Abstract
We aimed to validate the HIV Stigma Mechanisms Scale (HIV-SMS) in a sample of Mexican adults living with HIV, which differentiates between sources and mechanisms of stigma. Adults (n = 362) with a median age of 32 years old completed a web-based version in Spanish of the HIV-SMS as well as sociodemographic and HIV-related characteristics questionnaire. Exploratory factor analyses with weighted least squares and oblique rotation were performed to assess the construct validity of the scale. The Spanish translation for the Mexican population of the HIV-SMS has adequate internal consistency (Ω = 0.86) and demonstrated a structure similar to the original scale. After excluding the items related to community and social workers, a five-factor solution with internalized, promulgated, and anticipated stigma from family and healthcare workers showed adequate construct validity. The HIV-SMS is a valid and sensitive scale that can be used in a Mexican adult population living with HIV.
Resumen
El objetivo de este estudio fue validar la Escala de Mecanismos de Estigma de VIH (EME-VIH) en una muestra de adultos mexicanos que viven con VIH. Esta escala distingue entre fuentes y mecanismos de estigma. 362 adultos con una edad media de 32 años completaron vía web una versión en español de la EME-VIH así como preguntas acerca de sus características sociodemográficas y cuestiones relacionadas con el VIH. Se realizaron análisis factoriales exploratorios de mínimos cuadrados ponderados con rotación oblicua para evaluar la validez de constructo de la escala. La traducción al español de la EME-VIH para población mexicana tiene consistencia interna adecuada (Ω = 0.86) y muestra una estructura similar a la escala original. Después de excluir los ítems relacionados con trabajadores comunitarios y sociales, se encontró una solución con validez de constructo adecuada de cinco factores: estigma internalizado, promulgado y anticipado ejercido por la familia y personal de salud. La EME-VIH es una escala válida y sensible que puede usarse en población adulta mexicana que vive con VIH.
Similar content being viewed by others
Introduction
HIV- related stigma is the combination of beliefs, attitudes, and actions against persons living with HIV (PLWH) [1]. It involves a social phenomenon that contributes to a range of psychological responses that makes persons realize that they have a devaluated social characteristic [2]. HIV- related stigma has been explained as other health-related stigmas, in which the perpetration of the rejection of people living with a disease is based on blaming persons for their condition and isolating them to decrease the risk of infection [3]. Stigma continues to be a barrier to HIV prevention and treatment in high-income settings [2], but its effects are even more evident in low- and middle-income countries [4], including Mexico, where new infections have not been controlled [5].
Highly active antiretroviral therapy (HAART) for HIV has been available in Mexico since 1997 and it covers the uninsured population since 2003 [6]. However, HIV-related mortality has not decreased. In 2021, there were 11,869 new cases reported nationwide (incidence rate 9.3 per 100,000 persons), and 5,281 related- deaths were registered in 2019 (mortality rate 4.19 per 100,000), the highest in recent years [5]. Optimal outcomes of antiretroviral therapy (ART) in Mexico are still an unachieved goal, which may be related to the high rates of late entry into HIV care and treatment [7].
As in other countries, in Mexico stigma may play an important role as a barrier to services, treatment adherence, and it may also extend to Pre-Exposure Prophylaxis (PrEP) services [8]. Key informants in the Mexican northern city of Tijuana stated that PLWH face stigma from family members, and healthcare professionals. Consequently, they choose not to disclose their status to their families, friends, coworkers, and employers [9]. Enacted stigma by health providers in Mexico has been related to a lack of treatment adherence and a lower quality of life among PLWH [10]. Stigma is usually unaccounted in the HIV care cascade although its effects are potentially substantial in access to care and treatment adherence [11].
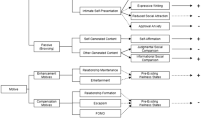
Theoretical frameworks and instruments are key to studying and addressing the association between a construct such as stigma and HIV-related health outcomes. The HIV Stigma Framework [2] explores how HIV stigma acts through three mechanisms (enacted or promulgated, internalized, and anticipated), which may lead to negative health outcomes among PLWH. This research article aims to adapt and validate de HIV mechanisms of stigma scale [12] for the Mexican adult population living with HIV. Unlike other instruments, this scale is based on a robust conceptual framework that was developed after gathering data on HIV-related experiences of stigma that may hinder access to care [2, 12].
