Abstract
A branched vascular network is crucial to placental development and is dependent on factors such as vascular endothelial growth factor (VEGF), placental growth factor (PlGF), angiopoietin-1 (Ang-1), angiopoietin-2 (Ang-2), soluble fms-like tyrosine kinase-1 (sFlt-1) and soluble endoglin (sEng) to regulate blood vessel growth. Imbalances in these factors can lead to aberrant placental vascular development. Throughout pregnancy, these factors are also released into the maternal circulation to aid in adapting the maternal cardiovascular system to pregnancy. Increased secretion of anti-angiogenic factors can lead to the development of an anti-angiogenic state in the mother and contribute to the development of pregnancy pathologies such as pre-eclampsia and foetal growth restriction (FGR). Thus, what are commonly referred to as ‘angiogenic factors’ have distinct functions in the maternal and placental circulations making this a misnomer. Indeed, technical issues in this field such as assay methodology and lack of data considering different placental cell types mean that the physiological roles of these factors in the maternal and placental circulations are frequently muddled in the literature. This review aims to (1) unpick the distinct roles of factors that influence placental vascular development and separate these from the roles of the same factors within the maternal circulation in normal pregnancy and (2) critically assess how imbalances may contribute to the distinct pathophysiological mechanisms underlying pregnancy disorders. Together, this critical assessment of the field endeavours to improve our ability to accurately use these factors as predictive/diagnostic biomarkers in the future.



Similar content being viewed by others
References
Boyd JD, Hamilton WJ (1970) The human placenta. Heffer, Cambridge
Pereira RD, De Long NE, Wang RC, Yazdi FT, Holloway AC, Raha S (2015) Angiogenesis in the placenta: the role of reactive oxygen species signaling. Biomed Res Int 2015:814543
Alfaidy N, Hoffmann P, Boufettal H, Samouh N, Aboussaouira T, Benharouga M, Feige JJ, Brouillet S (2014) The multiple roles of EG-VEGF/PROK1 in normal and pathological placental angiogenesis. Biomed Res Int 2014:451906
Chen D, Zheng J (2014) Regulation of placental angiogenesis. Microcirculation 21:15–25
Cuffe JS, Holland O, Salomon C, Rice GE, Perkins AV (2017) Placental derived biomarkers of pregnancy disorders. Placenta 54:104–110
Maynard SE, Min JY, Merchan J, Lim KH, Li J, Mondal S, Libermann TA, Morgan JP, Sellke FW, Stillman IE, Epstein FH, Sukhatme VP, Karumanchi SA (2003) Excess placental soluble fms-like tyrosine kinase 1 (sFlt1) may contribute to endothelial dysfunction, hypertension, and proteinuria in preeclampsia. J Clin Investig 111:649–658
Brownbill P, McKeeman GC, Brockelsby JC, Crocker IP, Sibley CP (2007) Vasoactive and permeability effects of vascular endothelial growth factor-165 in the term in vitro dually perfused human placental lobule. Endocrinology 148:4734–4744
Kendall RL, Thomas KA (1993) Inhibition of vascular endothelial cell growth factor activity by an endogenously encoded soluble receptor. Proc Natl Acad Sci USA 90:10705–10709
Yáñez-Mó M, Siljander PR, Andreu Z, Bedina Zavec A, Borràs FE, Buzas EI, Buzas K, Casal E, Cappello F, Carvalho J et al (2015) Biological properties of extracellular vesicles and their physiological functions. J Extracell Vesicle 4:27066
