Abstract
To examine HIV service interruptions during the COIVD-19 outbreak in South Carolina (SC) and identify geospatial and socioeconomic correlates of such interruptions, we collected qualitative, geospatial, and quantitative data from 27 Ryan White HIV clinics in SC in March, 2020. HIV service interruptions were categorized (none, minimal, partial, and complete interruption) and analyzed for geospatial heterogeneity. Nearly 56% of the HIV clinics were partially interrupted and 26% were completely closed. Geospatial heterogeneity of service interruption existed but did not exactly overlap with the geospatial pattern of COVID-19 outbreak. The percentage of uninsured in the service catchment areas was significantly correlated with HIV service interruption (F = 3.987, P = .02). This mixed-method study demonstrated the disparity of HIV service interruptions in the COVID-19 in SC and suggested a contribution of existing socioeconomic gaps to this disparity. These findings may inform the resources allocation and future strategies to respond to public health emergencies.
Similar content being viewed by others
Introduction
The outbreak of coronavirus disease 2019 (COVID-19), caused by the severe acute respiratory syndrome coronavirus (SARS-CoV-2), is a rapidly evolving global public health crisis [1]. On March 11, 2020, the World Health Organization characterized COVID-19 as a pandemic [2]. As of August 5, 2020, infection cases exceeded 18,614,177 across 216 countries and areas, with over 702,642 deaths [3]. These numbers continue to rise daily as the virus continues to spread globally.
People living with HIV (PLWH) have been recognized as a medically and socially vulnerable population during the COVID-19 pandemic [4]. HIV-related services have been unavoidably interrupted and impacted. On March 18, 2020, the CDC posted specific guideline to address PLWH’s concerns and questions related to their COVID-19 risk and prevention. On March 20, 2020, the NIH Office of AIDS Research also provided interim guideline related to COVID-19 and PLWH. However, there have been many challenges in the implementation of these guidelines, particularly in the areas of healthcare delivery and PLWH’s linkage to care and retention in care [5, 6].
During the unprecedented COVID-19 outbreak, many health facilities providing HIV prevention, treatment and care services had to change their schedules and operation modalities to adapt to the challenges imposed by COVID-19 and its prevention and control measures (social distancing, travel restrictions, stay at home orders, etc.). Routine, non-urgent or elective health care visits and procedures were cancelled or delayed. Supportive services such as face-to-face counselling, housing services and outreach services were temporarily suspended. In addition, patients avoided accessing health care, even for urgent concerns, due to fear of COVID-19 exposure [7, 8]. In order to improve healthcare delivery and provide sustainable quality care to PLWH during the COVID-19 pandemic and future pandemics, we need a better understanding of the nature and scope of HIV treatment service interruption and their correlates.
Existing literature suggests a health disparity in COVID-19 prevalence and related clinical outcomes (e.g., complications, mortality) in the United States. For example, one recent spatial analysis on COVID-19 epidemic reported an uneven impact on incidence and mortality of COVID-19 in the United States [9]. The study showed positive correlations of COVID‐19 incidence and mortality rates with socioeconomic factors [9]. However, no empirical studies have examined if there is a spatial disparity in the HIV service interruption and if existing social determinants of health influence the pattern of HIV service interruption, particularly in Southern States such as South Carolina.
South Carolina (SC) has been heavily hit by the COVID-19. The first case of COVID-19 was reported in SC on March 6, 2020 [10]. On April 2, 2020, SC Department of Health and Environmental Control (DHEC) announced that the virus had spread to all 46 counties in the state [11]. As of August 5, 2020, COVID-19 cases exceeded 94,831 with over 1819 deaths in SC [10].
Therefore, using mixed-method data, the current study aims to (1) examine the interruption of HIV service delivery in SC during COVID-19 outbreak; (2) demonstrate the pattern of this service interruption by geolocation; and (3) identify any existing health disparity factors (e.g., socioeconomic status) that were associated with the HIV service interruption.
