Abstract
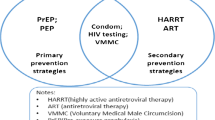
To understand the sexual risk behavior of men with traditional male circumcision and medical male circumcision in the context of the World Health Organization’s (WHO) campaign for voluntary medical male circumcision (VMMC) scale-up, we investigated ten countries prioritized for the scale-up from the Demographic and Health Surveys. Male respondents aged 15–49 were selected. Ordinal regression was used to analyze the relationship between three sexual risk behaviors—condom use with non-cohabiting partners, number of non-cohabiting partners, and partner type—and circumcision status (traditionally circumcised before and after the VMMC scale-up, medically circumcised before and after the scale-up, and not circumcised), while controlling for social demographic covariates. We found evidence that some sexual risky behavior, specifically lower condom use and higher number of sexual partners, was associated with traditional circumcision. This finding suggests that messages about the protective effect of male circumcision may not have reached men with traditional circumcision. We suggest that WHO’s VMMC campaign should include communities where traditional male circumcision is popular. We looked for, but did not find, evidence of differences between groups circumcised at different times, which could have indicated sexual risk compensation.




Similar content being viewed by others
References
Joint United Nations Programme on HIV/AIDS.: Get on the Fast Track. The life-cycle approach to HIV: finding solutions for everyone at every stage of life. Geneva: UNAIDS; 2016.
Schwartlander B, Stover J, Hallett T, Atun R, Avila C, Gouws E, Bartos M, Ghys PD, Opuni M, Barr D, Alsallaq R, Bollinger L, de Freitas M, Garnett G, Holmes C, Legins K, Pillay Y, Stanciole AE, McClure C, Hirnschall G, Laga M, Padian N. Towards an improved investment approach for an effective response to HIV/AIDS. Lancet. 2011;377:2031–41.
World Health Organization. Progress in scale-up of male circumcision for HIV prevention in eastern and southern Africa: focus on service delivery. Geneva: World Health Organization; 2011.
Szabo R, Short RV. How does male circumcision protect against HIV infection? BMJ. 2000;320:1592–4.
World Health Organization. New data on male circumcision and HIV Prevention: policy and programme implications. Geneva: World Health Organization; 2007.
Andersson N, Cockcroft A. Male circumcision, attitudes to HIV prevention and HIV status: a cross-sectional study in Botswana, Namibia and Swaziland. AIDS Care. 2012;24:301–9.
Cassell MM, Halperin DT, Shelton JD, Stanton D. Risk compensation: the Achilles’ heel of innovations in HIV prevention? BMJ. 2006;332:605–7.
Dushoff J, Patocs A, Shi CF. Modeling the population-level effects of male circumcision as an HIV-preventive measure: a gendered perspective. PLoS ONE. 2011;6:28608.
Riess TH, Achieng’ MM, Otieno S, Ndinya-Achola JO, Bailey RC. “When I was circumcised I was taught certain things”: risk compensation and protective sexual behavior among circumcised men in Kisumu, Kenya. PLoS ONE. 2010;5:12366.
Bailey RC, Egesah O, Rosenberg S. Male circumcision for HIV prevention: a prospective study of complications in clinical and traditional settings in Bungoma, Kenya. Bull World Health Organ. 2008;86:669–77.
Maffioli EM. Is traditional male circumcision effective as an HIV prevention strategy? Evidence from Lesotho. PLoS ONE. 2017;12:0177076.
Peltzer K, Nqeketo A, Petros G, Kanta X. Traditional circumcision during manhood initiation rituals in the Eastern Cape, South Africa: a pre-post intervention evaluation. BMC Public Health. 2008;8:64.
Thomas AG, Tran BR, Cranston M, Brown MC, Kumar R, Tlelai M. Voluntary medical male circumcision: a cross-sectional study comparing circumcision self-report and physical examination findings in Lesotho. PLoS ONE. 2011;6:27561.
Wilcken A, Keil T, Dick B. Traditional male circumcision in eastern and southern Africa: a systematic review of prevalence and complications. Bull World Health Organ. 2010;88:907–14.
Katisi M, Daniel M. Safe male circumcision in Botswana: tension between traditional practices and biomedical marketing. Glob Public Health. 2015;10:739–56.
Lau FK, Jayakumar S, Sgaier SK. Understanding the socio-economic and sexual behavioural correlates of male circumcision across eleven voluntary medical male circumcision priority countries in southeastern Africa. BMC Public Health. 2015;15:813.
Eaton LA, Cain DN, Agrawal A, Jooste S, Udemans N, Kalichman SC. The influence of male circumcision for HIV prevention on sexual behaviour among traditionally circumcised men in Cape Town, South Africa. Int J STD AIDS. 2011;22:674–9.
Nyembezi A, Ruiter RAC, van den Borne B, Sifunda S, Funani I, Reddy P. Correlates of consistent condom use among recently initiated and traditionally circumcised men in the rural areas of the Eastern Cape Province, South Africa. BMC Public Health. 2014;14:668.