Akercan F, Cirpan T, Terek MC, Ozcakir HT, Giray G, Sagol S, Karadadas N (2008) The immunohistochemical evaluation of VEGF in placenta biopsies of pregnancies complicated by preeclampsia. Arch Gynecol Obstet 277:109–114
Andraweera PH, Dekker GA, Roberts CT (2012) The vascular endothelial growth factor family in adverse pregnancy outcomes. Hum Reprod Update 18:436–457
Lyall F, Young A, Boswell F, Kingdom J, Greer IA (1997) Placental expression of vascular endothelial growth factor in placentae from pregnancies complicated by pre-eclampsia and intrauterine growth restriction does not support placental hypoxia at delivery. Placenta 18:269–276
Sgambati E, Marini M, Zappoli Thyrion GD, Parretti E, Mello G, Orlando C, Simi L, Tricarico C, Gheri G, Brizzi E (2004) VEGF expression in the placenta from pregnancies complicated by hypertensive disorders. BJOG 111:564–570
Sezer SD, Küçük M, Döger FK, Yüksel H, Odabaşı AR, Türkmen MK, Cakmak BÇ, Ömürlü İK, Kınaş MG (2013) VEGF, PIGF and HIF-1α in placentas of early- and late-onset pre-eclamptic patients. Gynecol Endocrinol 29:797–800
Kim S, Roh J, Park C (2016) Immunohistochemistry for pathologists: protocols, pitfalls, and tips. J Pathol Transl Med 50:411
Zhou Y, McMaster M, Woo K, Janatpour M, Perry J, Karpanen T, Alitalo K, Damsky C, Fisher SJ (2002) Vascular endothelial growth factor ligands and receptors that regulate human cytotrophoblast survival are dysregulated in severe preeclampsia and hemolysis, elevated liver enzymes, and low platelets syndrome. Am J Pathol 160:1405–1423
Cooper JC, Sharkey AM, Charnock-Jones DS, Palmer CR, Smith SK (1996) VEGF mRNA levels in placentae from pregnancies complicated by pre-eclampsia. Br J Obstet Gynaecol 103:1191–1196
Jarvenpaa J, Vuoristo JT, Savolainen E, Ukkola O, Vaskivuo T, Ryynanen M (2007) Altered expression of angiogenesis-related placental genes in pre-eclampsia associated with intrauterine growth restriction. Gynecol Endocrinol 23:351–355
Ranheim T, Cathrine Staff A, Henriksen T (2001) VEGF mRNA is unaltered in decidual and placental tissues in preeclampsia at delivery. Acta Obstet Gynecol Scand 80:93–98
Soker S, Svahn CM, Neufeld G (1993) Vascular endothelial growth factor is inactivated by binding to alpha 2-macroglobulin and the binding is inhibited by heparin. J Biol Chem 268:7685–7691
Witzenbichler B, Maisonpierre PC, Jones P, Yancopoulos GD, Isner JM (1998) Chemotactic properties of angiopoietin-1 and-2, ligands for the endothelial-specific receptor tyrosine kinase Tie2. J Biol Chem 273:18514–18521
Ferrara N, Davis-Smyth T (1997) The biology of vascular endothelial growth factor. Endocr Rev 18:4–25
Gordijn SJ, Beune IM, Thilaganathan B, Papageorghiou A, Baschat AA, Baker PN, Silver RM, Wynia K, Ganzevoort W (2016) Consensus definition of fetal growth restriction: a Delphi procedure. Ultrasound Obstet Gynecol 48:333–339. https://doi.org/10.1002/uog.15884
Arroyo JA, Winn VD (2008) Vasculogenesis and angiogenesis in the IUGR placenta. Semin Perinatol 32:172–177
Rigano S, Bozzo M, Ferrazzi E, Bellotti M, Battaglia FC, Galan HL (2001) Early and persistent reduction in umbilical vein blood flow in the growth-restricted fetus: a longitudinal study. Obstet Gynecol 185:834–838
Burton GJ, Woods AW, Jauniaux E, Kingdom J (2009) Rheological and physiological consequences of conversion of the maternal spiral arteries for uteroplacental blood flow during human pregnancy. Placenta 30:473–482
