Abstract
Men who have sex with men (MSM) often change sexual behaviors following HIV diagnosis. This systematic review examined such changes, including sero-adaptive behaviors (i.e., deliberate safer-sex practices to reduce transmission risk) to better understand the magnitude of their association with HIV diagnosis. We searched four databases (1996–2017) and reviewed references from other systematic reviews. We included studies conducted in the United States that compared sexual behavior among HIV-infected “aware” versus “unaware” MSM. We meta-analytically pooled RRs and associated 95% confidence intervals (CI) using random-effects models, and assessed risk of bias and evidence quality. Twenty studies reported k = 131 effect sizes on sexual practices outcomes, most of which reported changes in unprotected sex (k = 85), and on sex with at-risk partners (k = 76); 11 reported sero-adaptive behaviors. Unprotected anal intercourse with an HIV-uninfected/unknown-status partner was less likely among aware MSM (insertive position: k = 2, RR 0.26, 95% CI 0.17, 0.41; receptive position: k = 2, RR 0.53, 95% CI 0.37, 0.77). Risk of not always serosorting among aware MSM (k = 3) was RR = 0.92 (0.83, 1.02). Existing evidence, although low-quality, suggests that HIV-infected MSM tend to adopt safer sexual practices once aware of their diagnosis. Variation in reporting of outcomes limits their comparability. Sero-adaptive behavior data are sparse.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Men who have sex with men (MSM) are the group at greatest risk for HIV infection in the United States (US), comprising more than half of known cases of HIV and an even greater majority (67%) of new HIV infections, according to current surveillance data [1]. Thus, effective HIV prevention strategies targeting MSM are critical to addressing the national burden of HIV. Advances in biomedical HIV prevention strategies stand to protect anyone at risk but in the absence of ideal adherence and efficacy, behavior change remains essential to successful prevention: while uptake of pre-exposure prophylaxis (PrEP) has increased [2], PrEP coverage among MSM at risk of HIV infection is 35–63% [2, 3]. Further, even though antiretroviral therapy (ART) can lead to viral suppression that essentially eliminates transmission risk [4], risk of HIV persists for the many MSM who do not enter treatment right away (28% in 2017) [5] and among those who do not maintain viral suppression [6]. In a recent analysis, only 48.4% of people living with HIV for more than one year in the US were found to have sustained viral suppression [7]. Thus, the ability to make sexual risk decisions based on knowledge of one’s HIV status is a necessary component to interrupting HIV transmission. Similarly, understanding post-diagnosis behavior-change provides critical insight to prevention-strategy planning.
Research has documented a reduction in risky sexual behavior among MSM newly diagnosed with HIV [8, 9]. This includes adopting or increasing standard safer sex practices in general (e.g., condom use, abstinence, etc.) as well as considering a partner’s HIV status when making sexual risk decisions. Some research has examined the practice and community recognition of “sero-adaptive” behaviors among MSM who choose less-risky sexual behaviors with HIV-uninfected partners. This includes “serosorting”—limiting sexual partners to people with concordant HIV status—and “sero-positioning” (also called “strategic positioning”)—where HIV-infected MSM adopt the riskier, receptive role in anal sex with partners who are HIV-uninfected [10,11,12,13]. Substantially more research has investigated MSM sexual activity by partner’s HIV status but without considering specifically sero-adaptive practices. All of these research domains contribute to understanding HIV transmission dynamics among MSM, with sero-adaptive categories providing the greatest specificity. Figure 1 illustrates the categorization of and relationships among these various behaviors.
A comprehensive understanding of the effect of HIV diagnosis on sexual risk behavior change must consider sero-adaptive behaviors along with other safer sex practices. Previous systematic reviews have studied serosorting among MSM receiving negative HIV-test results, but not positive results [14, 15]. Other reviews, including one of our own, have examined change in condom use among various groups, including MSM, after receiving an HIV diagnosis [8, 16, 17] but none have specifically analyzed all sero-adaptive and safer-sex behaviors among HIV-infected MSM. Here, we evaluate and present the evidence base for the effect of HIV diagnosis on all sexual risk behaviors among MSM in the US, with meta-analysis where sufficient data were available.
Methods
This review was based on methods of the Cochrane Collaboration [18]. We developed and followed a protocol we registered in the PROSPERO International Prospective Register of Systematic Reviews (CRD42018085282) [19]. We followed Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines for reporting [20]. We used the Grading of Recommendations Assessment, Development and Evaluation Guideline (GRADE) tool to assess evidence quality by outcome across the literature [21].