Zungu NP, Simbayi LC, Mabaso M, Evans M, Zuma K, Ncitakalo N, Sifunda S. HIV risk perception and behavior among medically and traditionally circumcised males in South Africa. BMC Public Health. 2016;16:357.
Padian NS, Buve A, Balkus J, Serwadda D, Cates WJ. Biomedical interventions to prevent HIV infection: evidence, challenges, and way forward. Lancet. 2008;372:585–99.
UNAIDS/WHO/SACEMA Expert Group on Modelling the Impact and Cost of Male Circumcision for HIV Prevention. Male circumcision for HIV prevention in high HIV prevalence settings: what can mathematical modelling contribute to informed decision making? PLoS Med. 2009;6:1000109.
Awad SF, Sgaier SK, Lau FK, Mohamoud YA, Tambatamba BC, Kripke KE, Thomas AG, Bock N, Reed JB, Njeuhmeli E, Abu-Raddad LJ. Could circumcision of HIV-positive males benefit voluntary medical male circumcision programs in Africa? Mathematical modeling analysis. PLoS ONE. 2017;12:0170641.
Wawer MJ, Makumbi F, Kigozi G, Serwadda D, Watya S, Nalugoda F, Buwembo D, Ssempijja V, Kiwanuka N, Moulton LH, Sewankambo NK, Reynolds SJ, Quinn TC, Opendi P, Iga B, Ridzon R, Laeyendecker O, Gray RH. Circumcision in HIV-infected men and its effect on HIV transmission to female partners in Rakai, Uganda: a randomised controlled trial. Lancet. 2009;374:229–37.
Kalichman S, Mathews C, Kalichman M, Eaton LA, Nkoko K. Male circumcision for HIV prevention: awareness, risk compensation, and risk perceptions among South African women. Glob Public Health. 2018;13:1682–90.
Westercamp M, Agot KE, Ndinya-Achola J, Bailey RC. Circumcision preference among women and uncircumcised men prior to scale-up of male circumcision for HIV prevention in Kisumu, Kenya. AIDS Care. 2012;24:157–66.
Kalichman SC, Eaton L, Pinkerton SD. Male circumcision in HIV prevention. Lancet. 2007;369:1597–15989.
Weiss HA, Hankins CA, Dickson K. Male circumcision and risk of HIV infection in women: a systematic review and meta-analysis. Lancet Infect Dis. 2009;9:669–77.
Shi CF, Li M, Dushoff J. Evidence that promotion of male circumcision did not lead to sexual risk compensation in prioritized Sub-Saharan countries. PLoS ONE. 2017;12:0175928.
ICF International. Demographic and health survey sampling and household listing manual. Calverton: ICF International, MEASURE DHS; 2012.
World Health Organization. Progress in scaling up voluntary medical male circumcision for HIV prevention in east and southern Africa, January–December 2011. Geneva: World Health Organization; 2011.
Gray RH, Kigozi G, Serwadda D, Makumbi F, Watya S, Nalugoda F, Kiwanuka N, Moulton LH, Chaudhary MA, Chen MZ, Sewankambo NK, Wabwire-Mangen F, Bacon MC, Williams CFM, Opendi P, Reynolds SJ, Laeyendecker O, Quinn TC, Wawer MJ. Male circumcision for HIV prevention in men in Rakai, Uganda: a randomised trial. Lancet. 2007;369:657–66.
Kibira SPS, Nansubuga E, Tumwesigye NM, Atuyambe LM, Makumbi F. Differences in risky sexual behaviors and HIV prevalence of circumcised and uncircumcised men in Uganda: evidence from a 2011 cross-sectional national survey. Reprod Health. 2014;11:25.
Kong X, Kigozi G, Nalugoda F, Musoke R, Kagaayi J, Latkin C, Ssekubugu R, Lutalo T, Nantume B, Boaz I, Wawer M, Serwadda D, Gray R. Assessment of changes in risk behaviors during 3 years of posttrial follow-up of male circumcision trial participants uncircumcised at trial closure in Rakai, Uganda. Am J Epidemiol. 2012;176:875–85.
Baral S, Beyrer C, Muessig K, Poteat T, Wirtz AL, Decker MR, Sherman SG, Kerrigan D. Burden of HIV among female sex workers in low-income and middle-income countries: a systematic review and meta-analysis. Lancet Infect Dis. 2012;12:538–49.
Chen L, Jha P, Stirling B, Sgaier SK, Daid T, Kaul R, Nagelkerke N. Sexual risk factors for HIV infection in early and advanced HIV epidemics in sub-Saharan Africa: systematic overview of 68 epidemiological studies. PLoS ONE. 2007;2:1001.
Solon G, Haider SJ, Wooldridge J. What are we weighting for? https://www.nber.org/papers/w18859.pdf. Accessed 5 November 2018; 2013.
Christensen RHB. ordinal—regression models for ordinal data. R package version 28, 2015–06; 2015.
Carrasco MA, Nguyen TQ, Kaufman MR. Low uptake of voluntary medical male circumcision among high risk men in Malawi. AIDS Behav. 2018;22(2):447–53.