Methods
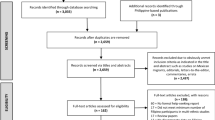
Sampling
Participants were recruited from April to July 2021 through a web-based snowball sampling that was initiated through supporting local nongovernmental organizations (NGOs) that provide services to PLWH, sexually transmitted infections (STI) testing, and sex work advocates, among others. Web-based sampling was performed given the sanitary conditions imposed due to the COVID-19 pandemic. This sampling method has proved to be adequate for hardly- reached populations, who may be disenfranchised and not engaged in treatment, such as PLWH. The NGOs, service providers, and participants shared the survey through their social networks, newsletters, and e-mail accounts. Inclusion criteria comprised being 18 years or older, having been diagnosed with HIV, and currently living in Mexico. All participants provided informed consent and voluntarily agreed to participate in the anonymous survey.
Measures
The original instrument was validated among an adult sample of PLWH in the United States [12]. It is based on the stigma framework [2], which considers 3 stigma mechanisms that are reflected in three types of psychological responses. This instrument consists of 3 subscales for each type of stigma: [1] promulgated (enacted) stigma, assessed through 9 Likert-scale items ranging from 1 (never) to 5 (always); [2] internalized stigma, assessed through 6 Likert-scale items ranging from 1 (strongly disagree) to 5 (strongly agree); and [3] anticipated stigma, assessed through 9 Likert- scale items ranging from 1 (very unlikely) to 5 (very likely). Each subscale has adequate internal consistency (α = 0.87; α = 0.89; α = 0.87 respectively). Promulgated and anticipated stigma are assessed from three sources: family, community and social community workers, and healthcare workers (three items each).
We also included the following sociodemographic characteristics: sexual identity (ciswoman, cisman, trans woman, trans man, other), age, sexual orientation (gay, heterosexual, bisexual, other), educational attainment (elementary, secondary, high school, community college, undergraduate, postgraduate), marital status (single, married/coliving, divorced, widowed, other), employment status (student, full-time employment, part-time employment, looking for a job, other) source of income (none, formal job, informal job, partner/family, public programs, begging, other), and average monthly income asked in Mexican pesos according to minimum wage rates in 2020 (< USD$49.3, USD$49.3- USD$133.6, USD$133.7- USD$267.2, USD$267.3- USD$400.9, USD$400.9- USD$668.2, >USD$668.2) [13].
HIV-related questions included current enrolment in ART (yes/ no), persons with whom participants have shared their HIV status (close social network, family, partner, healthcare workers, no one), to have been diagnosed with AIDS (yes/ no), years with a positive diagnosis for HIV, years enrolled in ART, and years with AIDS diagnosis.
Procedure
Phase 1: Pilot. The original instrument was independently translated by AL and CR. The translation was compared to the Spanish version used in the United States by Earnshaw and colleagues [12], grammar and style modifications were minimal. They involved the use of idioms to make the questions easier to understand in the Mexican context. After consensus, the scale was piloted online using Survio [14], an online survey service that guarantees data protection and encryption. Survio is certified by several international entities that guarantee data security and protection. In addition to the stigma scale, we included other HIV-related questions and sociodemographic characteristics. Open-ended questions were included to assess the quality of the translation, clarity in the instructions, appropriateness of the questions, and answer options. Based on the open-ended answers of the 107 participants that were included in the pilot phase, the answer options of the promulgated stigma subscale were modified to include “they do not know I live with HIV” and “not applicable”.
Phase 2. Validation. Sociodemographic characteristics, HIV-related factors, and the modified version of the scale were also uploaded into Survio. To allow participants to choose whether to answer each item, we included the following options: “they do not know I live with HIV” (coded as zero), and “I prefer not to answer” and “not applicable” (both coded as missing data). For the latter, we performed mean imputation, which has been proposed as an adequate solution to preserve the sample size without exaggerating distortion of results when a few items are omitted [15].
Statistical Analyses
We performed descriptive statistics to determine sample sociodemographic and HIV-related characteristics and performed Mardia’s test to assess multivariate normality among scale items. Due to the lack of normality and data level of assessment, we computed the polychoric correlation matrix. Then, we tested the fit of the correlation matrix using Bartlett’s Test Sphericity and Kaiser- Meyer- Olkin (KMO) Test. The decision about the number of factors to retain was supported by summary results from 23 indicators implemented in R’s nFactors routine [16]. Based on currently recommended standards, we performed an exploratory factor analysis (EFA) using weighted least squares (WLS) estimation with oblimin oblique rotation [17]. We assessed internal consistency for polytomous variables using ordinal omega coefficients for the global scale, by subscale (i.e., types of stigma), and sources of stigma.
