Abstract
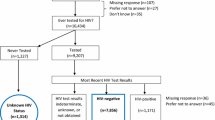
HIV testing is critical for timely care and controlling the HIV epidemic among men who have sex with men (MSM), particularly for regions with increasing infection rates such as China. This study investigated HIV testing and associated demographic, psychosocial, and risk behavior factors among internet-using Chinese MSM (n = 332). Most participants received HIV testing before (74.1%), which was associated with more HIV knowledge, online social life, and more frequent condomless anal sex. Among MSM who tested previously (n = 246), 48.4% reported regular HIV testing, which was associated with a greater online social life and less sexual identity concerns (internalized homonegativity and concealment motivation). Findings suggest a two-step approach to engage MSM who never tested for HIV and who do not undergo regular testing. Strategies to promote testing should enhance HIV knowledge, sex education, and online MSM community building. Interventions to increase acceptance and positivity of sexual identity are crucial to regular testing.
Resume
Pruebas del VIH son crítica para cuidado oportuno y controlando la epidemia de VIH entre hombres que tienen sexo con hombres (HSM), particularmente para regiones con tasas de infección en aumento tal como China. Este estudio investigó las pruebas de VIH y la asociada demográfico, psicológicos, y factores de comportamiento de riesgo entre HSH chinos que utilizan internet (n = 332). La mayoría de los participantes recibieron pruebas de VIH antes (74.1%), que se asoció con más conocimiento del VIH, vida social en línea, y sexo anal sin condón más frecuente. Entre HSH que probó previamente (n = 246), 48.4% reportaron pruebas de VIH regulares, que fue asociado con una mayor vida social en línea y menos preocupaciones de identidad sexual (homonegatividad interiorizada y motivación de ocultamiento). Resultados sugieren un enfoque de dos pasos para engancharse HSM que nunca ha probado para VIH y que no someterse pruebas con regularidad. Estrategias para promover las pruebas debería mejorar VIH conocimiento, educación sexual, y HSM construcción comunitaria en línea. Las intervenciones para aumentar la aceptación y la positividad de la identidad sexual son cruciales para las pruebas regulares.
Similar content being viewed by others
References
National Health and Family Planning Commission of China. 2015 China AIDS Response Progress Report. In: Global AIDS Response Progress Reporting. 2015. p. 1–26.
Chow EPF, Wilson DP, Zhang J, Jing J, Zhang L. Human immunodeficiency virus prevalence is increasing among men who have sex with men in China: findings from a review and meta-analysis. Sex Transm Dis. 2011;38(9):845–57.
Rotheram-Borus MJ, Newman PA, Etzel MA. Effective detection of HIV. J Acquir Immune Defic Syndr. 2000;25:105–14.
Branson BM, Handsfield HH, Lampe MA, Janssen RS, Taylor AW, Lyss SB, Clark JE. Revised recommendations for HIV testing of adults, adolescents, and pregnant women in health care settings. Ann Emerg Med. 2007;49(5):575–7.
Liu S, Wang K, Yao S, Guo X, Liu Y, Wang B. Knowledge and risk behaviors related to HIV/AIDS, and their association with information resource among men who have sex with men in Heilongjiang province, China. BMC Public Health. 2010;10:250.
Wu J. From, “Long Yang” and “Dui Shi” to Tongzhi: homosexuality in China. J Gay Lesbian Psychother. 2003;7(1–2):117–43.
Steward WT, Miège P, Choi K-H. Charting a moral life: the influence of stigma and filial duties on marital decisions among Chinese men who have sex with men. PLoS ONE. 2013;8(8):e71778.
Zhang B, Chu Q. MSM and HIV/AIDS in China. Cell Res. 2010;15:858–64.
Bien CH, Best JM, Muessig KE, Wei C, Han L, Tucker JD. Gay apps for seeking sex partners in China: implications for MSM sexual health. AIDS Behav. 2015;19(6):941–6.
Saxton P, Dickson N, Hughes A. Who is omitted from repeated offline HIV behavioural surveillance among MSM? Implications for interpreting trends. AIDS Behav. 2013;17(9):3133–44.
Noble M, Jones AM, Bowles K, DiNenno EA, Tregear SJ. HIV testing among internet-using MSM in the United States: systematic review. AIDS Behav. 2017;21(2):561–75.
Pachankis JE, Hatzenbuehler ML, Hickson F, Weatherburn P, Berg RC, Marcus U, Schmidt AJ. Hidden from health: structural stigma, sexual orientation concealment, and HIV across 38 countries in the European MSM Internet Survey. AIDS. 2015;29(10):1239–46.
Brito AM, Kendall C, Kerr L, Mota RMS, Guimarães MDC, Dourado I, Pinho AA, Benzaken AS, Brignol S, Reingold AL. Factors associated with low levels of HIV testing among men who have sex with men (MSM) in Brazil. PLoS ONE. 2015;10(6):1–14.