Glazier JD, Cetin I, Perugino G, Ronzoni S, Grey AM, Mahendran D, Marconi AM, Pardi G, Sibley CP (1997) Association between the activity of the system A amino acid transporter in the microvillous plasma membrane of the human placenta and severity of fetal compromise in intrauterine growth restriction. Pediatr Res 42:514–519
Jansson T, Scholtbach V, Powell TL (1998) Placental transport of leucine and lysine is reduced in intrauterine growth restriction. Pediatr Res 44:532–537
Krebs C, Macara LM, Leiser R, Bowman AW, Greer IA, Kingdom JC (1996) Intrauterine growth restriction with absent end-diastolic flow velocity in the umbilical artery is associated with maldevelopment of the placental terminal villous tree. Obstet Gynecol 175:1534–1542
Zygmunt M, Herr F, Münstedt K, Lang U, Liang OD (2003) Angiogenesis and vasculogenesis in pregnancy. Eur J Obstet Gynecol Reprod Biol 110:S1–S18
Roex A, Nikpoor P, van Eerd E, Hodyl N, Dekker G (2012) Serial plotting on customised fundal height charts results in doubling of the antenatal detection of small for gestational age fetuses in nulliparous women. Aust NZ J Obstet Gynecol 52:78–82
Gardosi J, Madurasinghe V, Williams M, Malik A, Francis A (2013) Maternal and fetal risk factors for stillbirth: population based study. BMJ 346:f108
Lowe SA, Bowyer L, Lust K, McMahon LP, Morton M, North RA, Paech M, Said JM (2015) SOMANZ guidelines for the management of hypertensive disorders of pregnancy 2014. Aust NZ J Obstet Gynecol. https://doi.org/10.1111/ajo.12399
Raymond D, Peterson E (2011) A critical review of early-onset and late-onset preeclampsia. Obstet Gynecol Surv 66:497–506
Crovetto F, Crispi F, Scazzocchio E, Mercade I, Meler E, Figueras F, Gratacos E (2014) First-trimester screening for early and late small-for-gestational-age neonates using maternal serum biochemistry, blood pressure and uterine artery Doppler. Ultrasound Obstet Gynecol 43:34–40
Wang A, Rana S, Karumanchi SA (2009) Preeclampsia: the role of angiogenic factors in its pathogenesis. Physiology (Bethesda) 24:147–158
Meekins JW, Pijnenborg R, Hanssens M, McFadyen IR, van Asshe A (1994) A study of placental bed spiral arteries and trophoblast invasion in normal and severe pre-eclamptic pregnancies. Br J Obstet Gynaecol 101:669–674
Lau SY, Guild S, Barrett CJ, Chen Q, McCowan L, Jordan V, Chamley LW (2013) Tumor necrosis factor-alpha, interleukin-6, and interleukin-10 levels are altered in preeclampsia: a systematic review and meta-analysis. Am J Reprod Immunol 70:412–427
Egbor M, Ansari T, Morris N, Green CJ, Sibbons PD (2006) Maternal medicine: morphometric placental villous and vascular abnormalities in early- and late-onset pre-eclampsia with and without fetal growth restriction. BJOG 113:580–589. https://doi.org/10.1111/j.1471-0528.2006.00882.x
Mayhew TM, Wijesekara J, Baker PN, Ong SS (2004) Morphometric evidence that villous development and fetoplacental angiogenesis are compromised by intrauterine growth restriction but not by pre-eclampsia. Placenta 25:829–833
Eastwood K, Hunter AJ, Patterson CC, Mc Cance DR, Young IS, Holmes VA (2018) Placental vascularization indices and prediction of pre-eclampsia in high-risk women. Placenta 70:53–59
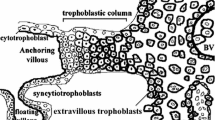
Reynolds LP, Redmer DA (2001) Angiogenesis in the placenta. Biol Reprod 64:1033–1040
Mihu CM, Suşman S, Ciucă DR, Mihu D, Costin N (2009) Aspects of placental morphogenesis and angiogenesis. Rom J Morphol Embryol 50:549–557
Kaufmann P, Mayhew TM, Charnock-Jones DS (2004) Aspects of human fetoplacental vasculogenesis and angiogenesis. II. Changes during normal pregnancy. Placenta 25:114–126