Kaufman MR, Dam KH, Sharma K, Van Lith LM, Hatzold K, Marcell AV, Mavhu W, Kahabuka C, Mahlasela L, Patel EU, Njeuhmeli E, Seifert Ahanda K, Ncube G, Lija G, Bonnecwe C, Tobian AAR. Females’ peer influence and support for adolescent males receiving voluntary medical male circumcision services. Clin Infect Dis. 2018;66:183–8.
Bulled N, Green EC. Making voluntary medical male circumcision a viable HIV prevention strategy in high prevalence countries by engaging the traditional sector. Crit Public Health. 2016;26:258–68.
Maughan-Brown B, Venkataramani AS, Nattrass N, Seekings J, Whiteside AW. A cut above the rest: traditional male circumcision and HIV risk among Xhosa men in Cape Town, South Africa. J Acquir Immune Defic Syndr. 2011;58:499–505.
Mark D, Middelkoop K, Black S, Roux S, Fleurs L, Wood R, Bekker LG. Low acceptability of medical male circumcision as an HIV/AIDS prevention intervention within a South African community that practises traditional circumcision. S Afr Med J. 2012;102:571–3.
Mshana G, Wambura M, Mwanga J, Mosha J, Mosha F, Changalucha J. Traditional male circumcision practices among the Kurya of north-eastern Tanzania and implications for national programmes. AIDS Care. 2011;23:1111–6.
Wambura M, Mwanga JR, Mosha JF, Mshana G, Mosha F, Changalucha J. Acceptability of medical male circumcision in the traditionally circumcising communities in northern Tanzania. BMC Public Health. 2011;11:373.
Katisi M, Daniel M. Exploring the roots of antagony in the safe male circumcision partnership in Botswana. PLoS ONE. 2018;13:0200803.
Parkhurst JO, Chilongozi D, Hutchinson E. Doubt, defiance, and identity: understanding resistance to male circumcision for HIV prevention in Malawi. Soc Sci Med. 2015;135:15–22.
Sabet Sarvestani A, Bufumbo L, Geiger JD, Sienko KH. Traditional male circumcision in Uganda: a qualitative focus group discussion analysis. PLoS ONE. 2012;7:45316.
Lane C, Bailey RC, Luo C, Parks N. Adolescent male circumcision for HIV prevention in high priority countries: opportunities for improvement. Clin Infect Dis. 2018;66:161–5.
Kaufman MR, Patel EU, Dam KH, Packman ZR, Van Lith LM, Hatzold K, Marcell AV, Mavhu W, Kahabuka C, Mahlasela L, Njeuhmeli E, Seifert Ahanda K, Ncube G, Lija G, Bonnecwe C, Tobian AAR. Counseling received by adolescents undergoing voluntary medical male circumcision: moving toward age-equitable comprehensive human immunodeficiency virus prevention measures. Clin Infect Dis. 2018;66:213–20.
Kaufman MR, Patel EU, Dam KH, Packman ZR, Van Lith LM, Hatzold K, Marcell AV, Mavhu W, Kahabuka C, Mahlasela L, Njeuhmeli E, Seifert Ahanda K, Ncube G, Lija G, Bonnecwe C, Tobian AAR. Impact of counseling received by adolescents undergoing voluntary medical male circumcision on knowledge and sexual intentions. Clin Infect Dis. 2018;66:221–8.
Bain LE, Nkoke C, Noubiap JJN. UNAIDS 90–90–90 targets to end the AIDS epidemic by 2020 are not realistic: comment on “Can the UNAIDS 90–90-90 target be achieved? A systematic analysis of national HIV treatment cascades”. BMJ Glob Health. 2017;2:000227.
U.S. President’s Emergency Plan For AIDS Relief (PEPFAR) VMMC Technical Working Group, Health Communication Capacity Collaborative, ed.: Voluntary medical male circumcision in-service communication best practices guide. https://tinyurl.com/vmmc-pepfar. Accessed 6 March 2019;2017.
Tobian AAR, Dam KH, Van Lith LM, Hatzold K, Marcell AV, Mavhu W, Kahabuka C, Mahlasela L, Patel EU, Njeuhmeli E, Seifert Ahanda K, Ncube G, Lija G, Bonnecwe C, Kaufman MR. Providers’ perceptions and training needs for counseling adolescents undergoing voluntary medical male circumcision. Clin Infect Dis. 2018;66:198–204.
Siegfried N, Muller M, Deeks JJ, Volmink J. Male circumcision for prevention of heterosexual acquisition of HIV in men. Cochrane Database Syst Rev. 2009;2:CD003362.
Acknowledgements
The authors thank Ben Bolker for valuable assistance in statistical analyses.
Funding
CS was funded by a grant from the John S. McDonnell Foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Shi, C., Li, M. & Dushoff, J. Traditional Male Circumcision is Associated with Sexual Risk Behaviors in Sub-Saharan Countries Prioritized for Male Circumcision. AIDS Behav 24, 951–959 (2020). https://doi.org/10.1007/s10461-019-02473-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-019-02473-0