Considering that 34.5% (n = 125) participants responded “they do not know I live with HIV” in items related to family promulgated stigma, we performed a Mann-Whitney U test to determine whether there were statistically significant differences between those who have and have not shared their HIV status with their family members. We found significant differences in four items of the internalized stigma sub-scale: Item 3 U(z= -1.99, p = 0.046); Item 4 U(z= -3.54, p < 0.01); Item 5 U(z= -3.36, p < 0.01); Item 6 U(z= -4.07, p < 0.01) and one promulgated stigma, Item 9 U(z = 2.33; p = 0.02). Based on these findings, we performed independent EFAs by HIV status disclosure to assess significant differences in the extracted factors for each model and their respective explained variance. In addition, given cultural and health- care system differences between the United States sample studied in Earnshaw [12] and this Mexican sample —as the United States is one of the countries with the largest program of community health workers in the world, as opposed to Mexico [18]—, we also performed independent EFAs excluding the items related to community and social workers from the promulgated and anticipated stigma subscales.
Hence, we performed six EFAs for different combinations of subsamples / items, among (1) full sample / all items; (2) full sample / all items except for those related to community and social community workers; (3) among those who disclosed their HIV status to their family members / all items; (4) among those who disclosed their HIV status to their family members / all items except for those related to community and social community workers; (5) among those who did not disclose their HIV status to their family members / all items except for those related to promulgated stigma from family members; (6) among those who did not disclose their HIV status to their family members / all items except for those related to promulgated stigma from family members and items related to community and social community workers. The selection of the best EFA was based on factor loadings, explained variance, and root mean square of residuals (RMSR).
All statistical analyses were performed in R Statistical Software. EFAs were fit using the fa routine from the psych package [19].
Ethical Considerations
This study was approved by the Ethics Committee of the Faculty of Psychology at the Universidad Nacional Autónoma de México. All participants provided informed consent before responding to the questionnaire.
Results
Sociodemographic Characteristics
Of the 362 participants, most were cismen (87.3%), followed by ciswomen (10.5%), and a small proportion of trans women (0.8%) (Table 1). The median age was 32 (interquartile range [IQR] = 28–40). Sexual orientation was mostly gay (81.6%), followed by heterosexual (9.2%), bisexual (7%), and other (2.2%). Most of the sample was single (75.5%), and a smaller proportion was married (11.9%), and divorced or widowed (2.6% each). Half of the sample had a full-time job (53.1%), and the rest were part-time employees (7.3%), full-time students (7.3%), a combination of both (9.5%), looking for a job (10.1%) or decided not to disclose their employment status (12.8%). The average monthly income was mostly distributed in the highest categories.
HIV Characteristics
In terms of the HIV-related characteristics (Table 2), participants reported having had a positive diagnosis of HIV for a median of 3 years (IQR = 1.5–7). Most of the sample reported being enrolled in ART at the time of the survey (96.7%). Regarding HIV status sharing, some had not disclosed it with anyone (6.3%), more than half with their close social network (59.1%), family (51.4%), intimate partners (51.9%), and healthcare workers (51.9%). Finally, among those who reported having an AIDS diagnosis (10.4%), the median time since AIDS diagnosis was 2 years (IQR = 1.3–7).
Factor Structure and Reliability
We assessed six EFAs using the WLS method (Supplementary Table 1). After close examination of these models (variance ranging from 56 to 68%; smallest factor loadings ranging from 0.42 to 0.60, and RMSR ranging from 0.03 to 0.05), we selected a 5- factor model that corresponds to the three mechanisms of stigma and two sources of stigma (family and healthcare workers, excluding community and social workers). This model includes 18 of the 24 original items and accounts for 68% of the variance (Supplementary Table 2). The KMO test result was 0.82 (X2153 = 4076.88; p < 0.001; RMRS corrected index = 0.03, factor loadings above 0.6 and communality from 0.45 to 0.91), indicating high adequacy of the model (Table 3). The internal consistency (Ω) is acceptable in all factors, ranging from 0.87 (promulgated stigma from healthcare workers) to 0.95 (promulgated stigma from family members). The global reliability is acceptable (Ω = 0.86).
