Abstract
The Evidence for Contraceptive Options and HIV Outcomes (ECHO) trial found no substantial difference in HIV acquisition risk between women randomised to injectable intramuscular depot medroxyprogesterone acetate (DMPA-IM), copper intrauterine device (Cu-IUD) or the levonorgestrel (LNG) implant. We evaluated post-randomization sexual behavior using an objective marker of condomless vaginal sex in a subset of participants. We conducted a sub-study among 458 ECHO participants at three sites (Cape Town, Johannesburg, Kisumu) to evaluate the frequency of condomless vaginal sex, measured by prostate specific antigen (PSA) detection in vaginal swabs, collected at the month 6 and final visit and the concordance of self-reported condomless vaginal sex with PSA detection, by randomized arm. We compared PSA detection frequency and concordance of PSA and self-reported condomless vaginal sex, by randomized group using Cochran–Mantel–Haenszel tests and adjusted generalized logistic growth curve models. PSA was detected less frequently in the DMPA-IM (16%), compared to the Cu-IUD (21%) and LNG implant (24%) groups, although results were not statistically significant in the unadjusted model when accounting for pre-specified multiple-testing criteria. There were significant differences in PSA detection between the DMPA-IM and LNG-implant groups (odds ratio 0.61 (95% CI 0.40, 0.94) in the adjusted model. There was moderate discordance between self-reported condomless vaginal sex and detection of PSA that was similar across randomized groups. These data suggest that women randomized to Cu-IUD and LNG implant may have had condomless sex more frequently than women randomized to DMPA-IM. The discordance between detectable PSA and self-reported sexual behaviour has important implications for design of future HIV prevention studies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The Evidence for Contraceptive Options and HIV Outcomes (ECHO) trial, which randomized women to three different contraceptive methods including intramuscular injectable depot medroxyprogesterone acetate (DMPA-IM), a copper intrauterine device (Cu-IUD) and a levonorgestrel (LNG) implant, found no significant differences in HIV acquisition between the contraceptive methods. Due to the nature of the contraceptive methods under study, neither study participants nor research staff at the study sites were blinded. We aimed to evaluate whether there were any post-randomization differences in condomless vaginal sex (hereafter sexual behavior), and thus potentially to HIV exposure, by randomized contraceptive group using prostate specific antigen (PSA) as an objective marker of recent condomless vaginal sex. PSA has been used in multiple studies as a valid proxy measure for recent condomless vaginal sex and is detectable in vaginal fluid immediately following condomless vaginal sex, and generally returns to undetectable levels within 48 h [1, 2]. We also compared detection of PSA to participant self-reported sexual behavior data to understand the accuracy of self-reported data in this context.
Methods
Study Design, Participants and Ethics
The ECHO Trial (clinicaltrials.gov ID NCT02550067) randomized 7829 HIV-seronegative women to either DMPA-IM, Cu-IUD or LNG implant, from December 2015 through September 2017 [3]. We conducted a prospective sub-study among ECHO trial participants to evaluate the frequency of condomless vaginal sex, as measured by detection of PSA in vaginal swabs, and the correlation of self-reported sexual behaviour with PSA detection, by randomized arm. The participants included in these analyses were those who consented to vaginal sample collection through an ancillary biological mechanisms study nested within ECHO to understand the impact of the study contraceptive methods on biological mechanisms of HIV acquisition. This sub study was conducted at three of the twelve ECHO trial sites including the Desmond Tutu HIV Centre, Cape Town and Wits Reproductive Health and HIV Institute, Johannesburg, South Africa and Kenya Medical Research Institute, Kisumu, Kenya [4]. To be eligible, participants had to have: (1) complete ECHO trial demographic (baseline; for identification of participant age) and self-reported sexual behaviour data (month six and final study visit conducted 12–18 months after enrolment) [3], (2) valid baseline and final visit nucleic acid amplification test (NAAT) results for Chlamydia trachomatis and Neisseria gonorrhoeae, (3) used their randomized contraceptive method for their duration of trial participation, and (4) stored vaginal specimens at the month six and final study visits.
This research was implemented in accordance with the Declaration of Helsinki and Good Clinical Practice. Institutional review boards at FHI 360, the University of Washington and each clinical site approved the study protocol and women provided written informed consent for future research on their biological samples.