Regnault T, Galan HL, Parker TA, Anthony RV (2002) Placental development in normal and compromised pregnancies—a review. Placenta 23:S119–S129
Wang Y (2010) Vascular biology of the placenta. In Colloquium series on integrated systems physiology: from molecule to function. Morgan & Claypool Life Sci 2:1–98
Tseng JJ, Chou MM, Hsieh YT, Wen MC, Ho ES, Hsu SL (2006) Differential expression of vascular endothelial growth factor, placenta growth factor and their receptors in placentae from pregnancies complicated by placenta accreta. Placenta 27:70–78
Ahmad S, Ahmed A (2004) Elevated placental soluble vascular endothelial growth factor receptor-1 inhibits angiogenesis in preeclampsia. Circ Res 95:884–891
Erez O, Romero R, Espinoza J, Fu W, Todem D, Kusanovic JP, Gotsch F, Edwin S, Nien JK, Chaiworapongsa T (2008) The change in concentrations of angiogenic and anti-angiogenic factors in maternal plasma between the first and second trimesters in risk assessment for the subsequent development of preeclampsia and small-for-gestational age. J Matern Fetal Neonatal Med 21:279–287
Kusanovic JP, Romero R, Chaiworapongsa T, Erez O, Mittal P, Vaisbuch E, Mazaki-Tovi S, Gotsch F, Edwin SS, Gomez R (2009) A prospective cohort study of the value of maternal plasma concentrations of angiogenic and anti-angiogenic factors in early pregnancy and midtrimester in the identification of patients destined to develop preeclampsia. J Matern Fetal Neonatal Med 22:1021–1038
Levine RJ, Maynard SE, Qian C, Lim K, England LJ, Yu KF, Schisterman EF, Thadhani R, Sachs BP, Epstein FH (2004) Circulating angiogenic factors and the risk of preeclampsia. N Engl J Med 350:672–683
Lim JH, Kim SY, Park SY, Yang JH, Kim MY, Ryu HM (2008) Effective prediction of preeclampsia by a combined ratio of angiogenesis-related factors. Obstset Gynecol 111:1403–1409
Hoeller A, Ehrlich L, Golic M, Herse F, Perschel FH, Siwetz M, Henrich W, Dechend R, Huppertz B, Verlohren S (2017) Placental expression of sFlt-1 and PlGF in early preeclampsia vs. early IUGR vs. age-matched healthy pregnancies. Hypertens Pregnancy 36:151–160
Shibata E, Rajakumar A, Powers RW, Larkin RW, Gilmour C, Bodnar LM, Crombleholme WR, Ness RB, Roberts JM, Hubel CA (2005) Soluble fms-like tyrosine kinase 1 is increased in preeclampsia but not in normotensive pregnancies with small-for-gestational-age neonates: relationship to circulating placental growth factor. J Clin Endocrinol Metab 90:4895–4903
Khalil A, Muttukrishna S, Harrington K, Jauniaux E (2008) Effect of antihypertensive therapy with alpha methyldopa on levels of angiogenic factors in pregnancies with hypertensive disorders. PLoS ONE 3:e2766
Ferrara N (2004) Vascular endothelial growth factor: basic science and clinical progress. Endocr Rev 25:581–611
Barut F, Barut A, Gun BD, Kandemir NO, Harma MI, Harma M, Aktunc E, Ozdamar SO (2010) Intrauterine growth restriction and placental angiogenesis. Diagn Pathol 5:24
Bates DO, MacMillan PP, Manjaly JG, Qiu Y, Hudson SJ, Bevan HS, Hunter AJ, Soothill PW, Read M, Donaldson LF (2006) The endogenous anti-angiogenic family of splice variants of VEGF, VEGFxxxb, are down-regulated in pre-eclamptic placentae at term. Clin Sci 110:575–585
Geva E, Ginzinger DG, Zaloudek CJ, Moore DH, Byrne A, Jaffe RB (2002) Human placental vascular development: vasculogenic and angiogenic (branching and nonbranching) transformation is regulated by vascular endothelial growth factor-A, angiopoietin-1, and angiopoietin-2. J Clin Endocrinol Metab 87:4213–4224