Methods
Study Setting
SC is one of the seven states targeted by the “Ending the HIV Epidemic (EtHE): A Plan for America” [12] campaign due to its high rural HIV burden [12]. With an HIV infection rate of 15.8 per 100,000 people, SC ranked 11th among all 50 states in 2018, with an estimate of 20,166 PLWH [13]. African Americans and men who have sex with men (MSM) are disproportionately affected by HIV/AIDS in SC [13]. By 2018, there were 27 clinics in SC funded by Ryan White HIV/AIDS Program [14]. The Ryan White HIV/AIDS Programs are federally funded programs to provide comprehensive HIV primary medical care, essential support services, and medications for low-income PLWH who are uninsured and underserved [15]. According to the program profile, it was estimated that 11,369 (56%) PLWH were served by the Ryan White clinics in SC in 2018 [16].
Data Collection
Qualitative information was extracted from the program process reports of 27 Ryan White HIV clinics (grantees of Ryan White HIV/AIDS programs) across 46 counties in SC in March, 2020. These reports were submitted to the SC DHEC based on the clinics’ status of operation and HIV-related service delivery during the COVID-19 outbreak.
Geolocations and zip codes of the HIV clinics were retrieved for geospatial analysis. Based on the information provided by the HIV clinics, we identified the service catchment areas of the clinics (i.e., counties these HIV clinics served). We then extracted data from various sources for each county’s relevant characteristics, such as number of PLWH per 100,000 in 2018 (via AIDSVu, https://aidsvu.org), number of COVID-19 cases per 100,000 as of June 13, 2020 (via SC DHEC, https://scdhec.gov), and socioeconomic status (SES) indicators in 2016 (via US Census Bureau, https://census.gov/). The SES indicators included poverty (percent of population living below federal poverty line) [17], high school education (percent of population with a high school degree or equivalent) [18], median household income [17], Gini Coefficient (a measure of income inequality with 0 reflecting complete equality and 1 reflecting complete inequality) [19], and percent of population without health insurance [20]. The current study was approved by the Institutional Research Board at University of South Carolina.
Categorization of Service Interruption
Based on qualitative data regarding the status of operation at HIV clinics, a medical expert with over 20 years experiences in both HIV-related research and clinic care initially categorized HIV service interruption during the COVID-19 outbreak into four types: complete interruption, partial interruption, minimal interruption, and no interruption. Specifically, there were four criteria for assessing the HIV service interruption including clinic operation hours (e.g., whether clinics are open for most of weekdays), HIV service coverage (e.g., whether clinics maintain most of existing services), telehealth use (e.g., whether clinics use telehealth in service delivery), and healthcare providers’ availability (e.g., whether most of healthcare providers, especially medical case managers can still work in their original capacity). The clinics that failed in meeting the four criteria were considered as “complete interruption”, failed in any two or three as “partial interruption”, failed in any one of the criteria as “minimal interruption”, and those met all the four criteria as “no interruption”. Another team member reviewed the data and confirmed the initial categorization using the same criteria.
Data Analysis
We analyzed the qualitative data based on grounded theory [21]. Five themes occurred regarding HIV service interruption, including operation days and time, protection measures, service coverage, the use of telehealth and mobile applications (apps), and healthcare provider availability.
We then mapped the pattern of HIV service interruptions using the Geographic Information System (GIS) to indicate geospatial distribution.
For quantitative data, we developed the county-level indicators (e.g., SES, COVID-19 cases, and HIV cases) for each HIV clinic based on its service catchment area. Specifically, each of the five SES indicators, number of COVID-19 cases per 100,000 people, and number of PLWH per 100,000 people were averaged among counties that each clinic served. It should be noted that there may be overlap among some clinics in catchment area with some counties being served by more than one clinic. In such cases, indicators of those counties were used by each serving clinic. ANOVA was used to examine the associations between these county-level indicators and types of service interruption. One HIV clinic that provided state-wide HIV service was removed from the county-level geospatial analysis and quantitative analysis since its service catchment area was not limited to any specific county.
Results
HIV Service Interruption in SC
Among the 27 HIV clinics in the current study, two clinics (7.4%) were assessed as “no interruption”, three (11.1%) as “minimal interruption”, 15 clinics (55.6%) as “partial interruption”, and seven clinics (25.9%) as “complete interruption”. The qualitative information regarding HIV service interruption during the outbreak of COVID-19 covered five domains (See sample quotes in Table 1). In terms of operation time, only one clinic had their main site open for normal hours. Most of HIV clinics reduced their office hours, limited office visits, and/or limited face-to-face appointments. Seven clinics were closed with only staff checking emails daily. Clinics adapted various strategies in adjusting operation hours. Some canceled evening hours. Some adjusted their schedule, providing different types of services at different dates and hours.