Specimen Collection and Analysis
Clinical staff collected a lateral vaginal wall swab from participants at each follow-up visit; swabs were stored dry at − 80 °C until analysis. We analysed swabs collected at the month six and final study visits for PSA at the University of North Carolina at Chapel Hill (UNC). Trained laboratory staff eluted lateral vaginal wall swabs into phosphate-buffered saline and centrifuged suspensions to separate cellular material and soluble contents (including PSA) in the supernatant using Isohelix Spin + Collect SC150-SPIN Devices. Eluate was diluted 1:10 with PBS and tested for PSA using the ABAcard p30 rapid immunochromatographic strip test (Abacus Diagnostics, West Hill, CA; lower limit of detection 4 ng PSA/ml) as previously described [1].
Statistical Analysis
Under the assumption of an average 20% PSA positivity rate at each follow-up time point, and accounting for 20% correlation between repeated measures and type 1 error rate adjustment due to multiple comparisons between randomized groups, our a priori assessment suggested that a sample size of 450 (150 per group) would provide > 90% power to detect a 15% difference in PSA detection between randomized groups. To investigate differences in the frequency of condomless vaginal sex between randomized contraceptive groups, we calculated the frequency of PSA detection at the month six and final study visits. We then compared the proportion of PSA positive specimens by randomized contraceptive group at the month six and final visits separately using the Cochran–Mantel–Haenszel test stratified by study site with Bonferroni correction. We used a generalized logistic growth curve model adjusting for site, age (continuous) and specimen collection order to evaluate whether the proportion of PSA positive specimens differed significantly by randomized group and/or over time. We evaluated the concordance of self-reported sexual behaviour data and PSA detection in two ways by randomized study group: (1) the proportion of women who reported no vaginal sex, or only condom-protected vaginal sex in the past seven days, who had detectable PSA, and (2) the proportion of women who reported their last vaginal sex act to have been within 3 days with a condom, or reported their last vaginal sex act to have been ≥ 4 days ago whether or not they report condom use during that last act, who had detectable PSA. Using these data, we estimated the proportion of potential misreporting, and associated 95% confidence interval, overall and by randomized contraceptive group at the month 6 and final visits individually and jointly. The same statistical analysis approaches described above were used to compare potential misreporting by randomized contraceptive method and to evaluate whether the proportion of potential misreporting differed by group and over time. All data analyses were conducted using SAS version 9.4 (Cary, NC, USA).
Participant and Public Involvement
The ECHO trial was designed over several years through an extensive consultative process with a range of stakeholders that included women’s health advocates. The trial’s Global Community Advisory Group (GCAG), which included advocates for women’s health and rights from each of the countries where the study was conducted, advised the ECHO Consortium on the trial protocol. The conduct of the trial was monitored through site-specific Good Participatory Practice plans designed to operationalize the GPP principles of respect, transparency, accountability, and community stakeholder autonomy.
Results
Participant Characteristics
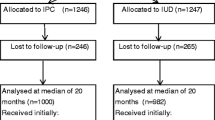
A total of 558 randomized participants had stored month 6 and final visit samples available for analysis at the three participating sites. Among those, 458 met the aforementioned inclusion criteria and were included in this analysis, including 145 in the DMPA-IM group, 158 in the Cu-IUD group and 155 in the LNG implant group. Baseline characteristics were similar across groups (Table 1). The median age of participants was 23 years, about half (50.9%) were married and had completed any secondary school (54.6%). Participants reported a median of 10 vaginal sex acts per month in the three months prior to enrolment, the vast majority (96.9%) reported having had the same primary sex partner during that period and most (73.3%) women reported having had any unprotected sex. The prevalences of Chlamydia trachomatis and Neisseria gonorrhoeae were 15.5% and 4.1% respectively at baseline, with no significant differences by randomized group. Analysis of these baseline demographic, sexual behavior and STI prevalence data found no statistically significant differences between this sub-sample of ECHO trial participants and the overall trial population (data not shown).
PSA Detection During Follow-Up
PSA was detected in 17.6% of month 6 and 23.4% of final visit vaginal swab specimens (Fig. 1). In general, women in the DMPA-IM group were less likely to have PSA detected at both the month 6 and final visits (15.5% and 17.2%) as compared to women in the Cu-IUD (17.1% and 25.5%) or LNG implant groups (20.0% and 27.1%, Table 2). When pooling across visits, women in the DMPA-IM group had 29% lower odds [odd ratio (OR) 0.71, 95% CI 0.46, 1.06)] of PSA detection compared to the copper IUD group and 39% lower odds [OR 0.61 (0.40, 0.94) compared to the LNG implant group. Women in the Cu-IUD arm had 13% lower odds of PSA detection than women in the LNG implant group (OR 0.87 (0.59, 1.31)]. Across all arms, women were significantly more likely to have PSA detected at the final visit relative to the month 6 visit [OR 1.44 (1.05, 1.98)].
