Abstract
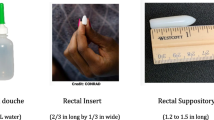
Tenofovir administration via rectal douching results in higher rectal-mucosa drug concentration than oral administration. Many who engage in receptive anal intercourse (RAI) use cleansing rectal douches. To inform development of a behaviorally-congruent tenofovir douche, 4751 individuals ≥ 18 years-old, born male, from all US states/territories, who engaged in anal intercourse responded to an online survey. Of those who reported RAI in the prior 3 months, 80% douched beforehand, 82% within 1 h, mean 2.9 consecutive applications; 27% douched afterwards, 83% within 1 h, mean 1.7 consecutive applications. Among multidose users, 78% applied doses within 2 min, and 76% retained liquid < 1 min. Most used tap water (89%) in an enema bottle (50%) or rubber bulb (43%), and douched for cleanliness (97%), to avoid smelling bad (65%), and to enhance pleasure (24%). 98% reported high likelihood of using an HIV-prevention douche. An ideal product will protect within a user’s typical number of applications, within 1 h, and be dissolvable in tap water.
Resumen
La administración de tenofovir por medio de una ducha rectal resulta en una concentración de droga en la mucosa rectal más alta que por vía oral. Muchos de los que tienen sexo anal receptivo (SAR) usan duchas rectales para limpiarse. Para informar el desarrollo de una ducha rectal congruente con los comportamientos habituales de los usuarios, 4751 individuos mayores de 18 años, nacidos varones, de todos los estados y territorios de los EEUU, que tenían sexo anal respondieron a una encuesta por Internet. De los que reportaron SAR en los últimos 3 meses, 80% usaron una ducha previamente, 82% dentro de una hora, con un promedio de 2.9 aplicaciones consecutivas; 27% usaron una ducha posteriormente, 83% dentro de una hora, con un promedio de 1.7 aplicaciones consecutivas. De los que usaron múltiples dosis, 78% aplicaron las dosis dentro de 2 minutos, y 76% retuvieron el líquido < 1 minuto. La mayoría usó agua corriente (89%) en una botella de enema (50%) o un bulbo de goma (43%), y se ducharon para estar limpios (97%), para evitar feos olores (65%), y para aumentar el placer (24%). 98% reportó alta probabilidad de usar una ducha que prevenga el VIH. El producto ideal debería proteger dentro del número típico de aplicaciones del usuario, dentro de una hora, y ser soluble en agua corriente.


Similar content being viewed by others
References
Grant RM, Lama JR, Anderson PL, et al. Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. N Engl J Med. 2010;363(27):2587–99. https://doi.org/10.1056/NEJM0a1011205.
Molina JM, Capitant C, Spire B, et al. On-demand preexposure prophylaxis in men at high risk for HIV-1 infection. N Engl J Med. 2015;373(23):2237–46. https://doi.org/10.1056/NEJMoa1506273.
Schlesinger E, Johengen D, Luecke E, et al. A tunable, biodegradable, thin-film polymer device as long-acting implant delivering tenofovir alafenamide fumarate for HIV pre-exposure prophylaxis. Pharm Res. 2016;33(7):1649–56. https://doi.org/10.1007/s11095-016-1904-6.
Spreen WR, Margolis DA, Pottage JC Jr. Long-acting injectable antiretrovirals for HIV treatment and prevention. Curr Opin HIV AIDS. 2013;8(6):565–71. https://doi.org/10.1097/COH.0000000000000002.
Golub SA, Gamarel KE, Rendina HJ, Surace A, Lelutiu-Weinberger CL. From efficacy to effectiveness: facilitators and barriers to PrEP acceptability and motivations for adherence among MSM and transgender women in New York City. AIDS Patient Care STDS. 2013;27(4):248–54. https://doi.org/10.1089/apc.2012.0419.