All the clinics adapted specific measures to protect patients, visitors, healthcare providers, and staff from COVID-19 infection. Common strategies included requiring temperature and symptom screening for all visitors entering into the building, asking all the people in the offices and building to wear face masks, and taking precaution to maintain social distancing in offices. One clinic mentioned that they provided COVID-19 testing at their sites. One clinic highlighted that their patients were screened and triaged prior to entering into clinic. Another clinic reported that they had sufficient stock to provide masks to both clinic staff and visiting patients.
Due to the closure and reduced operation hours, HIV-related services were interrupted at many clinics in terms of scope and delivery modality. Two HIV clinics reported that they had to discontinue home visits and support groups. Several clinics suspended walk-in services. One clinic mentioned that their dental offices were only seeing patients for emergency visits. Prevention services were available by appointment only and HIV testing services were provided at alternative sites. However, most of clinics still accepted new referrals for HIV treatment and primary care, and they also delivered medical care, case management services, pharmacy services and lab services over telephone and/or in the offices when needed. One clinic reported that they also provided curbside/drive through COVID-19 testing on-site and partnering with SC DHEC to do COVID-19 testing in the community. Two clinics also assisted patients with medication pick-up/delivery, food cards, personal pantry and housing services/support as needed.
Telehealth and mobile apps were widely used in HIV clinics for making appointments and delivering HIV prevention, treatment, and care services. One clinic also introduced an on-line request system for rent, food, and clothing assistance. For the clinics where regular operation hours remained unchanged, telehealth was also provided as an option for patients. One clinic reported, “We have virtual visit capabilities for all patients with regular follow-up appointments if patients have computer and internet access at home. For Ryan White patients, medical case managers (MCMs) will bring laptop and hot spot to the patient's home, get them online with provider and step out of the room”.
During the COVID-19 outbreak, most healthcare providers and staff had flexible working schedules. Policy regarding remote working and return-to-work varied across clinics and also changed along with the rapidly evolving pandemic. Most of clinics reported that the providers and staff were working from home using Virtual Private Network (VPN) for access to Provide Enterprise (Ryan White data reporting system). In some clinics, MCMs were rotating “in office” at least 2 days a week, providing services by appointment only. One clinic reported that their MCMs reached out to clients who had not picked up medicines and offered medication delivery. Since June 2020, more providers and staff have returned to the office. One clinic staff said, “Decisions going forward will be made daily/weekly as to our re-opening with full staffing.”
Geospatial Patterns of HIV Service Interruption
The county-level geospatial pattern of the HIV service interruption among all HIV clinics (except the one that provided state-wide service), along with the geospatial pattern of COVID-19 cases in SC is shown in Fig. 1. Generally, most of the service catchment areas were moderately affected by the COVID-19 outbreak in terms of confirmed COVID-19 cases per capita. In the Upstate area no clinic reported “complete interruption” of HIV services. Geospatial heterogeneity in terms of HIV service interruption existed. However, the geospatial pattern of HIV service interruption did not exactly overlap with the density of COVID-19 cases at county level.
Association Between Interruption and Health Disparity Factors
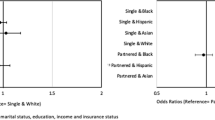
The results of descriptive analysis and ANOVA analysis are shown in Table 2. Among the service catchment areas of the HIV clinics, the mean rate of PLWH in 2018 and the mean rate of confirmed COVID-19 cases as of June 13, 2020 was 429 and 416 per 100,000, respectively. The median household income averaged $43,124 (SD = 5367). The mean of Gini coefficients was .46. The percentage of uninsured population was 13.5% on average (statewide: 10.5%) [13]. Among these counties, the percentage of people in the county living in poverty was approximately 20% (statewide: 15.3%) [13]. On average, about 83% of population had graduated from high school. ANOVA analysis did not detect significant difference by HIV service interruption types in terms of SES indicators except the percentage of uninsured population.
