338. doi:10.1503/cmaj.051611
Berlin JA, Golub RM (2014) Meta-analysis as evidence: building a better pyramid. JAMA 312:603. doi:10.1001/jama.2014.8167
Brouwers MC, Kho ME, Browman GP et al (2010) AGREE II: advancing guideline development, reporting and evaluation in health care. CMAJ Can Med Assoc J 182:E839–E842. doi:10.1503/cmaj.090449
McMahon AD (2002) Study control, violators, inclusion criteria and defining explanatory and pragmatic trials. Stat Med 21:1365–1376. doi:10.1002/sim.1120
Mehta RH, Chen AY, Alexander KP et al (2015) Doing the right things and doing them the right way: association between hospital guideline adherence, dosing safety, and outcomes among patients with acute coronary syndrome. Circulation 131:980–987. doi:10.1161/CIRCULATIONAHA.114.013451
Dawes AJ, Sacks GD, Cryer HG et al (2015) Compliance with evidence-based guidelines and interhospital variation in mortality for patients with severe traumatic brain injury. JAMA Surg 150:965–972. doi:10.1001/jamasurg.2015.1678
Bristow RE, Chang J, Ziogas A et al (2015) Impact of national cancer institute comprehensive cancer centers on ovarian cancer treatment and survival. J Am Coll Surg 220:940–950. doi:10.1016/j.jamcollsurg.2015.01.056
Schroeck FR, Kaufman SR, Jacobs BL et al (2014) Adherence to performance measures and outcomes among men treated for prostate cancer. J Urol 192:743–748. doi:10.1016/j.juro.2014.03.091
Boland GM, Chang GJ, Haynes AB et al (2013) Association between adherence to national comprehensive cancer network treatment guidelines and improved survival in patients with colon cancer: guideline treatment improves survival. Cancer 119:1593–1601. doi:10.1002/cncr.27935
van de Water W, Bastiaannet E, Dekkers OM et al (2012) Adherence to treatment guidelines and survival in patients with early-stage breast cancer by age at diagnosis. Br J Surg 99:813–820. doi:10.1002/bjs.8743
Feinstein AR (1985) Clinical epidemiology: the architecture of clinical research. Saunders, Philadelphia
Cheng SH, Wang CJ, Lin J-L et al (2009) Adherence to quality indicators and survival in patients with breast cancer. Med Care 47:217–225. doi:10.1097/MLR.0b013e3181893c4a
Hernan MA (2006) Estimating causal effects from epidemiological data. J Epidemiol Community Health 60:578–586. doi:10.1136/jech.2004.029496
Williamson EJ, Aitken Z, Lawrie J et al (2014) Introduction to causal diagrams for confounder selection. Respirology 19:303–311. doi:10.1111/resp.12238
Zagouri F, Liakou P, Bartsch R et al (2015) Discrepancies between ESMO and NCCN breast cancer guidelines: an appraisal. The Breast 24:513–523. doi:10.1016/j.breast.2015.02.031
National Collaborating Centre for Cancer (2009) Early and locally advanced breast cancer diagnosis and treatment: full guideline. National Collaborating Centre for Cancer, Cardiff https://www.nice.org.uk/guidance/cg80/resources/early-and-locally-advanced-breast-cancer-diagnosis-and-treatment-975682170565. Accessed 12 Dec 2016
Senkus E, Kyriakides S, Ohno S et al (2015) Primary breast cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 26:v8–v30. doi:10.1093/annonc/mdv298
Bleicher RJ, Ruth K, Sigurdson ER et al (2016) Time to Surgery and Breast Cancer Survival in the United States. JAMA Oncol 2:330–339. doi:10.1001/jamaoncol.2015.4508
Meiers P, Cil T, Guller U, Zuber M (2013) Sentinel lymph node biopsy in early-stage breast cancer patients: improved survival through better staging? Langenbecks Arch Surg Dtsch Ges Für Chir 398:687–690. doi:10.1007/s00423-012-1037-2
Coates AS, Winer EP, Goldhirsch A et al (2015) Tailoring therapies—improving the management of early breast cancer: St Gallen International Expert Consensus on the Primary Therapy of Early Breast Cancer 2015. Ann Oncol 26:1533–1546. doi:10.1093/annonc/mdv221