Correlation of PSA Detection and Self-reported Sexual Behavior
There was moderate discordance between self-reported sexual behavior and PSA results (Table 3). Of the women with detectable PSA at month 6 indicating condomless sex in the past 7 days (N = 80), 19% reported having had no vaginal sex, or only vaginal sex with a condom, in the past 7 days. Furthermore, 7.8% percent of women with detectable PSA at month 6 reported no vaginal sex in the past 7 days. Slightly higher discordance was observed at the final visit with 20 (25%) of the women with detectable PSA reporting no vaginal sex, or only vaginal sex with a condom, in the past 7 days. Sixteen percent of women with detectable PSA reported no vaginal sex in the past 7 days. There were no significant differences in discordance between randomized contraceptive groups [DMPA vs. Cu IUD OR 1.27 (95% CI 0.48, 3.34); DMPA vs. implant OR 1.72 (0.61, 4.86); IUD vs. implant OR 1.36 (95% CI 0.52, 3.55)].
Discussion
These data suggest that the frequency of condomless sex may have differed by randomized contraceptive method among ECHO trial participants at the 3 (out of 12 total) ECHO sites in this sub-study. By objectively measuring condomless sex, these data confirm the prior suggestion of differences in by-arm sexual behavior that were generated from self-reported data [3]. Any true differences in sexual behavior by randomized contraceptive group could be due to side effects of the contraceptives, differences in vaginal practices and/or differential concerns about HIV risk. The contraceptive methods under study in ECHO have side effect profiles that could differentially affect women’s sexual behavior. DMPA-IM is associated with irregular bleeding and reduced libido which could result in decreased sexual frequency and thereby explain the lower PSA detection in that group [5]. However, both the Cu-IUD and LNG implant are also associated with bleeding irregularities, including amenorrhea, irregular bleeding, heavy bleeding and prolonged bleeding [6, 7]. The bleeding pattern irregularities with these methods tend to differ over time, thus making it difficult to draw conclusions about the impact of bleeding differences on sexual behavior by contraceptive arm. It is also possible that women in the DMPA-IM arm engaged in less frequent sex and/or more condom use due to concerns about HIV risk. While the informed consent process described that the study objective was to understand if any of the three contraceptive methods change a woman’s risk of HIV, it also explained that the World Health Organization stated (at the time) that there was evidence of a possible increased risk of HIV acquisition associated with DMPA-IM. It is therefore plausible that women in the DMPA-IM arm may have modified their sexual behavior due to concerns about HIV risk.
There are important limitations to this analysis that must be considered in interpretation of the results. While we did not observe any statistically significant differences in baseline demographic, sexual behavior or STI prevalence by randomized contraceptive group between the women in this sub-study as compared to the overall trial population, this sub-study represents only 6% of the total trial population. Moreover, the selection criteria for inclusion in this sub-study required that women have remained on their randomized contraceptive method through their final visit. It is possible that women in this sub-study differed in unknown ways correlated with sexual behavior that are not generalizable to the full trial population or the larger population of women represented by trial participants.
Importantly, the data from this study highlight reliability concerns with self-reported sexual behavior. While PSA is not a perfect surrogate for recent condomless vaginal sex due to inter- and intra-person variability PSA clearance kinetics, the self-reported measures we selected for comparison with PSA detection were robust. Specifically, between 8 and 16% of women with PSA detected reported not having any vaginal sex in the prior 7 days and PSA kinetic data clearly exclude detection of PSA at that timepoint [2]. The interpretation of PSA detection among women who reported no, or condom-only protected sex, in the last 7 days is more subject to error since women were not specifically asked about vaginal sex acts in which a condom was used for the entire duration of vaginal sex. Nonetheless, the data suggest that studies which rely on self-reported sexual behavior should consider validation against reliable biological indicators of recent condomless vaginal sex.
In conclusion, the results of this sub-study suggest that the frequency of condomless vaginal sex may have differed between randomized contraceptive groups in the ECHO trial. Notably, the ECHO trial was designed to evaluate whether there are differences in the risk of HIV acquisition among women randomized to DMPA-IM, the Cu-IUD and the LNG implant, and the trial accomplished that objective. While the trial was not designed to evaluate the biological effect of the randomized contraceptive methods on HV risk, the results from a causal analysis which adjusted for self-reported sexual behaviour generated results consistent with the intention-to-treat results [3]. The results of this sub-study suggest that inaccuracies in participant self-reported sexual behavior could have resulted in residual confounding of the causal analysis.