The geospatial distribution pattern of PLWH was similar to the distribution pattern of confirmed COVID-19 cases. HIV service interruption pattern did not consistently correspond with the density of COVID-19 cases. While the clinics that reported no interruption in services were in areas with the lowest rate of COVID-19 cases, some clinics that reported minimal interruptions were in areas with the highest rate of COVID-19 cases. The percentage of uninsured population was significantly different by HIV service interruption type (F = 3.987, P = .02), indicating a potential correlation between health insurance coverage and the HIV service interruption. Post-hoc pairwise comparison (data not shown) suggested that the service catchment areas with no interruption in services had a lower percentage of uninsured than those areas with minimal service interruption, partial service interruption, and complete service interruption, although not all of these differences reached statistical significance.
Discussion
Using mixed-method data collected from 27 HIV clinics in SC, the current study examined HIV service interruptions in SC during the COVID-19 outbreak. We demonstrated geospatial pattern of the HIV service interruption, and explored the potential socioeconomic correlates with the service interruption. Of our sample, nearly 82% of the HIV clinics were either partially interrupted (56%) or completely closed (26%) during the COVID-19 outbreak. The COVID-19 disrupted regular operation routine, reduced office hours, and decreased the availability of healthcare providers and staff in HIV clinics. Although most of the clinics still provided core HIV services (e.g., medicine refilling, HIV testing), they had to suspend or cancel face-to-face counseling and social support group. Geospatial heterogeneity in terms of HIV service interruption existed. However, the geospatial pattern of HIV service interruption did not exactly overlap with the density of confirmed COVID-19 cases in the service catchment area. The areas with a higher insurance coverage (i.e., a lower percentage of uninsured population) tended to show less HIV service interruption.
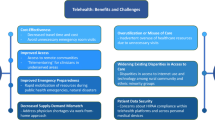
Telehealth and mobile applications played an important role in retaining HIV services and delivering other supportive services during the COVID-19 outbreak. Our findings provide further empirical evidence for the value and need of telehealth as a convenient and inexpensive care option during disasters and public health crisis [22,23,24]. However, our qualitative study suggested that not all HIV clinics were able to make a timely shift to a telehealth system. Four of the HIV clinics did not have capacity to support virtual visit for patients. In addition, many patients who did not have computer or internet access at home might not be able to benefit from telehealth, leading to a widening disparity in care. Further implementation science studies are needed to explore the facilitators and barriers for scaling-up telehealth in responding to COVID-19 pandemic and other public health emergencies.
The geospatial distribution of PLWH largely overlapped with the geospatial distribution of confirmed COVID-19 cases through June 2020. This result suggests the importance to integrate the efforts of responding dual epidemics of HIV and COVID-19. Some HIV clinics reported that they provided COVID-19 testing for their communities in partnership with SC DHEC. These practices are consistent with the recent recommendation in the literature to take advantage of COVID-19 contact tracing as a great opportunity for a more coverage of HIV testing [25]. Future studies on needs assessment and infrastructure evaluation are warranted to explore the feasibility and acceptability of providing integrated COVID-19 and HIV testing and services for local communities based on existing HIV testing program or infrastructures available at HIV clinics.
Our findings suggested a big variation across SC in extent of HIV service interruption with a range from no interruption to complete interruption of services. Most of HIV clinics had adapted flexible strategies to deal with the crisis caused by COVID-19, but they still showed difference in operational hours, healthcare provider availability, and scope of HIV services during the outbreak. This gap in responding to the public health crisis could not be fully explained by the COVID-19 itself. Existing socioeconomic disparities at county level might contribute to the gap in health service delivering. For example, the percentage of uninsured population in service catchment area was related to the service interruption of HIV clinics. We may need to further examine the characteristics of HIV clinics in terms of their financial situation, human resources, and infrastructure of telehealth to explore if and how existing variation in health infrastructure is associated with disparity of HIV service interruption.
The disparity of HIV service interruption during a public health crisis such as COVID-19 is an important issue for the healthcare systems and policy makers to consider as such interruption may further amplify the disparities in HIV treatment cascade in settings with a significant HIV burden or among various vulnerable populations. In the global context, there might be 500,000 additional deaths due to a 6-month interruption of ART in Africa [26]. In the United States, a Boston health center reported that disruptions in Pre-Exposure Prophylaxis (PrEP) care were more prominent among vulnerable population [27]. In Maryland, a comprehensive patient and family centered HIV primary care was interrupted among racial, sexual and gender minority youth living with HIV, which might impede their medicine adherence and clinical improvement [28]. To prevent the further widening of the disparities in existing HIV care system, strengthening and empowering community partners of HIV clinics could be essential for more effective and accountable responses to public health emergencies [29,30,31].