Young SD, Holloway I, Jaganath D, Rice E, Westmoreland D, Coates T. Project HOPE: online social network changes in an HIV prevention randomized controlled trial for African American and Latino men who have sex with men. Am J Public Health. 2014;104(9):1707–12.
Zou H, Hu N, Xin Q, Beck J. HIV testing among men who have sex with men in China: a systematic review and meta-analysis. AIDS Behav. 2012;16:1717–28.
Song Y, Li X, Zhang L, Fang X, Lin X, Liu Y, Stanton B. HIV-testing behavior among young migrant men who have sex with men (MSM) in Beijing, China. AIDS Care. 2011;23(2):179–86.
Li R, Pan X, Ma Q, Wang H, He L, Jiang T, Wang D, Zhang Y, Zhang X, Xia S. Prevalence of prior HIV testing and associated factors among MSM in Zhejiang Province, China: a cross-sectional study. BMC Public Health. 2016;16(1):1–8.
Zhou J, Chen J, Goldsamt L, Wang H, Zhang C, Li X. HIV testing and associated factors among men who have sex with men in Changsha, China. J Assoc Nurses AIDS Care. 2018;29(6):932–41.
Li X, Wu G, Lu R, Feng L, Fan W, Xiao Y, Sun Z, Zhang H, Xing H, Shao Y, Ruan Y. HIV-testing behavior and associated factors among MSM in Chongqing, China. Medicine (Baltimore). 2014;93(27):1–9.
Zhao P, Liu L, Zhang Y, Cheng H, Cao B, Liu C, Wang C, Yang B, Wei C, Tucker JD, Tang W. The interaction between HIV testing social norms and self-efficacy on HIV testing among Chinese men who have sex with men: results from an online cross-sectional study. BMC Infect Dis. 2018;18(1):1–8.
Wei C, Wong T, Liu C, Mao J, Tang S, Yang B, Tucker JD, Zhang TP, Tang W, Han L, Zhang Y. Community engagement in sexual health and uptake of HIV testing and syphilis testing among MSM in China: a cross-sectional online survey. J Int AIDS Soc. 2017;20(1):21372.
Han L, Bien C, Wei C, Muessig K, Yang M, Liu F, Yang L, Meng G, Emch M, Tucker J. An online survey of HIV self testing among MSM in China: implications for expanding HIV testing among key populations. J Acquir Immune Defic Syndr. 2014;67(2):216–21.
Tsui HY, Lau JTF. Comparison of risk behaviors and socio-cultural profile of men who have sex with men survey respondents recruited via venues and the internet. BMC Public Health. 2010;10:232–42.
Meyer IH. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychol Bull. 2003;129(5):674–97.
Emory University. American Men’s Internet Survey (AMIS): online HIV behavioral survey of men who have sex with men. In: PRISM Health. Atlanta, GA; 2014.
Sanchez TH, Zlotorzynska M, Sineath RC, Kahle E, Tregear S, Sullivan PS. National trends in sexual behavior, substance use and HIV testing among United States men who have sex with men recruited online, 2013 Through 2017. AIDS Behav. 2018;22(8):2413–25.
Wei C, Yan H, Yang C, Raymond HF, Li J, Yang H. Accessing HIV testing and treatment among men who have sex with men in China: a qualitative study. AIDS Care. 2014;26(3):372–8.
Carey MP, Schroder KEE. Development and psychometric evaluation of the brief HIV Knowledge Questionnaire. AIDS Educ Prev. 2002;14(2):172–82.
Wagenaar BH, Sullivan PS, Stephenson R. HIV knowledge and associated factors among internet-using men who have sex with men (MSM) in South Africa and the United States. PLoS ONE. 2012;7(3):1–8.
Mimiaga MJ, Reisner SL, Cranston K, Isenberg D, Bright D, Daf G, Bland S, Driscoll MA, Vanderwarker R, Vega B, Mayer KH. Sexual mixing patterns and partner characteristics of Black MSM in Massachusetts at increased risk for HIV infection and transmission. J Urban Health. 2009;86(4):602–23.
Pando MA, Balan I, Marone R, Dolezal C, Barreda V, Carballo-Dieguez A, Avila MM. HIV knowledge and beliefs among men who have sex with men (MSM) in Buenos Aires, Argentina. AIDS Behav. 2013;17:1305–12.
Mohr J, Fassinger R. Measuring dimensions of lesbian and gay male experience. Meas Eval Couns Dev. 2000;33:66–90.
Mohr J, Kendra MS. Revision and extension of a multidimensional measure of sexual minority identity: the lesbian, gay, and bisexual identity scale. J Couns Psychol. 2011;58(2):234–45.