Dunk C, Shams M, Nijjar S, Rhaman M, Qiu Y, Bussolati B, Ahmed A (2000) Angiopoietin-1 and angiopoietin-2 activate trophoblast Tie-2 to promote growth and migration during placental development. Am J Pathol 156:2185–2199
Kappou D, Sifakis S, Androutsopoulos V, Konstantinidou A, Spandidos DA, Papantoniou N (2014) Placental mRNA expression of angiopoietins (Ang)-1, Ang-2 and their receptor Tie-2 is altered in pregnancies complicated by preeclampsia. Placenta 35:718–723
Lobov IB, Brooks PC, Lang RA (2002) Angiopoietin-2 displays VEGF-dependent modulation of capillary structure and endothelial cell survival in vivo. Proc Natl Acad Sci USA 99:11205–11210
Whitley GS, Dash P, Ayling LJ, Prefumo F, Thilaganathan B, Cartwright JE (2007) Increased apoptosis in first trimester extravillous trophoblasts from pregnancies at higher risk of developing preeclampsia. Am J Pathol 170:1903–1909
Charolidi N, Host AJ, Ashton S, Tryfonos Z, Leslie K, Thilaganathan B, Cartwright JE, Whitley GS (2018) First trimester placental endothelial cells from pregnancies with abnormal uterine artery Doppler are more sensitive to apoptotic stimuli. Lab Investig 99:411–420
Chappell JC, Taylor SM, Ferrara N, Bautch VL (2009) Local guidance of emerging vessel sprouts requires soluble Flt-1. Dev Cell 17:377–386
Kumasawa K, Ikawa M, Kidoya H, Hasuwa H, Saito-Fujita T, Morioka Y, Takakura N, Kimura T, Okabe M (2011) Pravastatin induces placental growth factor (PGF) and ameliorates preeclampsia in a mouse model. Proc Natl Acad Sci USA 108:1451–1455
Nikuei P, Rajaei M, Malekzadeh K, Nejatizadeh A, Mohseni F, Poordarvishi F (2017) Expression of placental growth factor mRNA in preeclampsia. Int J Reprod Biomed (Yazd) 15:169
Record M (2014) Intercellular communication by exosomes in placenta: a possible role in cell fusion? Placenta 35:297–302
Boeldt DS, Bird IM (2017) Vascular adaptation in pregnancy and endothelial dysfunction in preeclampsia. J Endocrinol 232:R27
Tsiakkas A, Duvdevani N, Wright A, Wright D, Nicolaides KH (2015) Serum soluble fms-like tyrosine kinase-1 in the three trimesters of pregnancy: effects of maternal characteristics and medical history. Ultrasound Obstet Gynecol 45:584–590
Pang L, Wei Z, Li O, Huang R, Qin J, Chen H, Fan X, Chen Z (2013) An increase in vascular endothelial growth factor (VEGF) and VEGF soluble receptor-1 (sFlt-1) are associated with early recurrent spontaneous abortion. PLoS ONE 8:e75759
Tandon V, Hiwale S, Amle D, Nagaria T, Patra PK (2017) Assessment of serum vascular endothelial growth factor levels in pregnancy-induced hypertension patients. J Pregnancy. https://doi.org/10.1155/2017/3179670
Nadar SK, Karalis I, Al Yemeni E, Blann AD, Lip GY (2005) Plasma markers of angiogenesis in pregnancy induced hypertension. Thromb Haemost 94:1071–1076
El-Sokkary MS, El-Refaie TA, Mostafa NBH, Elaassar MMS (2017) Maternal serum vascular endothelial growth factor in patients with preeclampsia. Egypt J Hosp Med 69:1634–1640
Saffer C, Olson G, Boggess KA, Beyerlein R, Eubank C, Sibai BM, NORMALS Study Group (2013) Determination of placental growth factor (PlGF) levels in healthy pregnant women without signs or symptoms of preeclampsia. Pregnancy Hypertens 3:124–132
De Vivo A, Baviera G, Giordano D, Todarello G, Corrado F, D’anna R (2008) Endoglin, PlGF and sFlt-1 as markers for predicting pre-eclampsia. Acta Obstet Gynecol Scand 87:837–842
Crispi F, Llurba E, Dominguez C, Martín-Gallán P, Cabero L, Gratacos E (2008) Predictive value of angiogenic factors and uterine artery Doppler for early- versus late-onset pre-eclampsia and intrauterine growth restriction. Ultrasound Obstet Gynecol 31:303–309