HIV Stigma Mechanisms
In a scale from zero to five, the sample reported a low total score of stigma (mean = 2.0; standard deviation [SD] = 0.6; median = 1.9; interquartile range [IQR] = 1.6– 2.4) (Table 4). The lowest score was reported for promulgated stigma among family members (median = 1.0), and the highest was for internalized stigma (median = 2.3).
Discussion
This study aimed to validate the HIV mechanisms of stigma scale for the Mexican population. From the six models we tested, we selected the 5-factor model, explaining 68% of the total variance. To our knowledge, there is only a previous study that validated an HIV stigma scale [20]. Overall, our findings show better psychometric properties than the validation for the Mexican sample (n = 75) of the Berger HIV stigma scale [20], which explains 60.5% of the total variance and reported a KMO = 0.78. It is relevant to compare the psychometric properties of both scales to distinguish that the HIV-SMS is a more appropriate instrument for the Mexican population.
In our sample, 10.2% of participants reported having transitioned to an AIDS diagnosis, which is concerning considering that the median age of the sample is 32 and that most have lived with an HIV diagnosis between 0.5 and 7 years. Although the sociodemographic characteristics of the sample are different from those of the general population, this finding is supported by previous reports of late HIV diagnosis in the Mexican population, especially among highly marginalized populations [7]. A study that analyzed predictors of late HIV diagnosis in Mexico found that the national HIV Program that ran from 2013 to 2017 had been marginally successful in decreasing the proportion of persons with a late HIV diagnosis, especially among cismen older than 29 years old [21], who are the group with the highest rate of HIV in the country.
Most of our sample reported currently receiving ART and have been engaged in treatment almost immediately after their diagnosis. This also stresses the need for extended HIV testing, timely diagnosis, and treatment engagement. In Mexico, treatment adherence may be associated with structural barriers such as health insurance affiliation [22]. Future studies need to assess the intersection between treatment adherence and healthcare services, and stigma.
Although stigma scores were overall low, this sample reported a medium score for internalized stigma. Internalized stigma may be related to the fact that a third of the sample had not disclosed to their family their HIV- positive status. In addition, it may also have health implications, including low treatment adherence and sexual risk behaviors [23, 24]. Internalized stigma may contribute to mental health symptoms such as depression, anxiety, and hopelessness [25]. These psychological characteristics may influence the reiterative decisions related to status disclosure and how to cope with stigma [26]. Further studies need to address this in the Mexican population.
This study has several limitations. First, we did not assess discriminant or convergent validity. However, our findings support the evidence of construct validity and future studies should focus on the standardization of the scale. Second, although 78% of the Mexican urban population has Internet access [27], web-based studies have consistently reported a more privileged profile of participants than the Mexican general population [28, 29]. This includes higher income than the national average, higher educational attainment, and potentially higher ART access through employment-based healthcare. However, web-based studies also allow to access hardly reached populations, such as stigmatized persons, and allow them to respond in a more confidential approach than face-to-face surveys [30]. Third, although we aimed to purposively sample more ciswomen, transwomen, and transmen living with HIV through women-only NGOs and LGBTQI + associations, we were not able to have a proportion that allows a sexual identity comparison. However, our proportion of cismen equals that reported in the 2021 national incidence data [5]. Fourth, considering that access to health is closely linked to employment in Mexico [31], it may have been pertinent to include employment-based HIV stigma-related questions. However, we opted not to include a different source of stigma that was not originally included in the conceptual framework. Finally, we did not include questions regarding treatment adherence and CD4 count. We suggest future studies regarding HIV-related stigma include a more thorough questionnaire than what a psychometric study such as the present article may include.
Conclusion
Psychometric properties indicate that the 5- factor structure of the HIV mechanisms of stigma scale is a valid instrument that may be used among the Mexican population living with HIV. This scale may be used to explore the role stigma is currently playing in access to care, treatment adherence, and other social barriers that harm PLWH.
Data Availability
The data that support the findings of this study are available upon request.
Code Availability
Not applicable.
References
Florom-Smith AL, De Santis JP. Exploring the Concept of HIV-Related Stigma. Nurs Forum. 2012;47(3):153–65.
