Abstract
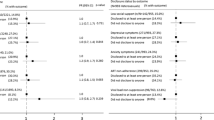
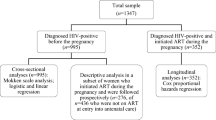
HIV status disclosure can help patients obtain support which may influence treatment adherence and subsequent healthcare needs. We examined the extent of disclosure and correlates of non-disclosure among 1180 adults newly initiating antiretroviral treatment (ART). While 91 % of those in a relationship shared their status with their partners, 14 % of the overall sample had not disclosed to anyone. Non-disclosure was positively associated with older age; control over household resources; and concerns about unintended disclosure, life disruptions, and family reactions. Knowing other HIV-positive people and longer time since diagnosis were associated with lower odds of non-disclosure. Most respondents reporting disclosure experienced supportive responses, frequently including decision to get an HIV test by confidants who had not known their own status. Although HIV status disclosure prior to ART initiation was high, some individuals cited concerns about unintended disclosure, gossip, and partner violence, and may benefit from additional disclosure support.
Resumen
La revelación del estado serológico del VIH puede ayudar a los pacientes a obtener apoyo que podría influir en la adherencia al tratamiento y en las necesidades de cuidado para su salud. Examinamos la frecuencia y factores asociados con la no revelación del estado serológico del VIH en 1180 adultos iniciando tratamiento antirretroviral (TARV) por primera vez. Mientras 91 % de los que estaban en una relación compartió su estado serológico con su pareja, 14 % de la muestra total no reveló su estado a nadie. La no revelación del estado serológico estuvo asociada positivamente con mayor edad, control sobre los recursos familiares, y preocupaciones sobre revelaciones no intencionales, interrupciones en la vida cotidiana y las reacciones familiares. Conocer otras personas VIH-positivas y mayor tiempo desde el diagnóstico estuvieron asociados con menor posibilidades de no revelación. La mayoría de los encuestados que revelaron su estado recibieron respuestas de apoyo, incluyendo una aceptación considerable del test de VIH en confidentes que no conocían su estado serológico. Aunque la revelación del VIH antes de iniciar TARV fue alta, ciertos individuos mencionaron preocupaciones sobre revelaciones no intencionales, chismes y violencia por parte de su pareja, y podrían beneficiarse de apoyo adicional para revelar su estado serológico.
Similar content being viewed by others
References
Joint United Nations Programme on HIV/AIDS. Opening up the HIV/AIDS epidemic. Guidance on encouraging beneficial disclosure, ethical partner counselling and appropriate use of HIV case-reporting. Geneva: World Health Organization. 2000.
Southern African AIDS Trust. Guidelines for Counseling on Disclosure of HIV Status. Southern African AIDS Trust. 2011.
Petrak JA, Doyle A-M, Smith A, Skinner C, Hedge B. Factors associated with self-disclosure of HIV serostatus to significant others. Br J Health Psychol. 2001;6(1):69.
Medley A, Garcia-Moreno C, McGill S, Maman S. Rates, barriers and outcomes of HIV serostatus disclosure among women in developing countries: implications for prevention of mother-to-child transmission programmes. Bull World Health Organ. 2004 Apr;82(4):299–307.
Deribe K, Woldemichael K, Njau BJ, Yakob B, Biadgilign S, Amberbir A. Gender differences regarding barriers and motivators of HIV status disclosure among HIV-positive service users. SAHARA J. 2010;7(1):30–9.
Deribe K, Woldemichael K, Wondafrash M, Haile A, Amberbir A. Disclosure experience and associated factors among HIV positive men and women clinical service users in Southwest Ethiopia. BMC Public Health. 2008;8:81.
Gari T, Habte D, Markos E. HIV positive status disclosure among women attending art clinic at Hawassa University Referral Hospital, South Ethiopia. East Afr J Public Health. 2010 Mar;7(1):87–91.
Genet M, Sebsibie G, Gultie T. Disclosure of HIV seropositive status to sexual partners and its associated factors among patients attending antiretroviral treatment clinic follow up at Mekelle Hospital, Ethiopia: a cross sectional study. BMC Res Notes. 2015;8:109.
Kassaye KD, Lingerh W, Dejene Y. Determinants and outcomes of disclosing HIV-sero positive status to sexual partners among women in Mettu and Gore towns, Illubabor Zone southwest Ethiopia. Ethiop J Health Dev. 2005;19(2):126–31.
Reda AA, Biadgilign S, Deribe K, Deribew A. HIV-positive status disclosure among men and women receiving antiretroviral treatment in eastern Ethiopia. AIDS Care. 2013 Aug;25(8):956–60.
Seid M, Wasie B, Admassu M. Disclosure of HIV positive result to a sexual partner among adult clinical service users in Kemissie district, northeast Ethiopia. Afr J Reprod Health. 2012 Mar;16(1):97–104.
Alemayehu M, Aregay A, Kalayu A, Yebyo H. HIV disclosure to sexual partner and associated factors among women attending ART clinic at Mekelle hospital, Northern Ethiopia. BMC Public Health. 2014;14:746.