Study Eligibility
We included studies conducted in the US that compared sexual risk behaviors of HIV-infected adult or adolescent MSM aware of their infection versus MSM who were unaware of their infection. Study populations could be of any antiretroviral therapy (ART) status. We excluded studies with data collection completed before 1996, when triple-ART regimens became widely available in the US.
We included any study designs that clearly indicated timing of HIV diagnosis and assessment of outcomes to allow pre- and post-HIV diagnosis comparisons. We included studies that either compared HIV-infected aware MSM vs. HIV-infected but unaware MSM (between-group comparison), or compared HIV-infected MSM before knowledge of diagnosis vs. after receiving diagnosis (within-group comparison). We excluded studies that did not report quantitative epidemiological data (e.g., modeling) or were not rigorously peer-reviewed (e.g., unpublished data, conference proceedings).
Eligible studies could report on ways HIV-infected MSM changed their sexual behavior to account for a partners’ HIV status or on change in sexual behavior overall, which might reflect deliberate efforts to reduce risk but could be due to other factors (e.g., reduced sexual activity due to depression). Figure 1 illustrates eligible outcomes and their interrelationships. Sexual acts included in this review were condom use (overall, for anal sex overall, or for anal sex by role; reported as always using condoms or as the likelihood of using a condom based on condom use reported at last sex), any sex (also reported as abstinence), oral sex, anal sex (overall or by sexual role), withdrawal before ejaculation, number of partners, and number of sex acts.
For the purpose of this review, we defined sero-adaptive behaviors (as opposed to ‘general sexual acts’) when outcomes were measured in a way that could explicitly capture deliberate risk reduction including: serosorting (sex exclusively with sero-concordant partners), seropositioning (anal sex with serodiscordant partners with the HIV-infected partner exclusively in the receptive role), condom serosorting or condom seropositioning (where unprotected sex was restricted as above, but was not necessarily restricted when condoms were used), and oral sex serosorting (where anal sex was restricted as above, but oral sex was not necessarily restricted). We also regarded as sero-adaptive outcomes: (a) the encouragement of an HIV-uninfected partner to take PrEP by an HIV-infected partner or (b) basing sexual decisions on viral load.
Searches and Screening
We searched PubMed, Embase, PsycInfo, and Web of Science databases using keywords for study design, sexual risk behaviors, MSM populations, and HIV (Supplemental digital content A). The search period for all databases was January 1, 1996–January 15, 2018. We also reviewed references in included papers to identify additional studies. Finally, we included studies from Malekinejad et al. 2021 [16], our recently-completed review on condom use behavior among newly-HIV diagnosed people of any risk group when those studies met the criteria for this review.
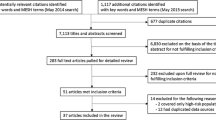
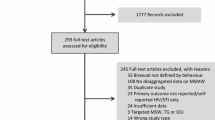
We imported all primary records from the database searches into EndNote software version X8 [22]. One reviewer used the search function in EndNote to locate titles with keywords that were likely irrelevant (e.g., “qualitative,” “in-vitro,” see Fig. 2) and reviewed the titles and, if relevant, the abstracts of those records. The two reviewers then independently examined the remaining record titles and, if relevant, abstracts and keywords. The first reviewer also sorted records by study location and excluded studies performed outside of the US. Reviewers resolved incongruent ratings via discussion. They evaluated the full text of included studies independently. A third reviewer was available to resolve disagreements and ambiguities.
Data Extraction and Standardization
We used a pre-structured data collection spreadsheet to capture the following: study details (e.g., complete citation, geographical setting, study design); descriptions of participants (e.g., age, sex, relevant demographic characteristics); details of HIV testing and comparators (e.g., location and means of HIV testing, HIV testing setting and context, comparison type); outcome definitions and descriptions; details of outcome assessment methods; recruitment methods and eligibility criteria; length of follow-up (time since diagnosis); and data necessary for assessing risk of bias. One reviewer extracted all data, which the second reviewer subsequently reviewed and cross-checked against full-text papers. The two reviewers discussed any disagreements and/or consulted a third rater to adjudicate. When needed, they contacted authors to obtain important missing information from the reports.