Kim S, Ryu H, Yang J, Kim M, Han J, Kim J, Chung J, Park S, Lee M, Kim D (2007) Increased sFlt-1 to PlGF ratio in women who subsequently develop preeclampsia. J Korean Med Sci 22:873–877
Tsatsaris V, Goffin F, Munaut C, Brichant J, Pignon M, Noel A, Schaaps J, Cabrol D, Frankenne F, Foidart J (2003) Overexpression of the soluble vascular endothelial growth factor receptor in preeclamptic patients: pathophysiological consequences. J Clin Endocrinol Metab 88:5555–5563
Leinonen E, Wathén K, Alfthan H, Ylikorkala O, Andersson S, Stenman U, Vuorela P (2010) Maternal serum angiopoietin-1 and -2 and tie-2 in early pregnancy ending in preeclampsia or intrauterine growth retardation. J Clin Endocrinol Metab 95:126–133
Lai J, Syngelaki A, Poon LC, Nucci M, Nicolaides KH (2013) Maternal serum soluble endoglin at 30-33 weeks in the prediction of preeclampsia. Fetal Diagn Ther 33:149–155
Chaiworapongsa T, Romero R, Kusanovic JP, Mittal P, Kim SK, Gotsch F, Than NG, Mazaki-Tovi S, Vaisbuch E, Erez O (2010) Plasma soluble endoglin concentration in pre-eclampsia is associated with an increased impedance to flow in the maternal and fetal circulations. Ultrasound Obstet Gynecol 35:155–162
Nanjo S, Minami S, Mizoguchi M, Yamamoto M, Yahata T, Toujima S, Shiro M, Kobayashi A, Muragaki Y, Ino K (2017) Levels of serum-circulating angiogenic factors within 1 week prior to delivery are closely related to conditions of pregnant women with pre-eclampsia, gestational hypertension, and/or fetal growth restriction. J Obstet Gynaecol Res 43:1805–1814
Esser S, Wolburg K, Wolburg H, Breier G, Kurzchalia T, Risau W (1998) Vascular endothelial growth factor induces endothelial fenestrations in vitro. J Cell Biol 140:947–959
Roberts JM, Rajakumar A (2009) Preeclampsia and soluble fms-like tyrosine kinase 1. J Clin Endocrinol Metab 94(7):2252–2254
McAllister KA, Lennon F, Bowles-Biesecker B, McKinnon WC, Helmbold EA, Markel DS, Jackson CE, Guttmacher AE, Pericak-Vance MA, Marchuk DA (1994) Genetic heterogeneity in hereditary haemorrhagic telangiectasia: possible correlation with clinical phenotype. J Med Genet 31:927–932
Sela S, Itin A, Natanson-Yaron S, Greenfield C, Goldman-Wohl D, Yagel S, Keshet E (2008) A novel human-specific soluble vascular endothelial growth factor receptor 1: cell type-specific splicing and implications to vascular endothelial growth factor homeostasis and preeclampsia. Circ Res 102:1566–1574
Eremina V, Sood M, Haigh J, Nagy A, Lajoie G, Ferrara N, Gerber H, Kikkawa Y, Miner JH, Quaggin SE (2003) Glomerular-specific alterations of VEGF-A expression lead to distinct congenital and acquired renal diseases. J Clin Investig 111:707–716
Bills VL, Salmon AH, Harper SJ, Overton TG, Neal CR, Jeffery B, Soothill PW, Bates DO (2011) Impaired vascular permeability regulation caused by the VEGF165b splice variant in pre-eclampsia. BJOG 118:1253–1261
Baker PN, Davidge ST, Barankiewicz J, Roberts JM (1996) Plasma of preeclamptic women stimulates and then inhibits endothelial prostacyclin. Hypertension 27:56–61
Toporsian M, Gros R, Kabir MG, Vera S, Govindaraju K, Eidelman DH, Husain M, Letarte M (2005) A role for endoglin in coupling eNOS activity and regulating vascular tone revealed in hereditary hemorrhagic telangiectasia. Circ Res 96:684–692
Venkatesha S, Toporsian M, Lam C, Hanai J, Mammoto T, Kim YM, Bdolah Y, Lim K, Yuan H, Libermann TA (2006) Soluble endoglin contributes to the pathogenesis of preeclampsia. Nat Med 12:642