Carballo-Diéguez A, Giguere R, Dolezal C, et al. Preference of oral tenofovir disoproxil fumarate/emtricitabine versus rectal tenofovir reduced-glycerin 1% gel regimens for HIV prevention among cisgender men and transgender women who engage in receptive anal intercourse with men. AIDS Behav. 2017;21(12):3336–45. https://doi.org/10.1007/s10461-017-1969-1.
Peinado J, Lama JR, Galea JT, et al. Acceptability of oral versus rectal HIV preexposure prophylaxis among men who have sex with men and transgender women in Peru. J Int Assoc Provid AIDS Care. 2013;12(4):278–83. https://doi.org/10.1177/1545109712473650.
Newman PA, Duan N, Lee SJ, et al. HIV vaccine acceptability among communities at risk: the impact of vaccine characteristics. Vaccine. 2006;24(12):2094–101. https://doi.org/10.1016/j.vaccine.2005.11.013.
Newman PA, Logie C. HIV vaccine acceptability: a systematic review and meta-analysis. AIDS. 2010;24(11):1749–56. https://doi.org/10.1097/QAD.0b013e32833adbe8.
Baeten JM, Palanee-Phillips T, Brown ER, et al. Use of a vaginal ring containing dapivirine for HIV-1 prevention in women. N Engl J Med. 2016;375(22):2121–32. https://doi.org/10.1056/nejmoa1506110.
Carballo-Diéguez A, Giguere R, Dolezal C, et al. Rectal-specific microbicide applicator: evaluation and comparison with a vaginal applicator used rectally. AIDS Behav. 2014;18(9):1734–45. https://doi.org/10.1007/s10461-014-0793-0.
Giguere R, Rael CT, Sheinfil A, et al. Factors supporting and hindering adherence to rectal microbicide gel use with receptive anal intercourse in a Phase 2 trial. AIDS Behav. 2018;22(2):388–401. https://doi.org/10.1007/s10461-017-1980-7.
Bauermeister JA, Giguere R, Leu CS, et al. Patterns of rectal microbicide placebo gel use in a preparatory stage for a Phase 1 trial among young men who have sex with. men. AIDS Behav. 2018;22(2):412–20. https://doi.org/10.1007/s10461-017-1847-x.
Bauermeister J, Giguere R, Dolezal C, et al. To use a rectal microbicide, first insert the applicator: gel and applicator satisfaction among young men who have sex with men. AIDS Educ Prev. 2016;28(1):1–10. https://doi.org/10.1521/aeap.2016.28.1.1.
Gross M, Celum C, Tabet SR, Clifton K, Coletti AS, Chesney MA. Acceptability of a bioadhesive nonoxynol-9 gel delivered by an applicator as a rectal microbicide. Sex Transm Dis. 1999;26(10):572–8.
Carballo-Diéguez A, Bauermeister JA, Ventuneac A, Dolezal C, Balan I, Remien RH. The use of rectal douches among HIV-uninfected and infected men who have unprotected receptive anal intercourse: implications for rectal microbicides. AIDS Behav. 2008;12(6):860–6. https://doi.org/10.1007/s10461-007-9301-0.
Carballo-Diéguez A, Bauermeister J, Ventuneac A, Dolezal C, Mayer K. Why rectal douches may be acceptable rectal-microbicide delivery vehicles for MSM. Sex Transm Dis. 2010;37(4):228–33. https://doi.org/10.1097/OLQ.0b013e3181bj9b2d.
Carballo-Diéguez A, Lentz C, Giguere R, Fuchs EJ, Hendrix CW. Rectal douching associated with receptive anal intercourse: a literature review. AIDS Behav. 2018;22(4):1288–94. https://doi.org/10.1007/s10461-017-1959-3.
Calabrese SK, Rosenberger JG, Schick VR, Novak DS, Reece M. An event-level comparison of risk-related sexual practices between black and other-race men who have sex with men: condoms, semen, lubricant and rectal douching. AIDS Patient Care STDS. 2013;27(2):77–84. https://doi.org/10.1089/apc.2012/0355.