Earnshaw VA, Chaudoir SR. From Conceptualizing to Measuring HIV Stigma: A Review of HIV Stigma Mechanism Measures. AIDS Behav. 2009;13(6):1160.
Deacon H. Towards a sustainable theory of health-related stigma: lessons from the HIV/AIDS literature. J Community Appl Social Psychol. 2006;16(6):418–25.
Smith MK, Xu RH, Hunt SL, Wei C, Tucker JD, Tang W, et al. Combating HIV stigma in low- and middle-income healthcare settings: a scoping review. J Int AIDS Soc. 2020;23(8):e25553.
Ceballos S, Carbajal G, Arellanos Y, Ramirez G, Martinez A. Sistema de vigilancia epidemiológica de VIH. Mexico: Government of Mexico; 2021.
Hernandez-Avila JE, Palacio-Mejia L, Hernandez-Romieu AC, Bautista-Arredondo SA, Sepulveda J, Hernandez-Avila M. Effect of universal access to antiretroviral therapy on HIV/AIDS mortality in Mexico 1990 2011. JAIDS. 2015;69(3):e100-e8.
Hernandez-Romieu AC, del Rio C, Hernandez-Avila JE, Lopez-Gatell H, Izazola-Licea JA, Uribe Zuniga P, et al. CD4 Counts at Entry to HIV Care in Mexico for Patients under the “Universal Antiretroviral Treatment Program for the Uninsured Population,“ 2007–2014. PLoS ONE. 2016;11(3):e0152444.
Torres-Cruz C, Suarez-Diaz E. The stratified biomedicalization of HIV prevention in Mexico City. Glob Public Health. 2020;15(4):598–610.
Pitpitan EV, Mittal ML, Smith LR. Perceived Need and Acceptability of a Community-Based Peer Navigator Model to Engage Key Populations in HIV Care in Tijuana, Mexico. J Int Assoc Provid AIDS Care. 2020;19:2325958220919276.
Herrera C, Campero L, Caballero M, Kendall T. Relationship between physicians and HIV patients: influence on adherence and quality of life. Rev Saude Publica. 2008;42(2):249–55.
Wolff MJ, Cortes CP, Mejìa FA, Padgett D, Belaunzarán-Zamudio P, Grinsztejn B, et al. Evaluating the care cascade after antiretroviral therapy initiation in Latin America. Int J STD AIDS. 2018;29(1):4–12.
Earnshaw VA, Smith LR, Chaudoir SR, Amico KR, Copenhaver MM. HIV stigma mechanisms and well-being among PLWH: a test of the HIV stigma framework. AIDS Behav. 2013;17(5):1785–95.
INEGI. Employed population according to income level, quarterly national Mexico: INEGI. National Occupation and Employment Survey (ENOE); 2022 [updated May 23, 2022. Available from: https://www.inegi.org.mx/app/tabulados/default.html?nc=602.
Survio. Czech Republic: Survio s.r.o; 2012 [Available from: https://www.survio.com/en/about-us.
Streiner DL, N GR, Cariney J. Health measurement scales: a practical guide to their development and use. 5 ed.: Oxford University Press; 2015.
Raiche G, Magis D, Raiche MG. Package ‘nFactors’: Repository CRAN; 2020.
Lloret-Segura S, Ferreres-Traver A, Hernández-Baeza A, Tomás-Marco I. El análisis factorial exploratorio de los ítems: una guía práctica, revisada y actualizada. Anales de Psicología. 2014;30(3):1151–69.
Perry HB, Zulliger R, Rogers MM. Community health workers in low-, middle-, and high-income countries: an overview of their history, recent evolution, and current effectiveness. Annu Rev Public Health. 2014;35(1):399–421.
Revelle W. How toow to: Use the psych package for factor analysis and data reduction. Evanston: Northwestern University, Department of Psychology; 2021.
Valle A, Trevino AC, Zambrano FF, Urriola KE, Sanchez LA, Elizondo JE. Perceived HIV-associated stigma among HIV-seropositive men: psychometric study of HIV stigma scale. Front Public Health. 2015;3:171.
Azamar A, Bautista-Arredondo SA, Smaill F, Mbuagbaw L, Costa AP, Tarride J-E. Patient characteristics and determinants of CD4 at diagnosis of HIV in Mexico from 2008 to 2017: a 10-year population-based study. AIDS Research and Therapy. 2021;18.
