Abstract
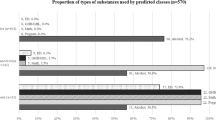
Men who have sex with men (MSM) are the largest risk group in the US HIV epidemic and African American MSM (AA MSM) are disproportionately affected. Substance-abusing sexual minorities warrant attention as they are at elevated risk for HIV, yet are not a homogeneous risk group. The purpose of this study was to use latent class analysis to identify patterns of drug and alcohol use in a sample of 359 AA MSM and examine associations with sexual risk. Three classes were identified: Individuals who used multiple substances (poly-users) (18 %), alcohol/marijuana users (33 %) and individuals who had low probability of reporting drug or problematic alcohol use (50 %). Results from multivariate analysis indicate that poly-users were older and more likely to report sex exchange and recent sexually transmitted infection compared to the other classes. Alcohol and poly-users were more likely to report sex under the influence. Identifying and defining substance use patterns can improve specification of risk groups and allocation of prevention resources.

Similar content being viewed by others
References
Centers for Disease Control and Prevention (CDC). Estimated HIV incidence among adults and adolescents in the United States, 2007–2010. HIV Surveillance Supplemental Report 2012;0017(No. 4).
Kader R, Govender R, Seedat S, Koch JR, Parry C. Understanding the impact of hazardous and harmful use of alcohol and/or other drugs on ARV adherence and disease progression. PLoS One. 2015;10(5):e0125088.
Parsons JT, Starks TJ, Millar BM, Boonrai K, Marcotte D. Patterns of substance use among HIV-positive adults over 50: implications for treatment and medication adherence. Drug Alcohol Depend. 2014;139:33–40.
McCabe SE, West BT, Hughes TL, Boyd CJ. Sexual orientation and substance abuse treatment utilization in the United States: results from a national survey. J Subst Abuse Treat. 2013;44:4.
Lambert E, Normand J, Stall R, Aral S, Vlahov D. Introduction: new dynamics of HIV risk among drug-using men who have sex with men. J Urban Health. 2005;82(1 Suppl 1):i1–8.
Finlayson T, Le B, Smith A, Bowles K, Cribbin M, Miles I, et al. HIV risk, prevention, and testing behaviors among men who have sex with men-National HIV Behavioral Surveillance System, 21 U.S. Cities, United States, 2008. MMWR Surveill Summ. 2011;60(14):1–38.
Newcomb ME, Ryan DT, Greene GJ, Garofalo R, Mustanski B. Prevalence and patterns of smoking, alcohol use, and illicit drug use in young men who have sex with men. Drug Alcohol Depend. 2014;1(141):65–71.
Lim SH, Cheung DH, Guadamuz TE, Wei C, Koe S, Altice FL. Latent class analysis of substance use among men who have sex with men in Malaysia: findings from the Asian internet MSM sex survey. Drug Alcohol Depend. 2015;151:31–7.
Colfax G, Coates TJ, Husnik MJ, Huang Y, Buchbinder S, Koblin B, et al. Longitudinal patterns of methamphetamine, popper (amyl nitrite), and cocaine use and high-risk sexual behavior among a cohort of San Francisco men who have sex with men. J Urban Health. 2005;82(1 Suppl 1):i62–70.
Plankey MW, Ostrow DG, Stall R, Cox C, Li X, Peck JA, et al. The relationship between methamphetamine and popper use and risk of HIV seroconversion in the multicenter AIDS cohort study. J Acquir Immune Defic Syndr. 2007;45(1):85–92.
McCutcheon A. Latent class analysis. Newbury Park: Sage; 1987.
Olino TM, Klein DN, Lewinsohn PM, Rohde P, Seeley JR. Latent trajectory classes of depressive and anxiety disorders from adolescence to adulthood: descriptions of classes and associations with risk factors. Compr Psychiatry. 2010;51(3):224–35.
Monga N, Rehm J, Fischer B, Brissette S, Bruneau J, El-Guebaly N, et al. Using latent class analysis (LCA) to analyze patterns of drug use in a population of illegal opioid users. Drug Alcohol Depend. 2007;88(1):1–8.
