Abstract
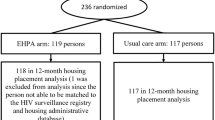
Though housing instability is linked to poor HIV health outcomes, studies that assess the HIV treatment cascade by housing status are limited. Using data from a multi-site Retention in Care initiative we constructed HIV treatment cascades for participants (n = 463) of five grantee sites. We found no significant differences in viral suppression at follow-up among participants who were unstably housed at enrollment (49%) as compared to those who were stably housed at enrollment (54%). Among participants with available data at 6- or 12-month follow-up, 94% were engaged in care, 90% were retained in, 94% were on ART, and 71% had suppressed viral load. Some site-level differences were noted; at two of the sites participants who were stably housed were more likely to be retained in care and on ART. Overall, findings demonstrated that participants moved successfully through the HIV treatment cascade regardless of housing status at enrollment, suggesting that evidence-based support and services to help people living with HIV/AIDS can help mitigate barriers to engagement in care associated with lack of stable housing.
Similar content being viewed by others
References
Gardner EM, McLees MP, Steiner JF, Del Rio C, Burman WJ. The spectrum of engagement in HIV care and its relevance to test-and-treat strategies for prevention of HIV infection. Clin Infect Dis. 2011;52(6):793–800.
Bhunu CP. Assessing the impact of homelessness on HIV/AIDS transmission dynamics. Cogent Math. 2015;2(1):1021602.
Cohen MS, Chen YQ, McCauley M, Gamble T, Hosseinipour MC, Kumarasamy N, et al. Prevention of HIV-1 infection with early antiretroviral therapy. N Engl J Med. 2011;365(6):493–505.
Hall HI, Tang T, Westfall AO, Mugavero MJ. HIV care visits and time to viral suppression, 19 U.S. jurisdictions, and implications for treatment, prevention and the national HIV/AIDS strategy. PLoS ONE. 2013;8(12):e84318.
Gray KM, Cohen SM, Hu X, Li J, Mermin J, Hall HI. Jurisdiction level differences in HIV diagnosis, retention in care, and viral suppression in the United States. J Acquir Immune Defic Syndr. 2014;65(2):129–32.
Barnighausen T. The HIV treatment cascade and antiretroviral impact in different populations. Curr Opin HIV AIDS. 2015;10:391–4.
Bobat R, Archary M, Lawler M. An update on the HIV treatment cascade in children and adolescents. Curr Opin HIV AIDS. 2015;10(6):411–9.
Buskin SE, Kent JB, Dombrowski JC, Golden MR. Migration distorts surveillance estimates of engagement in care: results of public health investigations of persons who appear to be out of HIV care. Sex Transm Dis. 2014;41(1):35–40.
Edun B, Iyer M, Albrecht H, Weissman S. The South Carolina HIV cascade of care. South Med J. 2015;108(11):670–4.
Horberg MA, Hurley LB, Klein DB, Towner WJ, Kadlecik P, Antoniskis D, et al. The HIV care cascade measured over time and by age, sex, and race in a large national integrated care system. AIDS Patient Care STDS. 2015;29(11):582–90.
Iroh PA, Mayo H, Nijhawan AE. The HIV care cascade before, during, and after incarceration: a systematic review and data synthesis. Am J Public Health. 2015;105(7):e5–16.
Lessells RJ, Swaminathan S, Godfrey-Faussett P. HIV treatment cascade in tuberculosis patients. Curr Opin HIV AIDS. 2015;10(6):439–46.
Mangal JP, Rimland D, Marconi VC. The continuum of HIV care in a Veterans’ affairs clinic. AIDS Res Hum Retrovir. 2014;30(5):409–15.
Maulsby C, Charles V, Kinsky S, Riordan M, Jain K, Holtgrave D. Positive charge: filling the gaps in the U.S. HIV continuum of care. AIDS Behav. 2015;19(11):2097–107.