Assessment of Risk of Bias and Quality of Evidence
Two reviewers independently applied criteria recommended by the GRADE Working Group [21] for observational studies: failure of study investigators to develop and apply appropriate eligibility criteria; flawed measurement of exposure and outcome; failure to adequately control confounding; and inadequate follow-up. Each of these assessments helped us determine the quality of evidence for each report and outcome. Raters used a neutral third party to adjudicate disagreements. The quality of evidence was rated as high, unclear, or low based on risk of bias, indirectness, precision, and consistency [21].
Data Analysis and Synthesis
For dichotomous outcomes, we calculated risk ratios (RR) and 95% confidence intervals (CI). We used the Zhang and Yu method [23] to calculate RR when studies reported odds ratios (OR) for non-rare outcomes. When studies did not report 95% CI, we calculated 95% CI from p-values or from the number of persons with and without the outcome among HIV-infected aware and unaware conditions. For continuous variables, we reported mean difference (MD) and standard deviation (SD) or median and interquartile range (IQR) between the two groups.
To facilitate comparability of findings, we report all RR for undesirable behavior (e.g., unprotected sex instead of condom use). Thus, RR < 1 should be interpreted as decreased risk of undesirable outcomes throughout this review. When we identified two or more contextually compatible outcomes, we performed a meta-analysis using Stata version 14.2 [24]. We used a random-effects model to calculate the pooled effect sizes and 95% CI. We assessed statistical homogeneity using the I2 statistic, which reports the overall variation among the pooled data due to heterogeneity, rather than change alone, as a percent value [18]. Because some outcomes combined data on partners who were HIV-uninfected and of unknown HIV status [25], our meta-analyses combine these into a single “partner at risk” group; when studies reported separately on HIV-uninfected and unknown-status partners, we prioritized data for HIV-uninfected partners and report the pooled estimate using data for unknown-status partners in a footnote. Where data were available, we analyzed outcomes for participants on ART. To estimate long-term effects, we pooled data reported for intervals of 12 months or more; if studies reported multiple long-term intervals, we included the longest interval in meta-analysis.
Results
Descriptive Analysis
Study Screening Results
Our database search returned 4042 unique records, 3893 of which were excluded on the basis of title and/or abstract. We reviewed full text of the remaining 149 articles, and excluded 140 articles that did not meet the inclusion criteria. Of the remaining studies, one was a systematic review that further informed our search. Data from the other eight studies were included in our analysis. We also included data from 12 additional studies reviewed in Malekinejad et al. 2021 [16], resulting in a total of 20 studies. See Fig. 2 and Supplemental digital content B for details.
Characteristics of Included Studies
Of the 20 included studies, 13 were cross-sectional and seven had pre-post designs, one of which analyzed and reported data cross-sectionally. Data collection began as early as 1987 [26] and as recently as 2016 [27]. Four studies began prior to 1996. Two studies reported only approximate data collection dates.
Only three studies reported on serosorting [28,29,30], and one of these studies further differentiated between oral serosorting (serosorting for anal and not oral sex) and condom serosorting (serosorting for unprotected sex but not sex with condoms) [29]. One study reported on seropositioning, which was defined as seropositioning when not using condoms [29].
We reported outcomes by three groups of partner type, depending on the infected person’s knowledge of their partner’s HIV diagnosis. These included: partners who were at risk (n = 11; HIV-uninfected or HIV status not known to the HIV-infected partner), partners whose HIV status was not specified by the authors (n = 18), and partners who were both HIV-infected (n = 2).
Most (n = 13) studies did not report ART uptake among HIV-aware participants. Of those that did, median ART coverage (at follow-up, if reported separately for baseline and follow-up) was 75.8% (IQR 67.0–85.7%). Among prospective cohort studies, follow-up intervals varied from one month to eight years, although the two studies reporting both follow-up intervals and ART coverage had follow-up only at 12 months. Among seven cross-sectional studies that reported on time between HIV diagnosis and time of the sexual behavior in question, the median time interval was nine months (IQR 6.0–12.0 months).
Characteristics of Effect Sizes
From 20 studies, we identified a total of k = 131 eligible effect sizes in our analysis (see Table 1 and Supplemental digital content C). We observed great variation in the reported outcomes. Most (k = 86, 66%) effect sizes analyzed risk behavior categorically (e.g., the proportion of participants reporting any occurrence of risk behavior, Supplemental Digital Content C) while the remainder k = 45 reported continuous values (e.g., median number of partners, percentage of condom-protected sex acts, etc.). Seven effect sizes were reported at the sexual dyad level (enumerating partnerships by individual, not sex acts) and twelve reported on last sex or last partner while the remaining k = 112 reported on any outcome of interest during recall periods ranging from 1 to 96 months. Follow-up time was between 6 and 12 months for k = 37 effect sizes (28%), more than 12 months for k = 32 (24%), six months or less for k = 12 (9%), and not reported for k = 50 (38%) effect sizes.