Biglia N, Ponzone R, Bounous VE et al (2014) Role of re-excision for positive and close resection margins in patients treated with breast-conserving surgery. Breast Edinb Scotl 23:870–875. doi:10.1016/j.breast.2014.09.009
A’Hern RP, Ebbs SR, Baum MB (1988) Does chemotherapy improve survival in advanced breast cancer? A statistical overview. Br J Cancer 57:615–618
Bergh J, Jönsson PE, Glimelius B et al (2001) A systematic overview of chemotherapy effects in breast cancer. Acta Oncol Stockh Swed 40:253–281. doi:10.1080/02841860120784
Early Breast Cancer Trialists’ Collaborative Group (EBCTCG) (2011) Relevance of breast cancer hormone receptors and other factors to the efficacy of adjuvant tamoxifen: patient-level meta-analysis of randomised trials. The Lancet 378:771–784. doi:10.1016/S0140-6736(11)60993-8
Clarke M, Collins R, Darby S et al (2005) Effects of radiotherapy and of differences in the extent of surgery for early breast cancer on local recurrence and 15-year survival: an overview of the randomised trials. Lancet 366:2087–2106. doi:10.1016/S0140-6736(05)67887-7
McGuire SE, Gonzalez-Angulo AM, Huang EH et al (2007) Postmastectomy radiation improves the outcome of patients with locally advanced breast cancer who achieve a pathologic complete response to neoadjuvant chemotherapy. Int J Radiat Oncol Biol Phys 68:1004–1009. doi:10.1016/j.ijrobp.2007.01.023
Grunfeld E, Noorani H, McGahan L et al (2002) Surveillance mammography after treatment of primary breast cancer: a systematic review. Breast Edinb Scotl 11:228–235. doi:10.1054/brst.2001.0404
Montgomery DA, Krupa K, Cooke TG (2007) Follow-up in breast cancer: does routine clinical examination improve outcome? A systematic review of the literature. Br J Cancer 97:1632–1641. doi:10.1038/sj.bjc.6604065
Greenland S, Pearl J, Robins JM (1999) Causal diagrams for epidemiologic research. Epidemiol Camb Mass 10:37–48
Textor J, Hardt J, Knüppel S (2011) DAGitty: a graphical tool for analyzing causal diagrams. Epidemiol Camb Mass 22:745. doi:10.1097/EDE.0b013e318225c2be
Andreano A, Anghinoni E, Autelitano M et al (2016) Indicators based on registers and administrative data for breast cancer: routine evaluation of oncologic care pathway can be implemented. J Eval Clin Pract 22:62–70. doi:10.1111/jep.12436
Quan H, Li B, Couris CM et al (2011) Updating and validating the Charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. Am J Epidemiol 173:676–682. doi:10.1093/aje/kwq433
Deyo RA, Cherkin DC, Ciol MA (1992) Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol 45:613–619. doi:10.1016/0895-4356(92)90133-8
Caranci N, Biggeri A, Grisotto L et al (2010) L’indice di deprivazione italiano a livello di sezione di censimento: definizione, descrizione e associazione con la mortalità. Epidemiol Prev 34:167
Nuova Anagrafe Regionale. http://basidati.agid.gov.it/catalogo/bd?code=154911. Accessed 12 Dec 2016
Hernán M, Robins JM (2017) Causal survival analysis. In: Causal Inference. Chapman & Hall/CRC, Boca Raton, partII, pp 75–77
van Buuren S (2007) Multiple imputation of discrete and continuous data by fully conditional specification. Stat Method Med Res 16:219–242. doi:10.1177/0962280206074463
Rubin DB (2004) Multiple imputation for nonresponse in surveys. John Wiley & Sons, Hoboken
SAS Institute Inc. (2013) SAS/STAT Software, Version 9.4., Cary, NC
Core Team R (2015) R: A Language and Environment for Statistical Computing. R Found Stat Computing, Vienna, Austria
Steuten L, Vrijhoef B, Severens H et al (2006) Are we measuring what matters in health technology assessment of disease management? Systematic literature review. Int J Technol Assess Health Care 22:47–57. doi:10.1017/S0266462306050835