Sierra-Madero JG, Belaunzaran-Zamudio PF, Crabtree-Ramírez B, Magis-Rodriguez C. Mexico’s fragmented health system as a barrier to HIV care. The Lancet HIV. 2019;6(2):e74-e5.
Blake Helms C, Turan JM, Atkins G, Kempf M-C, Clay OJ, Raper JL, et al. Interpersonal Mechanisms Contributing to the Association Between HIV-Related Internalized Stigma and Medication Adherence. AIDS Behav. 2017;21(1):238–47.
Yigit I, Bayramoglu Y, Weiser SD, Johnson MO, Mugavero MJ, Turan JM, et al. Changes in Internalized Stigma and HIV Health Outcomes in Individuals New to HIV Care: The Mediating Roles of Depression and Treatment Self-Efficacy. AIDS Patient Care STDs. 2020;34(11):491–7.
Lee RS, Kochman A, Sikkema KJ. Internalized Stigma Among People Living with HIV-AIDS. AIDS Behav. 2002;6(4):309–19.
Poindexter CC, Shippy RA. HIV Diagnosis Disclosure: Stigma Management and Stigma Resistance. J Gerontol Soc Work. 2010;53(4):366–81.
INEGI. Internet use in Mexico: Government of Mexico; 2021 [Available from: https://www.inegi.org.mx/contenidos/saladeprensa/boletines/2021/OtrTemEcon/ENDUTIH_2020.pdf.
Martínez-Vélez NA, Tiburcio M, Natera Rey G, Villatoro Velázquez JA, Arroyo-Belmonte M, Sánchez-Hernández GY, et al. Psychoactive substance use and its relationship to stress, emotional state, depressive symptomatology, and perceived threat during the COVID-19 pandemic in Mexico. Front Public Health. 2021;9:709410-.
Ramos-Lira L, Rafful C, Flores-Celis K, Mora Ríos J, García-Andrade C, Rascón Gasca ML, et al. Emotional responses and coping strategies in adult Mexican population during the first lockdown of the COVID-19 pandemic: gender differences matter. Salud Mental. 2020;43(6):243–51.
Evans AR, Elford J, Bolding G, Wiggins RD. A comparison of item non-response in web and pen-and-paper surveys of sexual behaviour. Methodological Innovations Online. 2008;2(3):6–17.
Knaul FM, González-Pier E, Gómez-Dantés O, García-Junco D, Arreola-Ornelas H, Barraza-Llareéns M, et al. The quest for universal health coverage: achieving social protection for all in Mexico. The Lancet. 2012;380:1259–79.
Acknowledgements
The authors gratefully acknowledge the contributions to this research by the study participants. Data collection would not had been possible without the support of the following fellow researchers: Ricardo Baruch, Alexa Daza, Adriana Villafuerte, Andrés Gaeta, and Carlos Magis; and NGOs that provide services to persons that live with HIV, including: Casa David, Desnúdate, Ofender la Sociedad, Mesa de dibujo para personas con VIH, Aspros, Clínica Especializada Condesa, VIH CDMX, VIHve Libre, Casa de la Sal, Brigada Callejera de Apoyo a la Mujer “Elisa Martínez”, CEAVIH, YAAJ, Checcos, Fundación México Vivo, El Armario Abierto, VIH/Sida Latinoamérica, ¿Hablamos de VIH? ¿Yde sida?, +VIH, PrEP en México, and MEXFAM.
Funding
This study was supported by a PAPIIT IA301320.
Author information
Authors and Affiliations
Contributions
All authors had full access to all data and have read and approved the text as submitted. AL performed statistical analyses, CR drafted the manuscript, RO supervised the statistical analyses, JACV, MM, and LJ contributed to manuscript revisions.
Corresponding author
Ethics declarations
Conflict of Interest
The authors report no conflicts of interest.
Ethics Approval
This study was approved by the Ethics Committee of the Faculty of Psychology at the Universidad Nacional Autónoma de México.
Consent to Participate
All participants individually provided their informed consent prior to responding the questionnaire.
Consent for Publication
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Andrea López and Claudia Rafful contributed equally to the work.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
López, A., Rafful, C., Orozco, R. et al. HIV Stigma Mechanisms Scale: Factor Structure, Reliability, and Validity in Mexican Adults. AIDS Behav 27, 1321–1328 (2023). https://doi.org/10.1007/s10461-022-03868-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-022-03868-2