The most commonly reported outcome was UAI, overall (k = 37, 28%) or by role (insertive: k = 26, 20%; receptive: k = 13, 10%). Eleven effect sizes reported sero-adaptive behaviors, five of which were serosorting. Studies also reported on unprotected sex overall (k = 9, 7%) and by number of sexual partners (k = 12, 9%); any anal sex (k = 10, 8%); any sex (k = 1, 1%); and sexual activity by partner HIV status (k = 47, 36%, partner at risk; k = 8, 6%, partner HIV-infected). Seventy-six effect sizes (58%) reported on sex with partners at risk, k = 47 (36%) on partners of unspecified HIV status, and k = 8 (6%) on sex with HIV-infected partners.
Effects of Being Aware of HIV Diagnosis on Sexual Behaviors
When Partners were at Risk
Of 76 effect sizes reporting sexual behavior with a partner at risk among aware vs. unaware HIV-infected MSM, we omitted k = 19 from analyses due to overlap. Figure 3a and Table 2 meta-analyzed estimates and unique effect sizes that could not be pooled. The meta-analyzed RR for not serosorting was 0.92 (k = 3, I2 = 64%, 95% CI 0.83, 1.02); one study reported an effect size for a long-term effect of 0.93 (95% CI 0.68, 1.28) [31]. The meta-analyzed RR for any unprotected sex episode with a partner at risk was 0.55 (k = 4, I2 = 37%, 95% CI 0.47, 0.64) and for any unprotected anal intercourse (UAI) with a partner at risk was 0.62 (k = 4, I2 = 91.1%, 95% CI 0.25, 1.52). Specific to sexual role, the meta-analyzed RR for insertive UAI with a partner at risk was 0.26 (k = 2, I2 = 0%, 95% CI 0.17, 0.41) and for receptive UAI with a partner at risk was 0.53 (k = 2, I2 = 0%, 95% CI 0.37, 0.77). When analysis was restricted to participants on ART, estimates were: insertive RR 0.29 (k = 2, I2 = 0%, 95% CI 0.19, 0.44); receptive RR 0.45 (k = 2, I2 = 50%, 95% CI 0.24, 0.84, see Fig. 3c).
Changes in sexual practices of men who have sex with men who became aware of HIV diagnosis in the United States. a Effect of HIV diagnosis on sexual behavior with partner at risk among MSM in the United States. b Effect of HIV diagnosis on sexual risk behaviors reported for follow-up intervals of 12 months or more among MSM in the United States. c Effect of HIV diagnosis on sexual behavior among participants on antiretroviral therapy among MSM in the United States
When data were restricted to follow-up intervals of 12 months or more, results for UAI with a partner at risk were RR 0.81, k = 3, I2 = 86%, 95% CI 0.28, 2.36 (see Fig. 3b). One study reported mean differences for having a discordant partnership as ranging from − 5.90 to − 1.40 over follow-up intervals of 12 to 96 months [27].
When Partners were HIV-Infected
Four different outcomes where both partners were HIV-infected were reported across four studies. The RR reported for the percentage of partners who were HIV infected before and after diagnosis was 0.60 (k = 1, 95% CI 0.36, 1.01) and for an episode of unprotected sex was 0.21 (k = 1, 95% CI 0.08, 0.53) [32]. The RR for any insertive UAI with an HIV-infected partner among aware vs. unaware MSM was 1.51 (k = 1, 95% CI 1.00, 2.28) and 2.66 (k = 1, 95% CI 1.60, 4.44) for receptive UAI with an HIV-infected partner [33].
When Partners’ HIV Status was not Specified
Eighteen studies reported k = 47 effect sizes for sexual behavior with a partner of unspecified HIV status. The meta-analyzed mean difference in number of partnerships was − 3.11 (k = 2, I2 = 13%, 95% CI − 5.33, − 0.90). Meta-analyzed RR for any anal sex was 0.96 (k = 3, I2 = 86%, 95% CI 0.92, 1.00) and for any UAI as 0.75 (k = 11, I2 = 89%, 95% CI 0.62, 0.91), and found a reduction in receptive UAI (RR 0.79, k = 2, I2 = 0%, 95% CI 0.64, 0.98). Long-term effects (follow-up intervals of 12 months or more) for any anal sex were RR 0.95 (k = 2, I2 = 91%, 95% CI 0.91, 0.99) and for any UAI were RR 0.96 (k = 2, I2 = 41%, 95% CI 0.87, 1.05, see Fig. 3b). When analysis was restricted to participants on ART, results for any UAI were RR 0.92 (k = 2, I2 = 95%, 95% CI 0.63, 1.34, see Fig. 3c).
