Abstract
Introduction
A small proportion of patients with acute intermittent porphyria (AIP) suffer from recurrent porphyric attacks, with a severely diminished quality of life. In this retrospective case-control study, the burden of disease is quantified and compared among three AIP patient subgroups: cases with recurrent attacks, cases with one or occasional attacks and asymptomatic carriers.
Methods
Data from patient records and questionnaires were collected in patients between 1960 and 2016 at the Erasmus Medical Center, Rotterdam, the Netherlands. We collected symptoms related to porphyria, porphyria related complications, attack frequency, hospitalisation frequency, hospitalisation days related to acute porphyric attacks, frequency of heme infusions and medical healthcare costs based on hospitalisations and heme therapy.
Results
In total 11 recurrent AIP cases, 24 symptomatic AIP cases and 53 AIP carriers as controls were included. All recurrent patients reported porphyria related symptoms, such as pain, neurological and/or psychiatric disorders, and nearly all developed complications, such as hypertension and chronic kidney disease. In the recurrent cases group, the median lifelong number of hospitalisation days related to porphyric attacks was 82 days per patient (range 10–374), and they spent a median of 346 days (range 34–945) at a day-care facility for prophylactic heme therapy; total follow-up time was 243 person-years (PYRS). In the symptomatic non-recurrent group the median lifelong number of hospitalisation days related to porphyric attacks was 7 days per patient (range 1–78), total follow-up time was 528 PYRS. The calculated total medical healthcare cost for recurrent cases group was €5.8 million versus €0.3 million for the symptomatic cases group.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acute intermittent porphyria (AIP) is a rare inherited metabolic disorder in which patients suffer from acute porphyric attacks with abdominal pain, often with anxiety, nausea, tachycardia and hypertension. During severe attacks, psychiatric symptoms, hyponatremia, seizures and progressive peripheral neuropathy can occur (Bylesjö et al 2009). Such attacks can progress to paralysis, respiratory failure, and death if patients are not treated. Apart from acute porphyric attacks, patients have a long term increased incidence of hypertension, kidney disease and hepatocellular carcinoma (HCC) (Andersson et al 1996; Andersson et al 2000; Sardh et al 2013).
AIP is caused by mutations in the hydroxymethylbilane synthase (HMBS, OMIM 609806) gene. In literature it has been described that less than 10% of HMBS gene mutation carriers experience acute porphyric attacks during their lives (Puy et al 2010). However, a recent study indicates an even lower clinical penetrance of about 1% (Chen et al 2016). Ever since heme became the treatment of choice in the 1980s, porphyria attacks have been treated with intravenous heme. This has been shown to be effective in improving both the biochemical abnormalities, clinical symptoms and preventing deterioration of the neurological defects. It is therefore regarded as a life-saving therapy (Whatley and Badminton 2013).
Only a small subset of the symptomatic patient group suffers from recurring porphyric attacks several times per year. Recurring attacks are treated with weekly prophylactic heme infusions (Marsden et al 2015). This therapy is, however, complicated by iron overload, phlebitis, venous thrombosis and frequent need for venous access devices, and is a significant burden for the patient (Willandt et al 2016). Patients who suffer from recurrent attacks report a low quality of life (QoL) and a negative impact on several aspects of everyday life, including unemployment, personal relationships and long-term disability (Millward et al 2001; Jiménez-Monreal et al 2015; Naik et al 2016).
New in this study is the analysis of the recurrent patients separate from sporadically symptomatic cases, and HMBS gene carriers as controls. Although recurring porphyric attacks have been shown to be associated with a poor quality of life, the financial and personal burden of this disease in relation to the occurrence and frequency of attacks are unclear. Therefore, in order to get a better insight into the burden of AIP, we studied the prevalence of porphyria symptoms and complications, in addition to the costs related to recurrent porphyric attacks and compared them to symptomatic porphyria cases and asymptomatic gene carriers in a case-control study design.