Milloy MJ, Montaner JS, Wood E. Incarceration of people living with HIV/AIDS: implications for treatment-as-prevention. Curr HIV/AIDS Rep. 2014;11(3):308–16.
Nijhawan AE. Infectious diseases and the criminal justice system. Am J Med Sci. 2016;352(4):399–407.
Phelps BR, Ahmed S, Amzel A, Diallo MO, Jacobs T, Kellerman SE, et al. Linkage, initiation and retention of children in the antiretroviral therapy cascade: an overview. AIDS. 2013;27(Suppl 2):S207–13.
Risher K, Mayer KH, Beyrer C. HIV treatment cascade in MSM, people who inject drugs, and sex workers. Curr Opin HIV AIDS. 2015;10(6):420–9.
Saghayam S, Wanke C. The impact of nutritional status and nutrition supplementation on outcomes along the HIV treatment cascade in the resource-limited setting. Curr Opin HIV AIDS. 2015;10(6):472–6.
Santos GM, Wilson EC, Rapues J, Macias O, Packer T, Raymond HF. HIV treatment cascade among transgender women in a San Francisco respondent driven sampling study. Sex Transm Infect. 2014;90(5):430–3.
Shaw S, Amico KR. Antiretroviral therapy adherence enhancing interventions for adolescents and young adults 13–24 years of age: a review of the evidence base. J Acquir Immune Defic Syndr. 2016;72(4):387–99.
Tanser F, Barnighausen T, Vandormael A, Dobra A. HIV treatment cascade in migrants and mobile populations. Curr Opin HIV AIDS. 2015;10(6):430–8.
Vagenas P, Azar MM, Copenhaver MM, Springer SA, Molina PE, Altice FL. The impact of alcohol use and related disorders on the HIV continuum of care: a systematic review : alcohol and the HIV continuum of care. Curr HIV/AIDS Rep. 2015;12(4):421–36.
Williams EC, Hahn JA, Saitz R, Bryant K, Lira MC, Samet JH. Alcohol use and human immunodeficiency virus (HIV) infection: current knowledge, implications, and future directions. Alcohol Clin Exp Res. 2016;40(10):2056–72.
Zanoni BC, Mayer KH. The adolescent and young adult HIV cascade of care in the United States: exaggerated health disparities. AIDS Patient Care STDS. 2014;28(3):128–35.
Terzian AS, Irvine MK, Hollod LM, Lim S, Rojas J, Shepard CW. Effect of HIV housing services on engagement in care and treatment, New York City, 2011. AIDS Behav. 2015;19(11):2087–96.
Leaver CA, Bargh G, Dunn JR, Hwang SW. The effects of housing status on health-related outcomes in people living with HIV: a systematic review of the literature. AIDS Behav. 2007;11(6 Suppl):85–100.
Aidala A, Lee G, Abramson D, Messeri P, Sigeler A. Housing need, housing assistance, and connection to HIV medical care. AIDS Behav. 2007;11(Suppl):S101–15.
Aidala A, Wilson MG, Shubert V, Gogolishvili D, Globerman J, Rueda S, et al. Housing status, medical care, and health outcomes among people living with HIV/AIDS: a systematic review. Am J Public Health. 2016;106(1):95.
Milloy MJ, Marshall BD, Montaner J, Wood E. Housing status and the health of people living with HIV/AIDS. Curr HIV/AIDS Rep. 2012;9(4):364–74.
Friedman MS, Marshal MP, Stall R, Kidder DP, Henny KD, Courtenay-Quirk C, et al. Associations between substance use, sexual risk taking and HIV treatment adherence among homeless people living with HIV. AIDS Care. 2009;21(6):692–700.
Kidder DP, Wolitski RJ, Royal S, Aidala A, Courtenay-Quirk C, Holtgrave DR, et al. Access to housing as a structural intervention for homeless and unstably housed people living with HIV: rationale, methods, and implementation of the housing and health study. AIDS Behav. 2007;11(6 Suppl):149–61.