Risk of Bias
We identified four study designs, described previously [16]. Studies included in this review included two kinds of within-group comparison pre-post designs, where participants were either recruited (n = 2) or self-selected (n = 5) for testing, as well as cross-sectional studies where participants were self-selected for testing (n = 13). See Supplemental digital content D.
Risk of bias was generally high or unclear, largely due to the observational nature of the studies and the need to rely on self-reported data. All studies were rated at high risk of bias in the category of measurement of exposure and/or outcome, due to self-reported outcomes. Additionally, most effect sizes were rated at high or unclear risk of bias in data completion (including description of exclusion criteria and attrition, 104, 79%), selective outcome reporting (89, 68%), control for confounders (89, 68%), and other unspecified bias (116, 89%). Low risk of bias was identified for all effect sizes regarding development and application of eligibility criteria, and for all but two effect sizes in follow-up time, which were unclear. (See Supplemental digital content E and F.)
Discussion
To our knowledge, this review is the first of its kind addressing the association between HIV diagnosis knowledge and a wide range of sexual practices. Prior reviews [14, 15] have examined behavior change among HIV-uninfected MSM who engage in serosorting to protect themselves from HIV infection, but not focused on MSM receiving HIV diagnoses whose behavior change intends to prevent onward transmission. We found limited data on serosorting and seropositioning, and more data on condom use, sexual activity and discordant partnerships. This review provides an assessment of sero-adaptive and other sexual risk behavior change among HIV-infected MSM after learning of their diagnosis.
HIV-infected aware MSM have a lower risk of UAI with partners at risk, compared to those not aware of their infection (RR = 0.62). The reduction in UAI risk was observed for both receptive (RR = 0.53) and insertive (RR = 0.26) anal sex. This suggests that knowledge of positive HIV status was an important factor in reducing UAI and, therefore, expanded HIV testing may result in lower risk behavior among MSM who would otherwise be unaware of their infection. MSM aware of their HIV infection are also less likely to report sex with partners at risk, irrespective of condom use and fewer sexual partners.
HIV-infected-aware participants on ART had a lower risk of engaging in UAI with partners at risk and with partners whose HIV status was unspecified in studies. This held true at long-term follow-up of 12 months or more, though neither of these findings were statistically significant.
This review found somewhat different results for UAI than our prior review of condom use among various risk groups [16]. For example, the prior review estimated the RR for UAI with a partner at risk among aware MSM as 0.46 (k = 6, I2 = 60%, 95% CI 0.30, 0.70) while this review estimated an RR of 0.62 (k = 4, I2 = 90%, 95% CI 0.26, 1.52). We attribute such differences to changes in eligibility criteria: specifically, the prior review included data collected in Canada as well as conference abstracts, whereas this review was restricted to peer-reviewed studies conducted in the US. Notably, this review searched for keywords and captured outcomes beyond condom use which, although seldom reported, provide additional context and detail for the MSM population.
Limitations of this review reflect the limitations of primary studies, primarily the limited body of evidence on sero-adaptive behaviors; also bias due to self-reported behavioral outcomes. Additionally, the variation in how sexual behavior was reported by primary studies limited the volume of data available for pooled estimates. For example, “serosorting” was defined in different studies as: any sex exclusively with sero-concordant partners [29]; UAI only with sero-concordant partners [28, 34]; or not using condoms with a partner of concordant HIV status (with no discussion of serodiscordant sexual contact) [35]. Within these definitions, “concordant” may refer either to actual HIV status at or before HIV diagnosis (i.e., sex with an HIV-infected partner [28, 34]) or perceived HIV status (i.e., sex with an HIV-uninfected partner [31]). Additionally, where general sexual acts were reported, it is possible that reported sexual activity and condom use reflected some sero-adaptive behavior (e.g., reports of any receptive anal intercourse (RAI) could include participants who engaged in seropositioning), but this cannot be known definitively. Similarly, data on any anal sex and any oral sex could capture participants who switched from anal sex to oral sex to reduce risk or those who engaged in oral sex serosorting.