Methods
Data collection
In this single-centre retrospective longitudinal observational cohort study, all patients with AIP attending the clinic of the Porphyria Center in the Erasmus Medical Center (Rotterdam, the Netherlands) between 1960 and 2016 were included. The diagnosis AIP was based on either a known HMBS gene mutation, or on positive biochemistry (defined as a delta-aminolaevulinic acid (ALA) and porphobilinogen (PBG) level at least four times the upper limit of normal) in combination with a decreased porphobilinogen deaminase (PBGd) enzyme activity measured in either erythrocytes or lymphocytes.
Data were collected by R.A.N. and J.G.L. from patients’ electronic and paper records, and from self-reported questionnaires (Suppl. file 1). The patient charts and file data were first reviewed. When the retrospective data was unclear (e.g. due to old, poorly hand-written notes), a consensus was formed which was entered in the final database, or the data was discarded.
AIP patients with a proven diagnosis were eligible for inclusion. A confirmed acute porphyric attack was defined as an episode of abdominal pain in parallel with a significant rise in urinary ALA and PBG levels (≥ 4 times upper limit of normal) which necessitated a verified visit or admission to a hospital for diagnosis and treatment. Hospitalisations were defined as hospitalisations with a confirmed acute porphyric attack.
We collected data on (1) porphyria symptoms and long-term complications, (2) employment status, (3) hospitalisation episodes, hospitalisation days, amount and frequency of heme infusions (heme arginate, Normosang®, Orphan Europe), (4) heme dosage schedules, duration of prophylactic heme therapy, complications of heme therapy, placement of a Port-A-Cath® (PAC, Smiths Medical), oral contraception use, therapy with GnRH analogues, analgesia dependence and the age and cause of death. The annualised attack rate was defined as the number of attacks in all observed years of follow up, counting the number of confirmed acute porphyric attacks and dividing by the number of follow up years.
The medical ethics committee of the Erasmus Medical Center, Rotterdam, the Netherlands, approved prospective and retrospective data collection for this study (MEC 2014–593). Patients were asked to sign informed consent during visits to the outpatient clinic. Also, they have approved the use of anonymous retrospective medical data without informed consent.
Patient subgroup definitions
AIP patients were classified in three subgroups based on phenotypic characteristics. The first subgroup comprised cases with recurrent attacks, defined as patients who have more than four attacks in any year, or are on prophylactic heme therapy. The second subgroup was comprised of symptomatic cases, defined as patients who have experienced at least one confirmed acute porphyric attack, but who did not meet the definition of recurrent attack cases. The third subgroup comprised asymptomatic controls, defined as persons who carry a HMBS gene mutation but have never experienced a proven acute porphyric attack.
Cost of care analysis
To calculate the costs of care, we examined paper or electronic hospital records to count the number of verifiable heme infusions and hospitalisations (for day care and regular admission) for each individual. The approach was to be as conservative as possible, all data needed to be verifiable in the charts. Total basic-costs were calculated per individual including only hospitalisations, use of day-care facilities and heme arginate ampoules; the costs are presented per group. Prices are calculated based on 2016 data, historical prices or inflation were not taken into account. These basic costs of care are therefore limited to costs of hospital care and medication and do not take other indirect costs to the patient or society into account.
Statistical analysis
Statistical analyses were performed with IBM SPSS Statistics for Windows (version 21.0. Armonk, NY: IBM Corp.). Parameters were tested for normality using the Shapiro-Wilk test for normality. Normally distributed numerical data were compared among groups with one-way ANOVA, Bonferroni corrected. Non-parametric numerical independent data were analysed with Kruskal-Wallis’ test. Categorical data were analysed using the linear-by-linear Chi-square association-test, or Fischer’s exact test.
Supplementary methods description
Assays for porphyrins, porphyrin precursors and enzyme activity measurements were analysed as previously described (de Rooij et al 2003), see Suppl. file 2.
Results
Cohort description
The study cohort consisted of 88 individuals with AIP from 49 families, baseline characteristics are presented in Table 1. In 77 patients the diagnosis of AIP was confirmed by identifying a HMBS mutation. Twenty-five different HMBS gene mutations were identified (Suppl. file 3), the R116W (c.346C>T) mutation was the most common mutation (21 subjects, 24%). In the remaining 11 individuals the diagnosis AIP was based on biochemical test results in combination with decreased HMBS enzyme activity.