Kuramoto SJ, Bohnert AS, Latkin CA. Understanding subtypes of inner-city drug users with a latent class approach. Drug Alcohol Depend. 2011;118(2–3):237–43.
Ko JY, Martins SS, Kuramoto SJ, Chilcoat HD. Patterns of alcohol-dependence symptoms using a latent empirical approach: associations with treatment usage and other correlates. J Stud Alcohol Drugs. 2010;71(6):870–8.
Wittchen HU, Behrendt S, Hofler M, Perkonigg A, Rehm J, Lieb R, et al. A typology of cannabis-related problems among individuals with repeated illegal drug use in the first three decades of life: evidence for heterogeneity and different treatment needs. Drug Alcohol Depend. 2009;102(1–3):151–7.
Sherman SG, Sutcliffe CG, German D, Sirirojn B, Aramrattana A, Celentano DD. Patterns of risky behaviors associated with methamphetamine use among young Thai adults: a latent class analysis. J Adolesc Health. 2009;44(2):169–75.
Agrawal A, Lynskey MT, Madden PAF, Bucholz KK, Heath AC. A latent class analysis of illicit drug abuse/dependence: results from the national epidemiological survey on alcohol and related conditions. Addiction. 2007;102(1):94–104.
Carlson RG, Wang J, Falck RS, Siegal HA. Drug use practices among MDMA/ecstasy users in Ohio: a latent class analysis. Drug Alcohol Depend. 2005;79(2):167–79.
Tobin KE, Kuramoto SJ, German D, Fields E, Spikes P, Patterson J, et al. Unity in Diversity: results of a randomized clinical culturally tailored pilot HIV prevention intervention trial in Baltimore, MD, for African American men who have sex with men. Health Educ Behav. 2012;40:286.
Tobin KE, Takahashi LM, Cutchin M, Holtgrave D, Latkin C. Exploring the Social Geographies of African American Men who have Sex with Men, Baltimore, Maryland. Programs and abstracts of the National HIV Prevention Conference; August 14–17 Atlanta, GA: The National HIV Prevention Conference; 2011.
Pollack LM, Osmond DH, Paul JP, Catania JA. Evaluation of the center for disease control and prevention’s HIV behavioral surveillance of men who have sex with men: sampling issues. Sex Transm Dis. 2005;32(9):581–9.
Schwartz G. Estimating the dimension of a model. Ann Stat. 1978;6(2):461–4.
Vosburgh HW, Mansergh G, Sullivan PS, Purcell DW. A review of the literature on event-level substance use and sexual risk behavior among men who have sex with men. AIDS Behav. 2012;16:1–17.
Santos GM, Coffin PO, Das M, Matheson T, DeMicco E, Raiford JL, et al. Dose-response associations between number and frequency of substance use and high-risk sexual behaviors among HIV-negative substance-using men who have sex with men (SUMSM) in San Francisco. J Acquir Immune Defic Syndr. 2013;63(4):540–4.
Boone MR, Cook SH, Wilson P. Substance use and sexual risk behavior in HIV-positive men who have sex with men: an episode-level analysis. AIDS Behav. 2013;17(5):1883–7.
Kahler CW, Wray TB, Pantalone DW, Kruis RD, Mastroleo NR, Monti PM, et al. Daily associations between alcohol use and unprotected anal sex among heavy drinking HIV-positive men who have sex with men. AIDS Behav. 2014;19:422.
Mustanski BS, Newcomb ME, Du Bois SN, Garcia SC, Grov C. HIV in young men who have sex with men: a review of epidemiology, risk and protective factors, and interventions. J Sex Res. 2011;48(2–3):218–53.
Mustanski B. Moderating effects of age on the alcohol and sexual risk taking association: an online daily diary study of men who have sex with men. AIDS Behav. 2008;12(1):118–26.
Sexton J, Garnett G, Rottingen JA. Metaanalysis and metaregression in interpreting study variability in the impact of sexually transmitted diseases on susceptibility to HIV infection. Sex Transm Dis. 2005;32(6):351–7.