Jacobs R, Goddard M (2007) How do performance indicators add up? An examination of composite indicators in public services. Public Money Manag 27:103–110. doi:10.1111/j.1467-9302.2007.00565.x
Shwartz M, Restuccia JD, Rosen AK (2015) Composite measures of health care provider performance: a description of approaches: composite measures of health care provider performance. Milbank Q 93:788–825. doi:10.1111/1468-0009.12165
Reeves D, Campbell SM, Adams J et al (2007) Combining multiple indicators of clinical quality. Med Care 45:489–496. doi:10.1097/MLR.0b013e31803bb479
Huisman M, Kunst A, Andersen O et al (2004) Socioeconomic inequalities in mortality among elderly people in 11 European populations. J Epidemiol Community Health 58:468–475. doi:10.1136/jech.2003.010496
Funding
Supported by grant RF-2011-02348959 from the Italian Ministry of Health.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standards
All analyses were performed in compliance with the Italian law on health data protection.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Appendices
Appendix 1: Sensitivity analyses
1. Results of the IPW marginal structural model, assuming proportional hazards, investigating the association between survival and adherence as a dichotomous variable, using different cut-offs to define adherent care. Results, here and in the following section, are presented as the Hazard ratio (HR) of death for adherent vs. nonadherent patients and their 95% confidence intervals (CI).
Cut-off | % of adherent pts | HR (95% CI) | P |
|---|---|---|---|
60% | 84 | 0.71 (0.58–0.87) | 0.001 |
70% | 77 | 0.63 (0.52–0.76) | <.001 |
80% (main analysis) | 69 | 0.66 (0.55–0.77) | <.001 |
90% | 38 | 0.88 (0.73–1.07) | 0.21 |
2. Results of the IPW marginal structural model, assuming proportional hazards, investigating the association between survival and adherence as a four class ordinal variable (cut-points: 20th percentile, corresponding to 67%; 30th percentile, 75%; 60th percentile, 86%), and as a continuous variable. For the ordinal variable, probability of adherence given potential confounders f(A|L), was estimated using a cumulative logistic regression model with the same covariates of the main analysis, with the exception of all first-degree interactions.
Adherence | HR (95% CI) | P |
|---|---|---|
≤67% vs. > 86% | 2.83 (2.29–3.45) | <.001 |
>67 and ≤ 75% vs. > 86% | 1.57 (1.14–2.14) | 0.005 |
>75 and ≤ 86% vs. > 86% | 1.01 (0.80–1.28) | 0.911 |
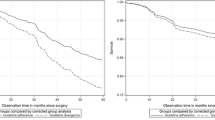
For adherence treated as a continuous variable varying between 0 and 100, f(A|L) is a probability density function and it was estimated through a linear regression model, including the same covariates of the main analysis, and then assuming a normal distribution with constant variance. We estimated an IPW marginal structural model for the association between survival and adherence as a flexible function (restricted cubic spline with three knots at 50, 85 and 90%). The graph illustrates the 8-year probability of death for increasing adherence level, which is higher for low adherence percentage and decreases almost linearly up to 80%. This trend motivated the choice of the cut-off for the main analysis presented in the article.
3. Complete cases analysis: we estimated an IPW marginal structural model for the association between survival and adherence assuming proportional hazards using only patients with all necessary potential confounders in the original dataset (3238). Characteristics of this population are described in the table below. The proportion of adherent patients was 69%. The estimated HR was 0.71 (95%CI, 0.57-0.90, P = 0.004).