Eleven patients (13%) were categorised as recurrent cases (subgroup R), 24 (27%) patients were categorised as symptomatic cases (subgroup S) and 53 persons (60%) were categorised as asymptomatic AIP carriers (subgroup A, control group). The male-to-female ratio, BMI and age at diagnosis were similar in all three groups. The age of onset of symptoms was not different between both symptomatic groups. Laboratory results are presented in Fig. 1 and details are presented in Suppl. file 4.
The distribution of first measured urinary porphyrin precursors in the different AIP groups. Subgroups were based on phenotypic characteristics: recurrent cases were defined as having more than four attacks in any year, or on prophylactic heme therapy; symptomatic cases, were defined as having experienced one or more confirmed acute porphyric attack; asymptomatic controls never experienced a proven acute porphyric attack. Abbreviations: A, asymptomatic controls; ALA, delta-aminolevulinic acid; PBG; porphobilinogen; R, recurrent cases; S, symptomatic cases. The grey areas mark increased levels, starting at 4 times the upper limit of normal (ULN) 4xULN ALA ≥ 184 μmol/L 4x ULN PBG ≥ 36 μmol/L
Prevalence of porphyric symptoms
Life-long prevalence of acute porphyria-related symptoms, long-term complications and other parameters such as unemployment in all three groups are presented in Table 2. Patients in the recurrent cases group report more porphyria related symptoms: pain, neurological deficits, and psychiatric symptoms. These differences were statistically significantly (p-values <0.001), except for the psychiatric symptoms. The differences between reported symptoms from patients in both symptomatic groups are smaller and mostly not statistically significantly different. However, the prevalence of several symptoms is at least double in the recurrent cases group compared to the symptomatic group, Suppl. file 5; malaise (p = 0.01, 82% of patients in recurrent group versus 29% in symptomatic group), fatigue (p < 0.01, 91 vs 38%), nausea (p < 0.01, 100 vs 46%), anxiety (p < 0.01, 46 vs 21%), psychosis/hallucinations (p = 0.03, 36 vs 4%) and seizures (p < 0.05, 46 vs 13%).
Prevalence of long-term complications
Hypertension was more prevalent in the recurrent cases group (73%) and in the symptomatic cases (71%) compared to the asymptomatic control group (26%). Kidney disease was also more prevalent in the recurrent cases (64%) and symptomatic cases (46%) compared to asymptomatic controls (13%), Table 2 and details in Suppl. file 5. There were four cases with hepatocellular carcinoma (HCC); one from the recurrent cases, two from the symptomatic cases, and one from the asymptomatic controls. One of the HCC patients was still alive at the time of database lock. In three patients, the tumour was inoperable and/or there were metastases at presentation. The fourth patient unfortunately died due to surgical complication, although the tumour was detected as an incidental finding in a curative stage.
Anemia was present in 14 cases, and mostly prevalent in the recurrent cases (7/11, 64%) and symptomatic cases (4/24, 17%) compared to asymptomatic controls (3/53, 6%). Kidney disease was present in 79% of the anemia cases (11/14). Anemia without renal insufficiency was present in 21% of all anaemic persons (3/14).
Number of hospitalisations, day-care-admissions, heme therapy and attack frequency
The life-long hospital admissions, duration and the calculated costs are presented in Table 3. Individuals from the recurrent group were hospitalised for a median of 82 days and received a median of 399 total ampoules of heme per person. Heme schedules differed among patients and over time, ranging from every other week, to weekly and biweekly. Individuals from the symptomatic group were hospitalised for a median of 7 days for acute attacks and received a median of 3 ampoules of heme per person. The median total cost per person of combined heme/albumin infusions for the recurrent subgroup was € 292.000 versus €2.200 for the symptomatic subgroup. The costs for the recurrent patient group accounted for at least 95% of the total costs.