Mills EJ, Nachega JB, Buchan I, Orbinski J, Attaran A, Singh S, et al. Adherence to antiretroviral therapy in sub-Saharan Africa and North America: a meta-analysis. JAMA J Am Med Assoc. 2006 Aug 9;296(6):679–90.
Skhosana N, Struthers H, Gray G, McIntyre J. HIV disclosure and other factors that impact on adherence to antiretroviral therapy: the case of Soweto, South Africa. Afr J AIDS Res. 2006;5(1):17–26.
Kalichman SC, Nachimson D. Self-efficacy and disclosure of HIV-positive serostatus to sex partners. Health Psychol. 1999 May;18(3):281–7.
Stirratt MJ, Remien RH, Smith A, Copeland OQ, Dolezal C, Krieger D. The role of HIV serostatus disclosure in antiretroviral medication adherence. AIDS Behav. 2006 Sep;10(5):483–93.
Waddell EN, Messeri PA. Social support, disclosure, and use of antiretroviral therapy. AIDS Behav. 2006 May;10(3):263–72.
Central Statistical Agency [Ethiopia] and ICF International. Ethiopia Demographic and Health Survey. Addis Ababa: Central Statistical Agency and ICF International. 2011.
Joint United Nations Programme on HIV/AIDS (UNAIDS). Global report: UNAIDS report on the global AIDS epidemic 2013. Geneva. 2013. 978-92-9253-032-7.
Federal HIV/AIDS Prevention and Control Office. Federal Ministry of Health. Guidelines for Implementation of the Antiretroviral Therapy Programme in Ethiopia. Federal HIV/AIDS Prevention and Control Office. Federal Ministry of Health. 2007
Earnshaw VA, Chaudoir SR. From conceptualizing to measuring HIV stigma: a review of HIV stigma mechanism measures. AIDS Behav. 2009;13(6):1160–77.
Makin JD, Forsyth BW, Visser MJ, Sikkema KJ, Neufeld S, Jeffery B. Factors affecting disclosure in South African HIV-positive pregnant women. AIDS patient care and STDs. 2008 Nov;22(11):907–16.
Kulkarni S, Hoffman S, Gadisa T, Melaku Z, Fantehun M, Yigzaw M, et al. Identifying perceived barriers along the HIV care continuum: findings from providers, peer educators, and observations of provider-patient interactions in Ethiopia. J Intern Assoc Provid AIDS Care. 2015. doi:10.1177/2325957415593635.
Akani CI, Erhabor O. Rate, pattern and barriers of HIV serostatus disclosure in a resource-limited setting in the Niger delta of Nigeria. Trop Doct. 2006;36(2):87–9.
Antelman G, Smith Fawzi MC, Kaaya S, Mbwambo J, Msamanga GI, Hunter DJ, et al. Predictors of HIV-1 serostatus disclosure: a prospective study among HIV-infected pregnant women in Dar es Salaam, Tanzania. AIDS (London, England). 2001;15(14):1865–74.
Ezegwui HU, Nwogu-Ikojo EE, Enwereji JO, Dim CC. HIV serostatus disclosure pattern among pregnant women in Enugu, Nigeria. J Biosoc Sci. 2009 Nov;41(6):789–98.
Kadowa I, Nuwaha F. Factors influencing disclosure of HIV positive status in Mityana district of Uganda. Afr Health Sci. 2009;9(1):26–33.
Longinetti E, Santacatterina M, El-Khatib Z. Gender perspective of risk factors associated with disclosure of HIV status, a cross-sectional study in Soweto, South Africa. PLoS ONE. 2014;9(4):e95440.
Maman S, Mbwambo JK, Hogan NM, Weiss E, Kilonzo GP, Sweat MD. High rates and positive outcomes of HIV-serostatus disclosure to sexual partners: reasons for cautious optimism from a voluntary counseling and testing clinic in Dar es Salaam, Tanzania. AIDS Behav. 2003 Dec;7(4):373–82.
Ndiaye C, Boileau C, Zunzunegui MV, Koala S, Aboubacrine SA, Niamba P, et al. Gender-related factors influencing HIV serostatus disclosure in patients receiving HAART in West Africa. World Health Popul. 2008;10(3):43–54.
Farquhar C, Ngacha D, Bosire R, Nduati R, Kreiss J, John G, editors. Prevalence and correlates of partner notification regarding HIV-1 in an antenatal setting in Nairobi, Kenya. XIII International AIDS Conference; 2000.
Cohen MS, Chen YQ, McCauley M, Gamble T, Hosseinipour MC, Kumarasamy N, et al. Prevention of HIV-1 infection with early antiretroviral therapy. N Engl J Med. 2012 Aug 11;365(6):493–505.
Acknowledgments
This study was funded by a grant from the National Institutes of Health R01 (5R01MH89831) entitled “Multi-level determinants of late ART initiation in sub-Saharan Africa” (LSTART) and the President’s Emergency Plan for AIDS Relief (PEPFAR).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gadisa, T., Tymejczyk, O., Kulkarni, S.G. et al. Disclosure History Among Persons Initiating Antiretroviral Treatment at Six HIV Clinics in Oromia, Ethiopia, 2012–2013. AIDS Behav 21, 70–81 (2017). https://doi.org/10.1007/s10461-016-1290-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-016-1290-4