Kidder DP, Wolitski RJ, Campsmith ML, Nakamura GV. Health status, health care use, medication use, and medication adherence among homeless and housed people living with HIV/AIDS. Am J Public Health. 2007;97(12):2238–45.
Royal SW, Kidder DP, Patrabansh S, Wolitski RJ, Holtgrave DR, Aidala A, et al. Factors associated with adherence to highly active antiretroviral therapy in homeless or unstably housed adults living with HIV. AIDS Care. 2009;21(4):448–55.
Wolitski R, Kidder D, Pals S, Royal S, Aidala A, Stall R, et al. Randomized trial of the effects of housing assistance on the health and risk behaviors of homeless and unstably housed people living with HIV. AIDS Behav. 2010;14(3):493–503.
Wolitski R, Kidder D, Fenton K. HIV, homelessness, and public health: critical issues and a call for increased action. AIDS Behav. 2007;11(6 Suppl):167–71.
Thakarar K, Morgan JR, Gaeta JM, Hohl C, Drainoni M-L. Homelessness, HIV, and incomplete viral suppression. J Health Care Poor Underserved. 2016;27(1):145–56.
Khanijow K, Hirozawa A, Ancock B, Hsu LC, Bamberger J, Schwarcz SK. Difference in survival between housed and homeless individuals with HIV, San Francisco, 2002–2011. J Health Care Poor Underserved. 2015;26(3):1005–18.
Dowshen N, Nguyen GT, Gilbert K, Feiler A, Margo KL. Improving transgender health education for future doctors. Am J Public Health. 2014;104(7):e5–6.
Lim S, Harris TG, Nash D, Lennon MC, Thorpe LE. All-cause, drug-related, and HIV-related mortality risk by trajectories of jail incarceration and homelessness among adults in New York City. Am J Epidemiol. 2015;181(4):261–70.
Lennon CA, Pellowski JA, White AC, Kalichman SC, Finitsis DJ, Turcios-Cotto V, et al. Service priorities and unmet service needs among people living with HIV/AIDS: results from a nationwide interview of HIV/AIDS housing organizations. AIDS Care. 2013;25(9):1083–91.
Buchanan D, Kee R, Sadowski LS, Garcia D. The health impact of supportive housing for HIV-positive homeless patients: a randomized controlled trial. Am J Public Health. 2009;99(Suppl 3):S675–80.
Marshall BD, Elston B, Dobrer S, Parashar S, Hogg RS, Montaner JS, et al. The population Impact of eliminating homelessness on HIV viral suppression among people who use drugs. AIDS. 2015;30:933.
Giordano TP, Gifford AL, White AC Jr, Suarez-Almazor ME, Rabeneck L, Hartman C, et al. Retention in care: a challenge to survival with HIV infection. Clin Infect Dis. 2007;44(11):1493–9.
Mugavero M, Westfall A, Zinski A, Davila J, Drainoni M, Gardner L, et al. Measuring retention in HIV care: the elusive gold standard. J Acquir Immune Defic Syndr. 2012;61(5):574–80.
Blair JM, McNaghten AD, Frazier EL, Skarbinski J, Huang P, Heffelfinger JD. Clinical and behavioral characteristics of adults receiving medical care for HIV infection: medical monitoring project, United States, 2007. MMWR Surveill Summ. 2011;60(11):1–20.
Mugavero M, Davila J, Nevin C, Giordano T. From access to engagement: measuring retention in outpatient HIV clinical care. AIDS Patient Care STDS. 2010;24(10):607–13.
Gardner LI, Giordano TP, Marks G, Wilson TE, Craw JA, Drainoni ML, et al. Enhanced personal contact with HIV patients improves retention in primary care: a randomized trial in 6 US HIV clinics. Clin Infect Dis. 2014;59(5):725–34.