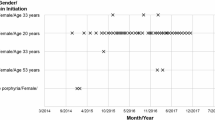
We calculated the number of attacks for the symptomatic and recurrent groups, per year of total follow-up. In total, in the recurrent group there were 137 acute attacks in 407 years of follow-up, or 0.3366 attacks per year. In the symptomatic group, there were 56 acute attacks in 959 years of follow-up, or 0.0584 attacks per year. The patients in the recurrent group suffered 5.8 times more attacks during follow-up. Figure 2 illustrates the follow-up time, the attacks and heme therapy for each patient in the symptomatic and recurrent groups over the observation period.
Schematic information with individual life lines with porphyric attacks of all symptomatic cases, including information regarding prophylactic heme therapy. Subgroups were based on phenotypic characteristics: recurrent cases were defined as having more than four attacks in any year, or on prophylactic heme therapy; symptomatic cases, were defined as having experienced one or more confirmed acute porphyric attack; asymptomatic controls never experienced a proven acute porphyric attack. On the left there are 11 lines derived from patients with recurrent attacks, and on the right 24 lines derived from symptomatic cases. Each line starts at 15 years of age and ends at the end of the observation period or death. Each segment on the line represents one year. The red blocks represent one attack during that year. The green bars under the timelines represent years in which patients received prophylactic heme. A cross represents death. Abbreviations. LTF, lost to follow-up; HCC, hepatocellular carcinoma; LTx, liver transplant. *not included in study analysis
Comparing the number of attacks before the start of heme prophylaxis to the number of attacks during heme prophylaxis, a 50% reduction in number of attacks was observed; before heme prophylaxis there were 2.28 attacks per year, during heme prophylaxis 1.11 attacks per year.
Description of cases with premature death
At the end of the observation period (31 December 2016) the median age of the AIP cohort was 54 years (range 18–81). Five patients died during the observation period, median age of death was 65 years (range 34–72 years). All deaths were directly or indirectly related to porphyria. Four out of five patients were in the recurrent attack group. One person died in the symptomatic case group, this was a male patient presenting at age 41 years with a first uncomplicated porphyric attack. At age 72 years, HCC was diagnosed following an incidental finding on a PET CT-scan performed for headache. He underwent hemi-hepatectomy but died from a brainstem hemorrhage, 13 days post-operatively. A detailed description of all deceased cases is presented in Suppl. file 6.
Recurrent cases subgroup
The details of the recurrent cases subgroup are presented in Table 4. Four out of 11 patients (36%) were male. The median number of attacks requiring hospitalisation was eight per patient (range 2–54) following a median observation time of 21 years (range 3–38). The total number of hospitalisation days per patient ranged between 10 to 374 days. Analgesic dependency was a problem in nearly all recurrent patients (82%, 9/11). Prophylactic heme therapy was initiated in a patient following only two attacks, this was deemed necessary following progression of neurological symptoms and a progressive rise in ALA and PBG levels following the first two attacks.
Prophylactic heme schedules were every other week, weekly, or biweekly, with a duration ranging from 1 to 14 years. PAC venous access catheters were required in 73% (8/11) of the cases to secure venous access. However, venous access was never an absolute limitation for heme therapy. The total number of heme infusions ranged from 79 to 945 per patient, while total lifelong medication costs ranged from €51.500 to €616.046 per patient. Reported side effects of heme therapy were increased serum ferritin levels and possibly iron overload (9/11, 82%) and phlebitis (4/11, 36%); iron overload was treated by phlebotomies.
Eleven patients on prophylactic heme therapy have made attempts to be weaned off heme therapy. This has triggered acute porphyric attacks in nine patients. One patient was weaned off heme by slowly reducing the amount of heme over a period of a year, this was followed by a liver transplantation (Willandt et al 2016), the only liver transplantation in this cohort.
Two patients were treated with hormonal interventions. One was treated with a GnRH-analogue (Syranel®, Pfizer Inc.) for a limited number of months, since she developed burdensome postmenopausal symptoms and no effect on reducing attacks. A second patient endured four porphyric attacks within 6 months, but following placement of a hormonal IUD, she has been free from attacks for 2 years now (52 mg levonorgestrel-releasing intrauterine device (IUD), Mirena®, Bayer HealthCare).