Data Availability (Data Transparency)
Access to data from this ancillary study of the ECHO Study may be requested through submission of a research concept to: jdeese@rti.org. Access will be granted if the concept is evaluated to have scientific merit and if sufficient data protections are in place. As of the time of publication, data access applications are in process with the governing institutional review boards of the ECHO Study to make de-identified data from the full trial publicly available.
Code Availability (Software Application or Custom Code)
Access to code from this ancillary study of the ECHO Study may be requested through submission of a request: jdeese@rti.org.
References
Hobbs MM, Steiner MJ, Rich KD, et al. Good performance of rapid prostate-specific antigen test for detection of semen exposure in women: implications for qualitative research. Sex Transm Dis. 2009;36(8):501–6.
Macaluso M, Lawson L, Akers R, et al. Prostate-specific antigen in vaginal fluid as a biologic marker of condom failure. Contraception. 1999;59(3):195–201.
Evidence for Contraceptive Options and HIV Outcomes Consortium. HIV incidence among women using intramuscular depot medroxyprogesterone acetate, a copper intrauterine device, or a levonorgestrel implant for contraception: a randomised, multicentre, open-label trial. Lancet. 2019;394(10195):303–13.
Scoville C, Palanee-Phillips T, Nair L, et al. Acceptability of genital mucosal sampling nested within a randomized contraceptive trial among women in Africa. Madrid: HIV Research for Prevention; 2018.
Dianat S, Fox E, Ahrens KA, et al. Side effects and health benefits of depot medroxyprogesterone acetate: a systematic review. Obstet Gynecol. 2019;133(2):332–41.
Hubacher D, Chen PL, Park S. Side effects from the copper IUD: do they decrease over time? Contraception. 2009;79(5):356–62.
Ali M, Akin A, Bahamondes L, et al. Extended use up to 5 years of the etonogestrel-releasing subdermal contraceptive implant: comparison to levonorgestrel-releasing subdermal implant. Hum Reprod. 2016;31(11):2491–8.
Acknowledgements
We thank the women who participated in this study for their motivation and dedication and the communities that supported this work.
Funding
The research reported in this publication was supported by the Eunice Kennedy Shriver National Institute of Child Health & Human Development of the National Institutes of Health under Award Number R21HD095708. Sample collection for the sub-study was supported by National Institute of Child Health & Human Development award number R01HD089831. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The Evidence for Contraceptive Options and HIV Outcomes (ECHO) Trial was supported by the combined generous support of the Bill & Melinda Gates Foundation [Grant OPP1032115]; the American people through the United States Agency for International Development [Grant AID-OAA-A-15-00045]; the Swedish International Development Cooperation Agency [Grant 2017/762965-0]; the South Africa Medical Research Council; and the United Nations Population Fund. Contraceptive supplies were donated by the Government of South Africa and US Agency for International Development. The contents of this paper are solely the responsibility of the authors and do not necessarily reflect the views, decisions or policies of the institutions with which they are affiliated, the ECHO trial funders, or the supporting governments.
Author information
Authors and Affiliations
Contributions
JD conceptualized and designed the study. XG and PC analyzed the data. MH provided oversight of laboratory testing; DH conducted prostate specific antigen testing. AM managed project implementation. All authors contributed equally to results interpretation. JD drafted the manuscript, and all authors approved the final version.
Corresponding author
Ethics declarations
Conflict of interest
No authors have any conflicts of interest.
Ethical Approval (Include Appropriate Approvals or Waivers)
This research was implemented in accordance with the Declaration of Helsinki and Good Clinical Practice. Institutional review boards at FHI 360, the University of Washington and each clinical site approved the study protocol.
Consent to Participate (Include Appropriate Consent Statements)
All participants provided written informed consent for future research on their biological samples.
Consent for Publication (Consent Statement Regarding Publishing an Individual’s Data or Image)
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Deese, J., Chen, P.L., Gao, X. et al. Post-randomization Differences in Condomless Vaginal Sex Among Women Randomized to Intramuscular Depot Medroxyprogesterone Acetate Injections, a Copper Intrauterine Device or a Levonorgestrel Implant in the ECHO Trial. AIDS Behav 27, 978–983 (2023). https://doi.org/10.1007/s10461-022-03834-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-022-03834-y