The current study is subject to several limitations. First, qualitative data was collected within 2 months and reports of the HIV clinics were obtained in different dates. Giving the rapidly evolving COVID-19 pandemic, the information we collected might lag behind the changes made by the clinics in response to the pandemic. Second, we were not able to quantify the HIV service interruption based on existing qualitative information. Although we have identified five domains to assess service interruptions, lack of complete and systematic assessment prevented us from developing a numeric index to measure HIV service interruption. The categorization of HIV clinics by a medical expert and other team member might introduce subjective bias. Third, we only included the Ryan White HIV clinics in the analysis because of the availability of program reports. Given the large state-wide coverage of Ryan White programs in providing HIV service, the findings may serve as a good presentation of the HIV service interruption issues in SC. Fourth, the service catchment areas of the HIV clinics were not mutually exclusive. Thus, one county might be included in the calculation of factor variables for more than one HIV clinics. However, since the analysis was based on clinic level, we do not believe that the inclusion of same county level data for different clinics would pose a serious threat to the internal validity of the clinic-level analysis. Finally, the small sample size of the quantitative study limited the power to detect statistically significant correlates.
Despite these limitations, the current study is one of the first efforts to examine the disparity of HIV service interruption and identified the socioeconomic correlates of this disparity. Our findings show that the COVID-19 pandemic added additional burdens to HIV care system in SC. A rapid shift to telehealth system and integration of HIV and COVID-19 care might be effective strategies to respond to this public health crisis. However, existing socioeconomic disparity might contribute to the gap in HIV service interruption, leaving PLWH in low SES communities more vulnerable. We call for more attentions to this disparity in HIV service delivery in both clinics’ capacity building and the federal or state support to HIV service programs in fighting the COVID-19 pandemic.
References
World Health Organization. Coronavirus disease (COVID-19) Pandemic 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019.
World Health Organization. WHO Director-General’s opening remarks at the media briefing on COVID-19—11 March 2020. 2020. March 22.
World Health Organization. Coronavirus disease (COVID-19) Situation Dashboard. 2020. June 21.
Centers for Disease Control and Prevention. People of any age with underlying medical conditions 2020 [updated June 25, 2020]. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fcoronavirus%2F2019-ncov%2Fneed-extra-precautions%2Fgroups-at-higher-risk.html.
Centers for Disease Control and Prevention. COVID-19: What people with HIV should know 2020. https://www.cdc.gov/coronavirus/2019-ncov/specific-groups/hiv.html.
National Institute of Health. Interim Guidance for COVID-19 and Persons with HIV 2020. https://aidsinfo.nih.gov/guidelines/html/8/covid-19-and-persons-with-hiv--interim-guidance-/0.
Beima-Sofie K, Ortblad KF, Swanson F, Graham SM, Stekler JD, Simoni JM. “Keep It Going if You Can”: HIV Service Provision for priority populations during the COVID-19 pandemic in Seattle, WA. AIDS Behav. 2020. https://doi.org/10.1007/s10461-020-02902-5.
Ridgway JP, Schmitt J, Friedman E, Taylor M, Devlin S, McNulty M, et al. HIV care continuum and COVID-19 outcomes among people living with HIV during the COVID-19 pandemic, Chicago, IL. AIDS Behav. 2020. https://doi.org/10.1007/s10461-020-02905-2.
Zhang CH, Schwartz GG. Spatial disparities in coronavirus incidence and mortality in the United States: an ecological analysis as of May 2020. J Rural Health. 2020;36:433–45.
South Carolina Department of Health and Environment Control. SC testing data & projections (COVID-19). 2020.
GoLaurens.com. COVID-19 reported in all 46 counties across SC, 4 cases in Laurens County. April 2, 2020. https://www.newsbreak.com/south-carolina/columbia/news/0OdiqYtQ/covid-19-reported-in-all-46-counties-across-sc-4-cases-in-laurens-county.
US Department of Health Human Services. Ending the HIV epidemic: a plan for America. 2019.