Fleming DT, Wasserheit JN. From epidemiological synergy to public health policy and practice: the contribution of other sexually transmitted diseases to sexual transmission of HIV infection. Sex Transm Infect. 1999;75(1):3–17.
Jeffries WL 4th. Beyond the bisexual bridge: sexual health among U.S. men who have sex with men and women. Am J Prev Med. 2014;47(3):320–9.
Gorbach PM, Murphy R, Weiss RE, Hucks-Ortiz C, Shoptaw S. Bridging sexual boundaries: men who have sex with men and women in a street-based sample in Los Angeles. J Urban Health. 2009;86(Suppl 1):63–76.
Tobin KE, Latkin CA. An examination of social network characteristics of men who have sex with men who use drugs. Sex Transm Infect. 2008;84(6):420–4.
Kurtz SP, Stall RD, Buttram ME, Surratt HL, Chen M. A randomized trial of a behavioral intervention for high risk substance-using MSM. AIDS Behav. 2013;17(9):2914–26.
Higa DH, Crepaz N, Marshall KJ, Kay L, Vosburgh HW, Spikes P, et al. A systematic review to identify challenges of demonstrating efficacy of HIV behavioral interventions for gay, bisexual, and other men who have sex with men (MSM). AIDS Behav. 2013;17(4):1231–44.
Morgan O, Kuramoto F, Emmet W, Stange JL, Nobunaga E. The impact of the affordable care act on behavioral health care for individuals from racial and ethnic communities. J Soc Work Disabil Rehabil. 2014;13(1–2):139–61.
Lo CC, Cheng TC. Racial/ethnic differences in access to substance abuse treatment. J Health Care Poor Underserved. 2011;22(2):621–37.
Santos GM, Coffin PO, Vittinghoff E, DeMicco E, Das M, Matheson T, et al. Substance use and drinking outcomes in personalized cognitive counseling randomized trial for episodic substance-using men who have sex with men. Drug Alcohol Depend. 2014;1(138):234–9.
Johnston LD, O’Malley PM, Miech RA, Bachman JG, Schulenberg JE. Monitoring the Future national survey results on drug use: 1975-2014: overview, key findings on adolescent drug use. Ann Arbor: Institute for Social Research, The University of Michigan; 2015.
Hensel DJ, Rosenberger JG, Novak DS, Reece M. Sexual event-level characteristics of condom use during anal intercourse among HIV-negative men who have sex with men. Sex Transm Dis. 2012;39(7):550–5.
Mimiaga MJ, Reisner SL, Cranston K, Isenberg D, Bright D, Daffin G, et al. Sexual mixing patterns and partner characteristics of black MSM in Massachusetts at increased risk for HIV infection and transmission. J Urban Health. 2009;86(4):602–23.
Adams J, Neville S. Men who have sex with men account for nonuse of condoms. Qual Health Res. 2009;19(12):1669–77.
Bauermeister JA, Carballo-Dieguez A, Ventuneac A, Dolezal C. Assessing motivations to engage in intentional condomless anal intercourse in HIV risk contexts (“Bareback Sex”) among men who have sex with men. AIDS Educ Prev. 2009;21(2):156–68.
Young SD, Shoptaw S. Stimulant use among African American and Latino MSM social networking users. J Addict Dis. 2013;32(1):39–45.
Acknowledgments
This research was supported by funding from the National Institute on Drug Abuse (1R03DA035696) and the National Institute on Alcohol Abuse and Alcoholism (R00AA020782). The authors thank Sharif Braxton for his assistance with references and manuscript preparation.
Author information
Authors and Affiliations
Corresponding author
Additional information
This work is not being considered elsewhere for publication, nor has it been previously published. This manuscript has been read and approved by all the authors.
Rights and permissions
About this article
Cite this article
Tobin, K.E., Yang, C., King, K. et al. Associations Between Drug and Alcohol Use Patterns and Sexual Risk in a Sample of African American Men Who Have Sex with Men. AIDS Behav 20, 590–599 (2016). https://doi.org/10.1007/s10461-015-1214-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-015-1214-8