Voron T, Marcheteau E, Pernot S, Colussi O, Tartour E, Taieb J, Terme M (2014) Control of the immune response by pro-angiogenic factors. Front Oncol 4:70
Takahashi A, Kono K, Ichihara F, Sugai H, Fujii H, Matsumoto Y (2004) Vascular endothelial growth factor inhibits maturation of dendritic cells induced by lipopolysaccharide, but not by proinflammatory cytokines. Cancer Immunol Immunother 53:543–550
Shojaei F, Wu X, Zhong C, Yu L, Liang X, Yao J, Blanchard D, Bais C, Peale FV, Van Bruggen N (2007) Bv8 regulates myeloid-cell-dependent tumour angiogenesis. Nature 450:825
Rana S, Schnettler WT, Powe C, Wenger J, Salahuddin S, Cerdeira AS, Verlohren S, Perschel FH, Arany Z, Lim K (2013) Clinical characterization and outcomes of preeclampsia with normal angiogenic profile. Hypertens Pregnancy 32:189–201
Szukiewicz D, Szewczyk G, Watroba M, Kurowska E, Maslinski S (2005) Isolated placental vessel response to vascular endothelial growth factor and placenta growth factor in normal and growth-restricted pregnancy. Gynecol Obstet Investig 59:102–107
Hirokoshi K, Maeshima Y, Kobayashi K, Matsuura E, Sugiyama H, Yamasaki Y, Masuyama H, Hiramatsu Y, Makino H (2005) Increase of serum angiopoietin-2 during pregnancy is suppressed in women with preeclampsia. Am J Hypertens 18:1181–1188
Baffert F, Thurston G, Rochon-Duck M, Le T, Brekken R, McDonald DM (2004) Age-related changes in vascular endothelial growth factor dependency and angiopoietin-1-induced plasticity of adult blood vessels. Circ Res 94:984–992
Thurston G, Wang Q, Baffert F, Rudge J, Papadopoulos N, Jean-Guillaume D, Wiegand S, Yancopoulos GD, McDonald DM (2005) Angiopoietin 1 causes vessel enlargement, without angiogenic sprouting, during a critical developmental period. Development 132:3317–3326
Thurston G, Suri C, Smith K, McClain J, Sato TN, Yancopoulos GD, McDonald DM (1999) Leakage-resistant blood vessels in mice transgenically overexpressing angiopoietin-1. Science 286:2511–2514
Kim I, Kim J, Ryu YS, Liu M, Koh GY (2000) Tumor necrosis factor-α upregulates angiopoietin-2 in human umbilical vein endothelial cells. Biochem Biophys Res Commun 269:361–365
Wang Y, Tasevski V, Wallace EM, Gallery ED, Morris JM (2007) Reduced maternal serum concentrations of angiopoietin-2 in the first trimester precede intrauterine growth restriction associated with placental insufficiency. BJOG 114:1427–1431
Hanahan D, Folkman J (1996) Patterns and emerging mechanisms of the angiogenic switch during tumorigenesis. Cell 86:353–364
Nasu K, Fujisawa K, Nishida Y, Kai S, Sugano T, Miyakawa I, Tateishi Y (2003) Expression of collagen XVIII mRNA and protein in human umbilical vein and placenta. Reprod Fertil Dev 15:107–114
Yamaguchi N, Anand-Apte B, Lee M, Sasaki T, Fukai N, Shapiro R, Que I, Lowik C, Timpl R, Olsen BR (1999) Endostatin inhibits VEGF-induced endothelial cell migration and tumor growth independently of zinc binding. EMBO J 18:4414–4423
Hirtenlehner K, Pollheimer J, Lichtenberger C, Wolschek MF, Zeisler H, Husslein P, Knöfler M (2003) Elevated serum concentrations of the angiogenesis inhibitor endostatin in preeclamptic women. J Soc Gynecol Investig 10:412–417
Wikström A, Larsson A, Åkerud H, Olovsson M (2009) Increased circulating levels of the antiangiogenic factor endostatin in early-onset but not late-onset preeclampsia. Reprod Sci 16:995–1000
Conde-Agudelo A, Papageorghiou AT, Kennedy SH, Villar J (2013) Novel biomarkers for predicting intrauterine growth restriction: a systematic review and meta-analysis. BJOG 120:681–694