Liu Y. The survey study of lesbian, gay, bisexual, and transgender identity in Taiwan (master dissertation). Taiwan: National Chi Nan University Institutional Repository; 2015.
R Core Team. R Development Core Team [Internet]. Vol. 55, R: A Language and Environment for Statistical Computing. 2016. p. 275–86. Available from: https://www.r-project.org/.
Huang L, Nehl EJ, Lin L, Meng G, Liu Q, Ross MW, Wong FY. Sociodemographic and sexual behavior characteristics of an online MSM sample in Guangdong, China. AIDS Care. 2014;26(5):648–52.
Hatzenbuehler ML, Nolen-Hoeksema S, Erickson SJ. Minority stress predictors of HIV risk behavior, substance use, and depressive symptoms: results from a prospective study of bereaved gay men. Health Psychol. 2008;27(4):455–62.
Mereish EH, Poteat VP, Mereish EH, Poteat VP. A relational model of sexual minority mental and physical health: the negative effects of shame on relationships, loneliness, and health. J Couns Psychol. 2015;62(3):425–37.
Millar BM, Wang K, Pachankis JE. The moderating role of internalized homonegativity on the efficacy of LGB-affirmative psychotherapy: results from a randomized controlled trial with young adult gay and bisexual men. J Consult Clin Psychol. 2016;84(7):565–70.
Feng Y, Wu Z, Detels R. Evolution of men who have sex with men community and experienced stigma among men who have sex with men in Chengdu, China. J Acquir Immune Defic Syndr. 2010;53(SUPPL. 1):98–103.
Zhang D, Bi P, Lv F, Zhang J, Hiller JE. Differences between Internet and community samples of MSM: implications for behavioral surveillance among MSM in China. AIDS Care. 2008;20(9):1128–37.
Pan S, Xu JJ, Han XX, Zhang J, Hu QH, Chu ZX, Hai YQ, Mao X, Yu YQ, Geng WQ, Jiang YJ, Shang H. Internet-based sex-seeking behavior promotes HIV infection risk: a 6-year serial cross-sectional survey to MSM in Shenyang, China. Biomed Res Int. 2016;2016:2860346.
Rosser BRS, Wilkerson JM, Smolenski DJ, Oakes JM, Konstan J, Horvath KJ, Kilian GR, Novak DS, Danilenko GP, Morgan R. The future of internet-based HIV prevention: a report on key findings from the Men’s INTernet (MINTS-I,II) sex studies. AIDS Behav. 2011;15(Suppl 1):S91–100. https://doi.org/10.1007/s10461-011-9910-5.
Bowen AM, Williams ML, Daniel CM, Clayton S. Internet based HIV prevention research targeting rural MSM: feasibility, acceptability, and preliminary efficacy. J Behav Med. 2008;31(6):463–77.
Holloway IW, Rice E, Gibbs J, Winetrobe H, Dunlap S, Rhoades H. Acceptability of smartphone application-based HIV prevention among young men who have sex with men. AIDS Behav. 2014;18(2):285–96.
Nehl EJ, He N, Wang X, Lin L, Wong FY, Yu F. Feasibility and willingness of using e-technologies for HIV prevention and research targeting Chinese MSM. AIDS Care. 2013;25(7):926–30.
Mi G, Wu Z, Wang X, Shi C, Yu F, Li T, Zhang L, McGoogan J, Pang L, Xu J, Rou K. Effects of a quasi-randomized web-based intervention on risk behaviors and treatment seeking among HIV-positive men who have sex with men in Chengdu, China. Curr HIV Res. 2015;13(6):490–6.
Burki T. Health and rights challenges for China’s LGBT community. Lancet. 2017;389(10076):1286.
Cao J, Guo L. Chinese, “Tongzhi” community, civil society, and online activism. Commun Public. 2017;1(4):504–8.
Institute of Medicine. The health of lesbian, gay, bisexual, and transgender people: Building a foundation for better understanding. Washington, DC: The National Academies Press; 2011.
Acknowledgements
This work was affiliated by the Providence/Boston Center for AIDS Research (P30AI042853). We would like to acknowledge Beijing LGBT Center, Division of Psychology for their support.
Funding
This research was supported by a grant from the Global Health Institute of University of Wisconsin-Madison awarded to the first author.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors have any conflicts of interest to report.
Ethical Approval
All procedures performed in the study involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
All participants provided their consent to the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sun, S., Whiteley, L. & Brown, L.K. HIV Testing Among Chinese Men Who Have Sex with Men: The Roles of HIV Knowledge, Online Social Life, and Sexual Identity Concerns. AIDS Behav 24, 437–449 (2020). https://doi.org/10.1007/s10461-019-02471-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-019-02471-2