Such complexity poses a challenge to understanding what effect HIV diagnosis truly has on risk behavior among MSM. In meta-analysis, we combined data with equivalent operational definitions. While transforming outcome data to RR facilitated comparability of findings across studies, many included studies are cross-sectional in design with limitations for developing a true estimate of risk. Further, given the diversity of the outcome types, it was prudent to apply a random-effects model to account for source of heterogeneity.
Finally, because few studies stratified results by participants’ ART status and no studies addressed PrEP use by HIV-uninfected partners, these factors are not fully addressed in our review.
Future research should attend to the above nuances and associated contextual factors in order to expand the body of evidence on sero-adaptive behaviors among MSM. In particular, studies should attempt to address pure serosorting and seropositioning behaviors—i.e., the degree to which UAI or insertive UAI is practiced with HIV-concordant partners at the exclusion of discordant partners. While existing data on “any” occurrence of sex with partners of each serostatus is helpful to both mathematical modeling and HIV prevention efforts, addressing the holistic context of participants’ sexual behavior through comprehensive data collection and analysis could further enhance HIV prevention strategies.
Data Availability
Upon request.
Code Availability
Not applicable.
References
CDC. Diagnoses of HIV infection in the United States and dependent areas, 2017. Atlanta: Centers for Disease Control and Prevention; 2018.
Finlayson T, Cha S, Xia M, Trujillo L, Denson D, Prejean J, et al. Changes in HIV preexposure prophylaxis awareness and use among men who have sex with men—20 urban areas, 2014 and 2017. MMWR Morb Mortal Wkly Rep. 2019;68(27):597–603.
Kanny D, Jeffries WLT, Chapin-Bardales J, Denning P, Cha S, Finlayson T, et al. Racial/ethnic disparities in HIV preexposure prophylaxis among men who have sex with men—23 urban areas, 2017. MMWR Morb Mortal Wkly Rep. 2019;68(37):801–6.
Rodger AJ, Cambiano V, Bruun T, Vernazza P, Collins S, Degen O, et al. Risk of HIV transmission through condomless sex in serodifferent gay couples with the HIV-positive partner taking suppressive antiretroviral therapy (PARTNER): final results of a multicentre, prospective, observational study. Lancet (London, England). 2019;393(10189):2428–38.
CDC. HIV infection risk, prevention, and testing behaviors among men who have sex with men—National HIV Behavioral Surveillance, 23 US cities, 2017. Atlanta: Centers for Disease Control and Prevention; 2019.
Li Z, Purcell DW, Sansom SL, Hayes D, Hall HI. Vital signs: HIV transmission along the continuum of care—United States, 2016. MMWR Morb Mortal Wkly Rep. 2019;68(11):267–72.
Crepaz N, Dong X, Wang X, Hernandez AL, Hall HI. Racial and ethnic disparities in sustained viral suppression and transmission risk potential among persons receiving HIV care—United States, 2014. MMWR Morb Mortal Wkly Rep. 2018;67(4):113–8.
Marks G, Crepaz N, Senterfitt JW, Janssen RS. Meta-analysis of high-risk sexual behavior in persons aware and unaware they are infected with HIV in the United States: implications for HIV prevention programs. J Acquir Immune Defic Syndr. 2005;39(4):446–53.
Vallabhaneni S, Li X, Vittinghoff E, Donnell D, Pilcher CD, Buchbinder SP. Seroadaptive practices: association with HIV acquisition among HIV-negative men who have sex with men. PLoS ONE. 2012;7(10): e45718.
Snowden JM, Raymond HF, McFarland W. Prevalence of seroadaptive behaviours of men who have sex with men, San Francisco, 2004. Sex Transm Infect. 2009;85(6):469–76.
Xia Q, Molitor F, Osmond DH, Tholandi M, Pollack LM, Ruiz JD, et al. Knowledge of sexual partner’s HIV serostatus and serosorting practices in a California population-based sample of men who have sex with men. AIDS. 2006;20(16):2081–9.
Parsons JT, Severino J, Nanin J, Punzalan JC, von Sternberg K, Missildine W, et al. Positive, negative, unknown: assumptions of HIV status among HIV-positive men who have sex with men. AIDS Educ Prev. 2006;18(2):139–49.
McFarland W, Chen Y-H, Nguyen B, Grasso M, Levine D, Stall R, et al. Behavior, intention or chance? A longitudinal study of HIV seroadaptive behaviors, abstinence and condom use. AIDS Behav. 2012;16(1):121–31.