Javanbakht M, Stahlman S, Pickett J, Leblanc MA, Gorbach PM. Prevalence and types of rectal douches used for anal intercourse: results from an international survey. BMC Infect Dis. 2014;14:1–8. https://doi.org/10.1186/1471-2334-14-95.
Achterbergh RCA, vann der Helm JJ, van den Boom W, et al. Is rectal douching and sharing douching equipment associated with anorectal chlamydia and gonorrhea? A cross-sectional study among men who have sex with men. Sex Transm Infect. 2017;93(6):431–7. https://doi.org/10.1136/sextrans-2016-052777.
Galea JT, Kinsler JJ, Imrie J, Nureña CR, Sánchez J, Cunningham WE. Rectal douching and implications for rectal microbicides among populations vulnerable to HIV in South America: a qualitative study. Sex Transm Infect. 2014;90(1):33–5. https://doi.org/10.1136/sextrans-2013-051154.
Mitchell JW, Sophus AI, Lee J-Y, Petroll AE. Anal douche practices and willingness to use a rectal microbicide enema for HIV prevention and associated factors among an Internet sample of HIV-negative and HIV-discordant male couples in the US. AIDS Behav. 2016;20(11):2578–87. https://doi.org/10.1007/s10461-015-1250-4.
Leyva FJ, Bakshi RP, Fuchs EJ, et al. Isoosmolar enemas demonstrate preferential gastrointestinal distribution, safety, and acceptability compared with hyperosmolar and hypoosmolar enemas as a potential delivery vehicle for rectal microbicides. AIDS Res Hum Retroviruses. 2013;29(11):1487–95. https://doi.org/10.1089/AID.2013.0189.
Maisel K, Chattopadhyay S, Moench T, et al. Enema ion compositions for enhancing colorectal drug delivery. J Control Release. 2015;209:280–7.
Weld ED, Fuchs E, Marzinke M, et al. Tenofovir enema as HIV PrEP for receptive anal intercourse: Safety, pharmacokinetics, pharmacodynamics and acceptability (DREAM 01). [MOLBPEC33] Presented at the 9th International AIDS Society Conference on HIV Science; 2017; Paris.
United States Census Bureau. QuickFacts United States. U.S. Department of Commerce. https://www.census.gov/quickfacts/fact/table/US/PST045217#viewtop. Accessed 29 March 2018.
Mensch BS, van der Straten A, Katzen LL. Acceptability in microbicide and PrEP trials: current status and a reconceptualization. Curr Opin HIV AIDS. 2012;7(6):534–41. https://doi.org/10.1097/COH.0b013e3283590632.
Miskell P. How Crest made business history. Harvard Business School: Working Knowledge. https://hbswk.hbs.edu/archive/how-crest-made-business-history. Accessed 12 April 2018.
Acknowledgements
We would like to thank the study participants, who took the time to complete the survey to contribute to our knowledge of douching practices, and the entire DREAM U19 study team for their input on the survey content. The study was funded by a U19 Grant under the Integrated Preclinical-Clinical Program for HIV Topical Microbicides (IPCP-HTM), Division of AIDS, National Institute of Allergy and Infectious Diseases, National Institutes of Health (NIH) (AI113127). This work was also supported by a Center Grant from the NIMH to the HIV Center for Clinical and Behavioral Studies at New York State Psychiatric Institute and Columbia University (P30-MH43520; PI: Remien, PhD). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None to declare.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Carballo-Dieguez, A., Giguere, R., Lentz, C. et al. Rectal Douching Practices Associated with Anal Intercourse: Implications for the Development of a Behaviorally Congruent HIV-Prevention Rectal Microbicide Douche. AIDS Behav 23, 1484–1493 (2019). https://doi.org/10.1007/s10461-018-2336-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-018-2336-6