Agrawal S, Cerdeira AS, Redman C, Vatish M (2017) Meta-analysis and systematic review to assess the role of soluble FMS-like tyrosine kinase-1 and placenta growth factor ratio in prediction of preeclampsia: the SaPPPhirE study. Hypertension 71:306–316
Alahakoon TI, Zhang W, Trudinger BJ, Lee VW (2014) Discordant clinical presentations of preeclampsia and intrauterine fetal growth restriction with similar pro- and anti-angiogenic profiles. J Matern Fetal Neonatal Med 27:1854–1859
Verlohren S, Herraiz I, Lapaire O, Schlembach D, Zeisler H, Calda P, Sabria J, Markfeld-Erol F, Galindo A, Schoofs K (2014) New gestational phase-specific cutoff values for the use of the soluble fms-like tyrosine kinase-1/placental growth factor ratio as a diagnostic test for preeclampsia. Hypertension 63:346–352
Akolekar R, Syngelaki A, Sarquis R, Zvanca M, Nicolaides KH (2011) Prediction of early, intermediate and late pre-eclampsia from maternal factors, biophysical and biochemical markers at 11–13 weeks. Prenat Diagn 31:66–74
Sovio U, Gaccioli F, Hund M, Charnock-Jones DS, Smith GC (2017) 155: Screening for late fetal growth restriction using ultrasound and the sFlt-1:PlGF ratio. AJOG 216:S104
Li Z, Zhang Y, Ying Ma J, Kapoun AM, Shao Q, Kerr I, Lam A, O’Young G, Sannajust F, Stathis P (2007) Recombinant vascular endothelial growth factor 121 attenuates hypertension and improves kidney damage in a rat model of preeclampsia. Hypertension 50:686–692
Gilbert JS, Verzwyvelt J, Colson D, Arany M, Karumanchi SA, Granger JP (2010) Recombinant vascular endothelial growth factor 121 infusion lowers blood pressure and improves renal function in rats with placentalischemia-induced hypertension. Hypertension 55:380–385
Carr DJ, Wallace JM, Aitken RP, Milne JS, Martin JF, Zachary IC, Peebles DM, David AL (2016) Peri- and postnatal effects of prenatal adenoviral VEGF gene therapy in growth-restricted sheep. Biol Reprod 94:142
Carr DJ, Wallace JM, Aitken RP, Milne JS, Mehta V, Martin JF, Zachary IC, Peebles DM, David AL (2014) Uteroplacental adenovirus vascular endothelial growth factor gene therapy increases fetal growth velocity in growth-restricted sheep pregnancies. Hum Gene Ther 25:375–384
Vaughan OR, Rossi CA, Ginsberg Y, White A, Hristova M, Sebire NJ, Martin J, Zachary IC, Peebles DM, David AL (2018) Perinatal and long-term effects of maternal uterine artery adenoviral VEGF-A165 gene therapy in the growth-restricted guinea pig fetus. Am J Physiol Regul Integr Comp Physiol 315:R344–R353
Spencer R, Ambler G, Brodszki J, Diemert A, Figueras F, Gratacós E, Hansson SR, Hecher K, Huertas-Ceballos A, Marlow N (2017) EVERREST prospective study: a 6-year prospective study to define the clinical and biological characteristics of pregnancies affected by severe early onset fetal growth restriction. BMC Pregnancy Childbirth 17:43
Funding
This study was funded by the University of Auckland Doctoral Scholarship to Anandita Umapathy and the Health Research Council Sir Charles Hercus Research Fellowship to Joanna L. James (Grant Number 16/043).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Umapathy, A., Chamley, L.W. & James, J.L. Reconciling the distinct roles of angiogenic/anti-angiogenic factors in the placenta and maternal circulation of normal and pathological pregnancies. Angiogenesis 23, 105–117 (2020). https://doi.org/10.1007/s10456-019-09694-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10456-019-09694-w