Discussion
This study is based on a longitudinal patient cohort and aims to quantify the severity of disease in AIP patients with recurrent attacks and compares this group to patients with sporadic symptoms and asymptomatic carriers. Patients with recurrent AIP have a high mortality rate and severe morbidity. Severe physical and psychological symptoms, including temporary or permanent disability, lead to unemployment in two-thirds of the recurrent patients. Hypertension and kidney disease were observed in respectively 73 and 64% of patients with recurrent AIP disease. Frequent hospitalisations for acute porphyric attacks, and frequent hospital visits when on prophylactic heme therapy alone, have a major impact on their lives and contribute most to the total calculated medical costs.
Studies that focus specifically on the recurrent patient group are scarce and mainly focus on the group’s diminished quality of life and therapeutic interventions in patient series (Marsden et al 2015; Schulenburg-Brand et al 2017). A recent qualitative study focused on the recurrent patient group (Naik et al 2016). They investigated the patients’ disease experience and concluded recurring patients have a markedly impaired QoL and often turn to alternative medicine. Another study interviewed five recurrent attack patients and showed that all of them reported psychological and coping issues with regard to the dysfunction the recurrent attack state causes (Wikberg et al 2000). The preliminary results of the prospective ‘EXPLORE’ study (Congress abstracts: https://icpp2017.org/wp-content/uploads/2017/06/OCs.pdf) show a high burden of disease in patients with frequent attacks. Our findings are in line with these findings, and illustrate one of the effects of the poor QoL in the high level of unemployment in the recurrent group. The present study shows there is a large difference in hospitalisation frequency and subsequent medical costs between recurrent and sporadic symptomatic patients. The increased burden, together with the costs, underline the importance to differentiate among recurrent cases, symptomatic cases and asymptomatic HMBS gene carriers. Asymptomatic HMBS gene carriers are without obvious disease burden or related medical costs, and will require separate studies to detect any long-term effects of the mutation.
Major strengths of this study are the prospectively defined clear study endpoints and categorisation of patients based on strict criteria for acute porphyric attacks to make comparisons among the different AIP patient groups possible. However, by using these strict criteria, an underestimation of the true impact on patient’s life and costs is likely, which may be regarded as a limitation. Furthermore, a retrospective study design, with data collection in historical, hand-written, medical charts and hospital records, will have resulted in missing data, and again in an underestimation of the burden and healthcare costs. Since 2014, we have collected data prospectively with questionnaires which can lead to recollection bias in all patient groups. There is also a definite underrepresentation of asymptomatic HMBS carriers in this cohort; based on the number of AIP families. Females were overrepresented in the present cohort (68%). This overrepresentation was expected in the symptomatic groups, since females have an increased risk of attacks (Bonkovsky et al 2014). However, this cannot explain the overrepresentation in the asymptomatic group which might be caused by selection bias, since women often have other reasons for abdominal pain.
There is a high prevalence of long term complications, such as hypertension, chronic kidney disease and hepatocellular carcinoma in AIP. In the present study, an increased prevalence of hypertension and chronic kidney disease in the recurrent patient group was present, compared to the other groups. Factors contributing to the occurrence of complications have not yet been elucidated. Long-term exposure to elevated plasma levels of ALA and PBG has been postulated to play a role. However, we’ve found a marked overlap in ALA and PBG levels among the recurrent, the symptomatic cases and asymptomatic HMBS gene carriers. There is no good explanation why some patients with markedly increased levels are without symptoms or long-term complications. Such subjects are often referred to as “asymptomatic high excreters”. In this group, plasma ALA PBG are often as high or even higher than those found in symptomatic patients (data not shown). For future studies this could be an interesting group to examine. Other mechanisms may play a role in AIP-associated tissue damage, such as human peptide transporter 2 (hPEPT2) genotypes, that are associated with AIP-associated kidney damage (Tchernitchko et al 2016). Hypertension was not associated with renal function decline in AIP patients (Pallet et al 2015).