Enriquez M, Farnan R, Cheng AL, Almeida A, Del Valle D, Pulido-Parra M, et al. Impact of a bilingual/bicultural care team on HIV-related health outcomes. J Assoc Nurses AIDS Care. 2008;19(4):295–301.
Aidala AA, Wilson MG, Shubert V, Gogolishvili D, Globerman J, Rueda S, et al. Housing status, medical care, and health outcomes among people living with HIV/AIDS: a systematic review. Am J Public Health. 2016;106(1):e1–23.
Stone MM, Hager MA, Griffin JJ. Organizational characteristics and funding environments: a study of a population of United Way–affiliated nonprofits. Public Adm Rev. 2001;61(3):276–89.
Cornelius T, Jones M, Merly C, Welles B, Kalichman MO, Kalichman SC. Impact of food, housing, and transportation insecurity on ART adherence: a hierarchical resources approach. AIDS Care. 2017;29(4):449–57.
The 2016 Annual Homeless Assessment Report (AHAR) to Congress. The U.S. Department of Housing and Urban Development Office of Community Planning and Development; 2016.
Marshall BD, Kerr T, Shoveller JA, Patterson TL, Buxton JA, Wood E. Homelessness and unstable housing associated with an increased risk of HIV and STI transmission among street-involved youth. Health Place. 2009;15(3):753–60.
Pellowski JA, Kalichman SC, Matthews KA, Adler N. A pandemic of the poor: social disadvantage and the US HIV epidemic. Am Psychol. 2013;68(4):197–209.
Acknowledgements
The authors would like to express their gratitude to the Retention in Care sites and their dedicated staff who participated in this project, and especially to Dr. Maria Caban from BOOM! Health for her help conceptualizing this paper.
Bradley Boekeloo, Ph.D., Sc.M., Prevention Research Center, School of Public Health Room 0228, Building #255 Valley Drive, University of Maryland, College Park, MD, 20742; Abby Charles, Institute for Public Health Innovation, 1301 Connecticut Avenue NW, Washington, DC 20036; Maria Caban, Ph.D., Director of Evaluation, BOOM Health, 540 East Fordham Rd, Bronx, NY, 10458; Rebecca Dillingham, M.D., M.P.H., Director, Center for Global Health, School of Medicine, University of Virginia, 345 Crispell Drive, Room 2520, Charlottesville, VA 22908-1379; Erin C. Falvey, Ph.D., Associate Executive Director and Clinical Director, Christie’s Place, 2440 Third Avenue, San Diego, CA 92101; Tanya Geiger, Ph.D., Prevention Research Center, School of Public Health Room 0228, Building #255 Valley Drive, University of Maryland, College Park, MD, 20742; Mary Hawk, DrPH, LSW, Assistant Professor, University of Pittsburgh, Graduate School of Public Health, Department of Behavioral and Community Health Sciences, 6124 Parran Hall – 130 DeSoto Street, Pittsburgh, PA, 15261; Sarah G. Solomon, MPH, Research Manager, Cardea, 1809 Seventh, Avenue, STE 600, Seattle, Washington, 98101.
Funding
This study was funded by AIDS United in partnership with the MAC AIDS Fund. Dr. Maulsby’s effort on the preparation of this manuscript was supported in part by a Grant from National Institute of Mental Health (1K01MH111388-01A1).
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
All data collection activities by sites independently underwent IRB review prior to execution. Evaluation activities conducted by the institution overseeing evaluation activities were determined to be non-human subjects research.
Additional information
A list of the AIDS United Retention in Care Intervention Team is given in Acknowledgements section.
Rights and permissions
About this article
Cite this article
Hawk, M., Maulsby, C., Enobun, B. et al. HIV Treatment Cascade by Housing Status at Enrollment: Results from a Retention in Care Cohort. AIDS Behav 23, 765–775 (2019). https://doi.org/10.1007/s10461-018-2295-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-018-2295-y