No. of pts 3238 | ||||
|---|---|---|---|---|
Adherent No. 2237 | Nonadherent No. 1001 | |||
N | % | N | % | |
Age | ||||
<50 years | 654 | 29.24 | 298 | 29.77 |
50–69 years | 1037 | 46.36 | 362 | 36.16 |
>69 years | 546 | 24.41 | 341 | 34.07 |
Grading | ||||
1 | 241 | 10.77 | 99 | 9.89 |
2 | 1189 | 53.15 | 523 | 52.25 |
3 | 807 | 36.08 | 379 | 37.86 |
Stage | ||||
1 | 1143 | 51.10 | 439 | 43.86 |
2 | 780 | 34.87 | 402 | 40.16 |
3 | 314 | 14.04 | 160 | 15.98 |
Molecular subtype | ||||
Luminal A | 817 | 36.52 | 375 | 37.46 |
Luminal B | 897 | 40.10 | 377 | 37.66 |
Luminal Her2 | 240 | 10.73 | 117 | 11.69 |
Her2 type | 96 | 4.29 | 56 | 5.59 |
Triple negative | 187 | 8.36 | 76 | 7.59 |
N of positive nodes | ||||
0 | 1431 | 63.97 | 618 | 61.74 |
1–3 | 524 | 23.42 | 260 | 25.97 |
4–9 | 161 | 7.20 | 66 | 6.59 |
≥10 | 121 | 5.41 | 57 | 5.69 |
Charlson index | ||||
0 | 1733 | 77.47 | 755 | 75.42 |
1–2 | 471 | 21.05 | 206 | 20.58 |
≥3 | 33 | 1.48 | 40 | 4.00 |
Deprivation index, quintiles | ||||
I | 273 | 12.20 | 146 | 14.59 |
II | 265 | 11.85 | 128 | 12.79 |
III | 336 | 15.02 | 135 | 13.49 |
IV | 525 | 23.47 | 208 | 20.78 |
V | 838 | 37.46 | 384 | 38.36 |
Marital status | ||||
Never married | 238 | 10.64 | 113 | 11.29 |
Married | 1627 | 72.73 | 635 | 63.44 |
Divorced | 88 | 3.93 | 47 | 4.70 |
Widow | 284 | 12.70 | 206 | 20.58 |
Education | ||||
None or elementary school | 713 | 31.87 | 370 | 36.96 |
Middle School | 606 | 27.09 | 230 | 22.98 |
High School | 814 | 36.39 | 339 | 33.87 |
College and higher | 104 | 4.65 | 62 | 6.19 |
Employment | ||||
Housewife/unemployed | 553 | 24.72 | 211 | 21.08 |
Workers | 242 | 10.82 | 90 | 8.99 |
Office worker/teachers | 540 | 24.14 | 232 | 23.18 |
Managers and professionals | 86 | 3.84 | 48 | 4.80 |
Retired | 816 | 36.48 | 420 | 41.96 |
4. Results of the IPW marginal structural model, assuming proportional and non-proportional hazards, investigating the association between survival and adherence as a dichotomous variable, excluding patients > 69 years.
No. | % of adherents | Proportional hazard model | Non proportional hazard model | ||
|---|---|---|---|---|---|
HR (95% CI) | HR(time since diagnosis) (95% CI) | ||||
1 year | 2 years | 5 years | |||
4559 | 72 | 0.73 (0.56–0.95) | 0.55 (0.36–0.86) | 0.58 (0.43–0.80) | 1.04 (0.70–1.56) |
Appendix 2. Distribution of weights
Distribution of stabilized weights derived from the analysis of 50 imputed datasets (missing data imputed by fully conditional specification using MI SAS procedure). Standard errors (SE) have been pooled according to Rubin [39]. Minimum and maximum are the lowest and highest values found across all datasets.
Stabilized weights | Mean | SE | Median | I Q | III Q | Min | Max |
|---|---|---|---|---|---|---|---|
Inverse probability of: | |||||||
Adherence | 1.005 | 0.001 | 0.958 | 0.888 | 1.079 | 0.328 | 7.177 |
Censoring | 1.000 | 0.000 | 1.000 | 0.999 | 1.000 | 0.949 | 1.123 |
Adherence and censoring | 1.005 | 0.001 | 0.958 | 0.888 | 1.079 | 0.328 | 7.184 |
Rights and permissions
About this article
Cite this article
Andreano, A., Rebora, P., Valsecchi, M.G. et al. Adherence to guidelines and breast cancer patients survival: a population-based cohort study analyzed with a causal inference approach. Breast Cancer Res Treat 164, 119–131 (2017). https://doi.org/10.1007/s10549-017-4210-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-017-4210-z