Figure 2 illustrates the effect of prophylactic heme therapy on attack rates in the individual patients. This therapy is not only expensive, but also time-consuming for the patients, and not fully successful in most patients. However, interrupting their schedules triggered severe acute porphyric attacks in nearly all patients. These rebound attacks are probably in part due to prolonged induction of hepatic heme oxygenase by administration of exogenous heme, resulting in increased heme turnover (Doberer et al 2010; Thomas et al 2016). Interestingly, it has been recently shown that the prevalence of patients with recurring attacks has increased since the introduction of heme arginate therapy (Schmitt et al 2018). An explaination could be that the prevalence of patients with recurring attacks has increased since the introduction of heme arginate therapy. There are promising emerging therapies for AIP such as gene-therapy, short interfering RNA (Chan et al 2015; Fontanellas et al 2016), which are undergoing clinical trials; until these therapies become available, heme will remain the most effective therapy. Consensus definitions of acute porphyric attacks and acute porphyric symptoms should be developed, in order to define indications for initiation and schedules, in patient with frequent and/or disabling porphyric attacks.
Conclusion and recommendations
In conclusion, AIP patients with recurrent attacks have a high mortality and morbidity, compared to other symptomatic AIP patients and to asymptomatic carriers. Recurrent attacks result in high medical costs and high unemployment rates. In future studies, these different AIP groups should therefore be analysed separately, as our study clearly demonstrated that patients with recurrent attacks are different than sporadical symptomatic patients and asymptomatic HMBS gene carriers.
Change history
27 July 2018
Due to a typesetting error the wrong figure 2 was used.
References
Andersson C, Bjersing L, Lithner F (1996) The epidemiology of hepatocellular carcinoma in patients with acute intermittent porphyria. J Intern Med 240(4):195–201
Andersson C, Wikberg A, Stegmayr B, Lithner F (2000) Renal symptomatology in patients with acute intermittent porphyria. J Intern Med 248(4):319–325
Bonkovsky HL, Maddukuri VC, Tazici C et al (2014) Acute porphyrias in the USA: features of 108 subjects from the porphyrias consortium. Am J Med 127(12):1233–1241
Bylesjö I, Wikberg A, Andersson C (2009) Clinical aspects of acute intermittent porphyria in northern Sweden: a population-based study. Scand J Clin Lab Invest 69(5):612–618
Chan A, Liebow A, Yasuda M et al (2015) Preclinical development of a subcutaneous ALAS1 RNAi therapeutic for treatment of hepatic porphyrias using circulating RNA quantification. Mol Ther Nucleic Acids 4:e623
Chen B, Solis-Villa C, Hakenberg J et al (2016) Acute intermittent Porphyria: predicted pathogenicity of HMBS variants indicates extremely low penetrance of the autosomal dominant disease. Hum Mutat 37(11):1215–1222
de Rooij FWM, Edixhoven A, Wilson JHP (2003) Porphyria: a diagnostic approach. In: Kadish KM, Smith KM, Guilard R (eds) The porphyrin handbook. Elsevier, New York, pp 212–245
Doberer D, Haschemi A, Andreas M et al (2010) Haem arginate infusion stimulates haem oxygenese-1 expression in healthy subjects. Br J Pharmacol 161(8):1751–1762
Fontanellas A, Ávilla MA, Berraondo P (2016) Emerging therapies for acute intermittent porphyria. Expert Rev Mol Med 18:e17
Jiménez-Monreal AM, Murcia MA, Gómez-Murcia V, Bibiloni Mdel M, Pons A, Tur JA, Martínez-Tome M (2015) Anthropometric and quality-of-life parameters in acute intermittent Porphyria patients. Medicine (Baltimore) 94(30):e1023
Marsden JT, Guppy S, Stein P et al (2015) Audit of the use of regular Haem Arginate infusions in patients with acute Porphyria to prevent recurrent symptoms. JIMD Rep 22:57–65
Millward LM, Kelly P, Deacon A, Senior V, Peters TJ (2001) Self-rated psychosocial consequences and quality of life in the acute porphyrias. J Inherit Metab Dis 24(7):733–747