Kennedy CE, Bernard LJ, Muessig KE, Konda KA, Akl EA, Lo YR, et al. Serosorting and HIV/STI infection among HIV-Negative MSM and transgender people: a systematic review and meta-analysis to inform WHO guidelines. J Sex Transm Dis. 2013;2013: 583627.
Purcell DW, Higa D, Mizuno Y, Lyles C. Quantifying the harms and benefits from serosorting among HIV-negative gay and bisexual men: a systematic review and meta-analysis. AIDS Behav. 2017;21(10):2835–43.
Malekinejad M, Blodgett J, Horvath H, Parriott A, Hutchinson AB, Shrestha R, et al. Change in condom use in populations newly aware of HIV diagnosis in the United States and Canada: a systematic review and meta-analysis. AIDS Behav. 2021;25(6):1839–55.
Zakher B, Blazina I, Chou R. Association between knowledge of HIV-positive status or use of antiretroviral therapy and high-risk transmission behaviors: systematic review. AIDS Care. 2014;26(4):514–21.
Cochrane Handbook for Systematic Reviews of Interventions, Version 5.1.0. The Cochrane Collaboration https://www.cochrane-handbook.org 2011. accessed 18 Sept 2015.
Malekinejad M, Barker E, Horvath H, Kahn JG, Jimsheleishvili S. The impact of HIV infection diagnosis on sero-adaptive behaviors in men who have sex with men in the United States: protocol for a systematic review and meta-analysis [Protocol]. PROSPERO International Prospective Register of Systematic Reviews; 2018 https://www.crd.york.ac.uk/PROSPERO/display_record.php?RecordID=85282.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ (Clinical research ed). 2009;339: b2535.
GRADE handbook for grading quality of evidence and strength of recommendations. GRADE Working Group http://www.guidelinedevelopment.org/handbook/ 2013. accessed 21 Jan 2018.
EndNote v. X7. Thomson; 2013.
Zhang J, Yu KF. What’s the relative risk? A method of correcting the odds ratio in cohort studies of common outcomes. JAMA. 1998;280(19):1690–1.
Corp S. Stata Statistical Software: Release 14.2. College Station, TX: StataCorp LP.; 2015.
Colfax GN, Buchbinder SP, Cornelisse PGA, Vittinghoff E, Mayer K, Celum C. Sexual risk behaviors and implications for secondary HIV transmission during and after HIV seroconversion. AIDS. 2002;16(11):1529–35.
Darrow WW, Webster RD, Kurtz SP, Buckley AK, Patel KI, Stempel RR. Impact of HIV counseling and testing on HIV-infected men who have sex with men: the south beach health survey. AIDS Behav. 1998;2(2):115–26.
Vallabhaneni S, McConnell JJ, Loeb L, Hartogensis W, Hecht FM, Grant RM, et al. Changes in seroadaptive practices from before to after diagnosis of recent HIV infection among men who have sex with men. PLoS ONE. 2013;8(2):1–8.
Golden MR, Dombrowski JC, Kerani RP, Stekler JD. Failure of serosorting to protect African American men who have sex with men from HIV infection. Sex Transm Dis. 2012;39(9):659–64.
McFarland W, Chen YH, Raymond HF, Nguyen B, Colfax G, Mehrtens J, et al. HIV seroadaptation among individuals, within sexual dyads, and by sexual episodes, men who have sex with men, San Francisco, 2008. AIDS Care. 2011;23(3):261–8.
Khosropour CM, Dombrowksi JC, Hughes JP, Manhart LE, Golden MR. Evaluation of a computer-based recruitment system for enrolling men who have sex with men into an observational HIV behavioral risk study. Am J Epidemiol. 2016;184(6):477–83.
Khosropour CM, Dombrowski JC, Kerani RP, Katz DA, Barbee LA, Golden MR. Changes in condomless sex and serosorting among men who have sex with men after HIV diagnosis. J Acquir Immune Defic Syndr. 2016;73(4):475–81.
Steward WT, Remien RH, Higgins JA, Dubrow R, Pinkerton SD, Sikkema KJ, et al. Behavior change following diagnosis with acute/early HIV infection-a move to serosorting with other HIV-infected individuals. the NIMH multisite acute HIV infection study: III. AIDS Behav. 2009;13(6):1054–60.