South Carolina Department of Health and Environment Control. An epidemiologic profile of HIV and AIDS in South Carolina 2019. https://www.scdhec.gov/sites/default/files/media/document/2019-Epi-Profile.pdf.
South Carolina Department of Health and Environment Control. SC HIV Service Providers: Ryan White 2018. Part B. https://scdhec.gov/sites/default/files/media/document/STD%20HIV%20Part%20B%20Service%20Providers%2011092018.pdf. Part C. https://www.scdhec.gov/sites/default/files/docs/Health/docs/stdhiv/STD%20HIV%20Part%20C%20Service%20Providers.pdf.
Health Resources and Services Administration. About Ryan White HIV/AIDS Program 2019 [updated February 2019]. https://hab.hrsa.gov/about-ryan-white-hivaids-program/about-ryan-white-hivaids-program.
Health Resources and Services Adminstration. What are the demographic characteristics of Ryan White HIV/AIDS Program clients in South Carolina? 2018. https://hab.hrsa.gov/stateprofiles2018/#/profile.
United States Census Bureau. Small area income and poverty estimates. Table 1: 2916 poverty adn median income estimates: counties. 2016.
United States Census Bureau. American community survey 5-year estimates, 2016. Table DP02: educational attainment for the population 25 years and over: counties. 2016.
United States Census Bureau. American community survey 5-year estimates, 2016. Table B19083: Gini Index of income inequality. 2016.
United States Census Bureau. Small area health insurance estimates, 2016: Health insurance coverage status by age, race, hispanic origin, sex and income for counties and states. 2016.
Strauss A, Corbin J. Grounded theory methodology. Handb Qual Res. 1994;17(1):273–85.
Duffy S, Lee TH. In-person health care as option B. N Engl J Med. 2018;378(2):104–6.
Hollander JE, Carr BG. Virtually perfect? Telemedicine for COVID-19. N Engl J Med. 2020;382(18):1679–81.
Lurie N, Carr BG. The role of telehealth in the medical response to disasters. JAMA Intern Med. 2018;178(6):745–6.
Nosyk B, Armstrong WS, Del Rio C. Contact tracing for COVID-19: an opportunity to reduce health disparities and end the HIV/AIDS Epidemic in the US. Clin Infect Dis. 2020. https://doi.org/10.1093/cid/ciaa501.
Hogan AB, Jewell B, Sherrard-Smith E, Vesga J, Watson OJ, Whittaker C, et al. The potential impact of the COVID-19 epidemic on HIV, TB and Malaria in low-and middle-income countries. Imp Coll Lond (01-05-2020). 2020. https://doi.org/10.25561/78670.
Adadi P, Kanwugu ON. Living with HIV in the time of COVID-19: a glimpse of hope. J Med Virol. 2020. https://doi.org/10.1002/jmv.26118.
Armbruster M, Fields EL, Campbell N, Griffith DC, Kouoh AM, Knott-Grasso MA, et al. Addressing health inequities exacerbated by COVID-19 among youth with HIV: expanding our toolkit. J Adolesc Health. 2020. https://doi.org/10.1016/j.jadohealth.2020.05.021.
Pinto RM, Park S. COVID-19 Pandemic disrupts HIV continuum of care and prevention: implications for research and practice concerning community-based organizations and frontline providers. AIDS Behav. 2020;24:2486–9.
Operario D, King EJ, Gamarel KE. Prioritizing community partners and community HIV workers in the COVID-19 pandemic. AIDS Behav. 2020. https://doi.org/10.1007/s10461-020-02896-0.
International AIDS Society. The COVID-19 and HIV: a tale of two pandemics. 2020. https://covid19andhivreport.iasociety.org/.
Acknowledgements
Research reported in this publication was supported by the National Institute of Allergy and Infectious Diseases of the National Institutes of Health under Award Number R01AI127203-4S1 and the University of South Carolina Office of Vice President for Research COVID-19 grant (USCIP 80003673). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health and University of South Carolina.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Qiao, S., Li, Z., Weissman, S. et al. Disparity in HIV Service Interruption in the Outbreak of COVID-19 in South Carolina. AIDS Behav 25, 49–57 (2021). https://doi.org/10.1007/s10461-020-03013-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-020-03013-x