Naik H, Stoecker M, Sanderson SC, Balwani M, Desnick RJ (2016) Experiences and concern of patients with recurrent attacks of acute hepatic porphyria: a qualitative study. Mol Genet Metab 119(3):278–283
Pallet N, Mami I, Schmitt C et al (2015) High prevalence of and potential mechanisms for chronic kidney disease in patients with acute intermittent porphyria. Kidney Int 88(2):386–395
Puy H, Gouya L, Deybach J (2010) Porphyrias. Lancet 375(9718):924–937
Sardh E, Wahlin S, Björnstedt M, Harper P, Andersson DE (2013) High risk of primary liver cancer in a cohort of 179 patients with acute hepatic Porphyria. J Inherit Metab Dis 36(6):1063–1071
Schmitt C, Lenglet H, Yu A et al (2018) Recurrent attacks of acute hepatic porphyria: major role of the chronic inflammatory response in the liver. J Intern Med. https://doi.org/10.1111/joim.12750
Schulenburg-Brand D, Gardiner T, Guppy S, et al (2017) An audit of the use of gonadorelin analogues to prevent recurrent acute symptoms in patients with acute porphyria in the United Kingdom. JIMD Rep 36:99–107
Tchernitchko D, Tavernier Q, Lamoril J et al (2016) A variant of peptide transporter 2 predicts the severity of Porphyria-associated kidney disease. J Am Soc Nephrol 28(6):1924–1932
Thomas RA, Czopek A, Bellamy CO, McNally SJ, Kluth DC, Marson JP (2016) Hemin preconditioning upregulates heme oxygenase-1 in deceased donor renal transplant recipients: a randomized, controlled, phase IIB trial. Transplantation 100(1):176–183
Whatley SD, Badminton MN (2013) Acute intermittent porphyria. 2005 Sep 27 [Updated 2013 Feb 7]. In: Adam MP, Ardinger HH, Pagon RA, et al., editors. GeneReviews® [Internet]. Seattle (WA): University of Washington, Seattle; 1993-2018. Available from: https://www.ncbi.nlm.nih.gov/books/NBK1193/
Wikberg A, Jansson L, Lithner F (2000) Women's experience of suffering repeated severe attacks of acute intermittent porphyria. J Adv Nurs 32(6):1348–1355
Willandt B, Langendonk JG, Biermann K et al (2016) Liver fibrosis associated with iron accumulation due to long-term heme-arginate treatment in acute intermittent Porphyria: a case series. JIMD Rep 25:77–81
Acknowledgements
We are grateful to all the patients who participated and to the medical and nursing staff of the Erasmus MC in Rotterdam and the Isala Hospital in Zwolle for providing clinical follow-up data. We would also like to thank Dr. J.M. van Rosmalen, biostatistician, for statistical advice.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All procedures were followed in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Decleration of 1975, as revised in 2013. The medical ethics committee in the Erasmus MC, Rotterdam, the Netherlands, has approved the collection of retrospective/prospective data of patients with acute porphyrias (MEC-2014-593).
Conflict of interest
R. Neeleman, M. Wagenmakers, R. Koole-Lesuis, S. Mijnhout, P. Wilson, E. Friesema, and J. Langendonk declare that they have no conflicts of interest.
Funding
This study was initiated in 2013, and data collection started in 2014. Rochus Neeleman’s position is supported with the aid of a grant from The Foundation for Liver and Gastrointestinal Research (SLO).
Use of laboratory animals
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Communicated by: Robin Lachmann
The original version of this article was revised: the wrong figure 2 was used.
Electronic supplementary material
Supplementary file 1
(DOCX 33 kb)
Supplementary file 2
(DOCX 17 kb)
Supplementary file 3
(DOCX 13 kb)
Supplementary file 4
(DOCX 17.1 kb)
Supplementary file 5
(DOCX 16 kb)
Supplementary file 6
(DOCX 13 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Neeleman, R.A., Wagenmakers, M.A.E.M., Koole-Lesuis, R.H. et al. Medical and financial burden of acute intermittent porphyria. J Inherit Metab Dis 41, 809–817 (2018). https://doi.org/10.1007/s10545-018-0178-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10545-018-0178-z