Marks G, Millett GA, Bingham T, Bond L, Lauby J, Liau A, et al. Understanding differences in HIV sexual transmission among Latino and Black men who have sex with men: the Brothers y Hermanos Study. AIDS Behav. 2009;13(4):682–90.
Golden MR, Stekler J, Hughes JP, Wood RW. HIV serosorting in men who have sex with men: is it safe. J Acquir Immune Defic Syndr. 2008;49(2):212–8.
Moore DM, Kanters S, Michelow W, Gustafson R, Hogg RS, Kwag M, et al. Implications for HIV prevention programs from a serobehavioural survey of men who have sex with men in Vancouver, British Columbia: the ManCount study. Can J Public Health Revue canadienne de santé publique. 2012;103(2):142–6.
CDC. Adoption of protective behaviors among persons with recent HIV infection and diagnosis–Alabama, New Jersey, and Tennessee, 1997–1998. MMWR Morb Mortal Wkly Rep. 2000;49(23):512–5.
CDC. HIV testing and risk behaviors among gay, bisexual, and other men who have sex with men—United States. MMWR Morb Mortal Wkly Rep. 2013;62(47):958–62.
CDC. HIV Infection Risk, Prevention, and Testing Behaviors among Men Who Have Sex With Men—National HIV Behavioral Surveillance, 20 U.S. Cities, 2014. CDC; 2016.
Drumright LN, Strathdee SA, Little SJ, Araneta MRG, Slymen DJ, Malcarne VL, et al. Unprotected anal intercourse and substance use before and after HIV diagnosis among recently HIV-infected men who have sex with men. Sex Transm Dis. 2007;34(6):401–7.
German D, Sifakis F, Maulsby C, Towe VL, Flynn CP, Latkin CA, et al. Persistently high prevalence and unrecognized HIV infection among men who have sex with men in Baltimore: the Besure study. J Acquir Immune Defic Syndr. 2011;57(1):77–87.
Gorbach PM, Weiss RE, Jeffries R, Javanbakht M, Drumright LN, Daar ES, et al. Behaviors of recently HIV-infected men who have sex with men in the year postdiagnosis: Effects of drug use and partner types. J Acquir Immune Defic Syndr. 2011;56(2):176–82.
Gorbach PM, Javanbakht M, Bolan RK. Behavior change following HIV diagnosis: findings from a Cohort of Los Angeles MSM. AIDS Care. 2017;197:1–5.
McGowan JP, Shah SS, Ganea CE, Blum S, Ernst JA, Irwin KL, et al. Risk behavior for transmission of human immunodeficiency virus (HIV) among HIV-seropositive individuals in an urban setting. Clin Infect Dis. 2004;38(1):122–7.
Saah AJ, Hoover DR, Weng S, Carrington M, Mellors J, Rinaldo CR Jr, et al. Association of HLA profiles with early plasma viral load, CD4+ cell count and rate of progression to AIDS following acute HIV-1 infection. Multicenter AIDS Cohort Study AIDS. 1998;12(16):2107–13.
Valleroy LA, MacKellar DA, Karon JM, Rosen DH, McFarland W, Shehan DA, et al. HIV prevalence and associated risks in young men who have sex with men. Young Men’s Survey Study Group. JAMA. 2000;284(2):198–204.
Whitham HK, Sansom SL, Wejnert C, Finlayson T, Huang YA, An Q, et al. Sex practices by HIV awareness and engagement in the continuum of care among MSM: a national HIV behavioral surveillance analysis in 21 U.S. cities. AIDS Behav. 2018;22(3):840–7.
Acknowledgements
The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the Centers for Disease Control and Prevention.
Funding
This project was funded by the U.S. CDC, National Center for HIV, Viral Hepatitis, STD, and TB Prevention Epidemiologic and Economic Modeling Agreement (NEEMA, # 5U38PS004649).
Author information
Authors and Affiliations
Contributions
MM was the lead author and supervisor. SJ and EKB conducted record/article screening and data extraction. MM adjudicated disagreements in screening decisions and conduced meta-analysis. ABH, RKS, PV, and JGK provided technical guidance throughout the research project. All authors contributed to manuscript development.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
Not required (review).
Consent to Participate
Not required (review).
Consent for Publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Malekinejad, M., Jimsheleishvili, S., Barker, E.K. et al. Sexual Practice Changes Post-HIV Diagnosis Among Men Who Have Sex with Men in the United States: A Systematic Review and Meta-analysis. AIDS Behav 27, 257–278 (2023). https://doi.org/10.1007/s10461-022-03761-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-022-03761-y